Abstract
Background
The Lichtenstein technique is the treatment of first choice according to guidelines for primary inguinal hernia treatment. Postoperative chronic pain has been reported as complication in 15–40 % after Lichtenstein’s repair. The postoperative effects on health status after open preperitoneal hernia repair have hardly been examined. Development of an open technique that combines the safe anterior approach of the Lichtenstein with the ‘promising’ preperitoneal soft mesh position was done; the transinguinal preperitoneal (TIPP) mesh repair. A double-blind prospective randomized controlled trial (TULIP trial, ISRCTN93798494) was conducted to compare different outcome parameters after TIPP or Lichtenstein, one parameter is topic of evaluation in this paper; the health status after TIPP and Lichtenstein for inguinal hernia repair.
Methods
The study protocol has been published. It was hypothesized that the health status of inguinal hernia patients would be better after the TIPP repair compared with the Lichtenstein technique. The size of this study was based on chronic pain as primary outcome measure. Three hundred and two patients were randomized. Patients and the outcome assessors were blinded. Follow-up was scheduled after 14 days, 3 months, and 1 year. The three dimensions of possible errors were warranted.
Results
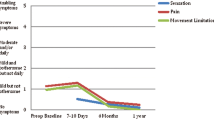
With regard to health status, significant differences were found in the dimensions ‘physical pain’ [difference: 6.1 (95 % CI 2.3–9.9, p = 0.002)] and ‘physical functioning’ [difference: 3.5 (95 % CI 0.5–6.7, p = 0.023)], favoring the TIPP patients after 1 year.
Conclusion
In conclusion, the SF-36 ‘physical function’ and ‘physical pain’ dimensions after TIPP show significant better patient outcomes at 1 year compared with the Lichtenstein patients in this trial. These differences are in line with reported significant differences in less patients with postoperative chronic pain after TIPP compared with Lichtenstein at 1 year.


Similar content being viewed by others
References
Source (2009) Statline, Centraal Bureau voor de Statistiek (http://statline.cbs.nl/statweb)
Official Dutch Inguinal Hernia Guideline (NVvH) (2003) ISBN 90-8523-001-2 (http://www.heelkunde.nl/uploads/xt/UD/xtUDdTOMwNlhcxalg-WJHQ/Richtlijnliesbreuk.pdf)
Simons MP, de Lange D, Beets GL, van Geldere D, Heij HA, Go PM (2003) The ‘inguinal hernia’ guideline of the association of surgeons of the Netherlands. Ned Tijdschr Geneesk 147:2111–2117
McCormack K, Scott N, Go PM, Ross SJ, Grant A (2008) Collaboration the EU Hernia Trialists. The Cochrane Collaboration and published in The Cochrane Library, Issue, Laparoscopic techniques versus open techniques for inguinal hernia repair 4
Bay-Nielsen M, Perkins FM, Kehlet H (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 233:1–7
Poobalan AS, Bruce J, Smith WC, King PM, Krukowski ZH, Chambers WA (2001) Chronic pain and quality of life following open inguinal hernia repair. Br J Surg 88:6–1122
Hair A, Duffy K, Mclean J, Taylor S, Smith H, Walker A et al (2000) Groin hernia repair in Scotland. Br J Surg 87:1722–1726
Bay-Nielsen M, Nilsson E, Nordin P, Kehlet H (2004) Chronic pain after open mesh and sutured repair of indirect hernia in young males. Br J Surg 91:1372–1376
Koning GG, Koole D, de Jongh MAC, de Schipper JP, Verhofstad MHJ, Oostvogel HJM, Vriens PWHE (2011) The transinguinal preperitoneal hernia correction vs Lichtenstein's technique; is TIPP top? Hernia 15(1):19–22
Langeveld HR, van’t Riet M, Weidema WF, Stassen LPS, Steyerberg EW, Lange J, Bonjer HJ, Jeekel J (2010) Total extraperitoneal inguinal hernia repair compared with Lichtenstein (the LEVEL-Trial). A randomized controlled trial. Ann Surg 251:819–824
Lawrence K, Jenkinson C, McWhinnie D, Coulter A (1997) Quality of life in patients undergoing inguinal hernia repair. Ann R Coll Surg Engl 79:40–45
Koning GG, Wetterslev J, van Laarhoven CJHM, Keus F (2011) PROTOCOL for: the totally extraperitoneal—(TEP) versus Lichtenstein's technique for inguinal hernia repair; a systematic review. www.ctu.dk/protocols
Koning GG, Wetterslev J, van Laarhoven CJHM, Keus F (2011). The totally extraperitoneal—(TEP) versus Lichtenstein’s technique for inguinal hernia repair; a systematic review of clinical trials Submitted to PLoS ONE Journal
Pélissier EP, Blum D, Marre D, Damas JM (2001) Inguinal hernia: a patch covering only the myopectineal orifice is effective. Hernia 5:84–87
Pélissier EP (2006) Inguinal hernia: preperitoneal placement of a memory-ring patch by anterior approach. Preliminary experience. Hernia 10:248–252
Berrevoet F, Maes L, Reyntjens K, Rogiers X, Troisi R, de Hemptinne B (2010) Transinguinal preperitoneal memory ring patch versus Lichtenstein repair for unilateral inguinal hernias. Lang Arch Surg 395(5):557–562
Koning GG, de Schipper HJ, Oostvogel HJM, Verhofstad MHJ, van Laarhoven CJHM, Vriens PWHE (2009) The Tilburg double blind randomized controlled trial comparing inguinal hernia repair according to Lichtenstein and the transinguinal preperitoneal technique. Trials. doi:10.1186/1745-6215-10-89
Nienhuijs SW, van Oort I, Keemers-Gels MEL, Strobbe JA, Rosman C (2005) Randomized clinical trial comparing the prolene hernia system, mesh plug repair and lichtenstein method for open inguinal hernia repair. Br J Surg 92:33–38
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R, Sprangers MA, te Velde A, Verrips E (1998) Translation, validation and norming of the dutch language version of the sf-36 health survey in community and chronic disease populations. J Clin Epidemiol 51:1055–1068
Brazier JE, Harper R, Jones NMB, O’Cathain A, Thomas KJ, Usherwood T (1992) Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 305:160–164
Ware JE, Snow KK, Kosinski M, Gandek B (1993) The SF36 health survey manual and interpretation guide. Health Institute, New England Medical Centre, Boston
McHoraey CA, Ware JE, Raczek AE (1993) The MOS 36-item health survey (SF-36). Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 31:247–263
Jenkinson C, Coulter A, Wright L (1993) Short form 36 (SF36) health survey questionnaire. Normative data for adults of working age. Br Med J 306:1437–1440
Amid PK, Shulman AG, Lichtenstein IL (1996) Open “tension-free” repair of inguinal hernias: the Lichtenstein technique. Eur J Surg 162:447–453
Koch A, Bringman S, Myrelid P, Smeds S, Kald A (2008) Randomized clinical trial of groin hernia repair with titanium-coated lightweight mesh compared with standard polypropylene mesh. Br J Surg 95:1226–1231
Koning GG, Keus F, Koeslag L, Cheung CL, Avci M, van Laarhoven CJHM, Vriens PWHE (2012) Randomised clinical trial on chronic pain after the transinguinal preperitoneal technique compared to Lichtenstein’s method for inguinal hernia repair. Accepted for publication in Br J Surg 2012
Higgins JPT, Green S (2008) Cochrane handbook for systematic reviews of interventions. The cochrane collaboration
Miserez M, Alexandre JH, Campanelli G, Corcione F (2007) The European hernia society groin hernia classification: simple and easy to remember. Hernia 11:113–116
Schulz KF, Altman DG, Moher D, CONSORT Group (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. PLoS Med 7(3):e1000251. doi:10.1371/journal.pmed.1000251
Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ (2008) GRADE working group: what is “quality of evidence” and why is it important to clinicians? BMJ 336:995–998
Katherine EM, Browne M, Kavanagh DO, Hurley M (2010) Laparoscopic (TEP) versus lichtenstein inguinal hernia repair: a comparison of quality-of-life outcomes. World J Surg 34:3059–3064
Barrat C, Seriser F, Arnoud R, Trouette P, Champault G (2004) Inguinal hernia repair with beta glucan-coated mesh: prospective multicenter study (115 cases)—preliminary results. Hernia 8:33–38
Keus F, Wetterslev J, Gluud C, van Laarhoven CJHM (2010) Evidence at a glance: error matrix approach for overviewing available evidence. BMC Med Res Meth 10:90
Keus F, Wetterslev J, Gluud C, Gooszen HG, van Laarhoven CJHM (2010) Trial sequential analyses of meta-analyses of complications in laparoscopic vs. small-incision cholecystectomy: more randomized patients are needed. J Clin Epidemiol 63:246–256
Acknowledgments
For participating, facilitating and contributing to the TULIP trial to: R. van Doorn, M.S. Ibelings, G.P. Gerritsen, J. Heisterkamp, H.J.M. Oostvogel, M.H.J. Verhofstad, J.A. Roukema, J. van Breda, M. Avci, C.L. Cheung, E. Wolters - van Loon, A. Gillis, F. Keus, and T. Hendriks. The authors would like to thank all the surgical residents, OPD- and ward nurses, of the St. Elisabeth Hospital, and TweeSteden Hospital in Tilburg and in Waalwijk, the Netherlands. The authors would also like to thank W. Lemmens (Dept. of Epidemiology, Biostatistics and Health Technology Assessment, Radboud University Nijmegen) for his statistical calculations and support.
Conflicts of interest
None. No industry funding, nor meshes free of charge, nor discounts.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koning, G.G., de Vries, J., Borm, G.F. et al. Health status one year after TransInguinal PrePeritoneal inguinal hernia repair and Lichtenstein’s method: an analysis alongside a randomized clinical study. Hernia 17, 299–306 (2013). https://doi.org/10.1007/s10029-012-0963-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-012-0963-9