Abstract
Objective
The standard opioid treatment for postoperative pain can be associated with nausea, vomiting, and constipation. In addition, opioids often provide insufficient pain relief. The purpose of this study was to compare postoperative pain and functional outcomes in patients undergoing inguinal herniorrhaphy who receive a COX-2 selective nonsteroidal anti-inflammatory drug (COX-2) or placebo preoperatively and for 4 days postoperatively.
Methods
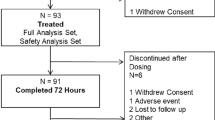
A prospective, randomized, blinded, placebo-controlled trial was conducted in adults undergoing elective, outpatient, unilateral inguinal herniorrhaphy. Patients received rofecoxib (50 mg, 1 h prior to incision) or placebo. Doses were re-administered once daily on postoperative days 1–4. Patients were also given hydrocodone bitartrate for use as needed in the postoperative period. Pain outcomes were assessed, including pain intensity (1–10 visual-analogue scale) and the use of hydrocodone bitartrate. In addition, functional outcomes such as activity and return of bowel function were examined for 5 postoperative days. Incidence and severity of side effects were examined. Statistics are mean ± standard deviation.
Results
Fifty-five subjects completed the study. Twenty-six patients received rofecoxib and 29 patients received placebo. Patients who received COX-2 demonstrated improved bowel function as reflected by more bowel movements on postoperative day 2 and postoperative day 3. COX-2-treated patients also reported better oral intake on these same days. In addition, COX-2-treated patients had less difficulty coughing on postoperative day 1. Overall satisfaction with pain management was better in COX-2-treated patients (very satisfied vs. satisfied). There were no statistically significant differences between groups in the amount of hydrocodone bitartrate consumption. There were no complications during the study period.
Conclusions
Administration of a COX-2 selective nonsteroidal anti-inflammatory drug prior to and following outpatient inguinal herniorrhaphy improves functional outcomes when compared with placebo and increases patient satisfaction. These results suggest that multimodal pain therapy with COX-2 inhibitors may have a role in outpatient inguinal hernia repair.





Similar content being viewed by others
References
Kehlet H (1997) Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 78:606–617
Carr DB (1998) Preempting the memory of pain. JAMA 279:1114–1115
Agency for Health Care Policy and Research (1992) Acute pain management: operative or medical procedures and trauma, clinical practice guideline no. 1. AHCPR publication 92-0032. US Public Health Service, Agency for Health Care Policy and Research, US Department of Health and Human Services, Rockville, MD
American Society of Anesthesiologists Task Force on Pain Management, Acute Pain Section (1995) Practice guidelines for acute pain management in the perioperative setting. Anesthesiology 82:1071–1081
Doyle E, Bowler GMR (1998) Pre-emptive effect of multimodal analgesia in thoracic surgery. Br J Anaesth 80:147–151
Dierking GW, Ostergaard E, Ostergaard HT, Dahl JB (1994) The effects of wound infiltration with bupivacaine versus saline on postoperative pain and opioid requirements after herniorrhaphy. Acta Anaesthesiol Scand 38:289–292
Johansson B, Hallerback B, Stubberod A, Janbu T, Edwin B, Glise H, Solhaug JH (1997) Preoperative local infiltration with ropivacaine for postoperative pain relief after inguinal hernia repair: a randomized controlled trial. Eur J Surg 163:371–378
Pettersson N, Emanuelsson BM (1998) High-dose ropivacaine wound infiltration for pain relief after inguinal hernia repair: a clinical and pharmacokinetic evaluation. Reg Anesth Pain Med 23:189–196
Schurr MJ, Gordon DB, Pellino TA, Scanlon TA (2004) Continuous local anesthetic infusion for pain management after outpatient inguinal herniorrhaphy. Surgery 136(4):761–769
Cleeland CS, Ryan KM (1994) Pain assessment: global use of the brief pain inventory. Ann Acad Med Singap 23:129–138
American Pain Society Quality of Care Committee (1995) Quality improvement guidelines for the treatment of acute pain and cancer pain. JAMA 274:1874–1880
Hong M, Tang J, White P, Zaentz A, Wender RH, Sloninsky A, Naruse R, Kariger R, Quon R, Wood D, Carroll BJ (2004) Perioperative rofecoxib improves early recovery after outpatient herniorrhaphy. Ambul Anesth 98:970–975
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R, Dunlop D, Gibbs J, Reda D, Henderson W (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Eng J Med 350:1819–1827
Acknowledgments
Supported by Merck & Co., Inc., West Point, PA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schurr, M.J., Faucher, L.D. A prospective, randomized, comparative trial of a COX-2 selective nonsteroidal anti-inflammatory drug versus placebo in inguinal herniorrhaphy patients. Hernia 13, 491–497 (2009). https://doi.org/10.1007/s10029-009-0489-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-009-0489-y