Abstract
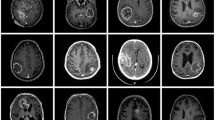
Surgery after administering bevacizumab should be carefully considered particularly because of wound healing concerns. A 27-year-old man presented with multiple tumor recurrences after gross total removal of a left temporal oligodendroglioma (1p/19q-noncodeleted). Whole brain radiotherapy with concomitant temozolomide and bevacizumab was immediately prescribed; however, the patient’s condition deteriorated because of brain herniation. Three days after administering bevacizumab, an emergency tumor removal with external decompression and a ventriculo-peritoneal shunt was performed. The surgery and postoperative clinical course were uneventful. On histopathological examination, the tumor showed findings such as tumor vessel thrombosis, numerous interstitial red blood cells, and cells with degraded, fragmented nuclei possibly suggesting apoptosis, which could be attributable to bevacizumab. Performing craniotomy shortly after administering bevacizumab is not recommended; however, it can still be safely performed as long as surgery and wound management is carefully performed. Vessel thrombosis might be among the mechanisms of action of bevacizumab.





Similar content being viewed by others
References
Chinot OL, Wick W, Mason W et al (2014) Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N Engl J Med 370:709–722. doi:10.1056/NEJMoa1308345
Gilbert MR, Dignam JJ, Armstrong TS et al (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 370:699–708. doi:10.1056/NEJMoa1308573
Di G, Hl C, Kr G et al (1996) Production of vascular endothelial growth factor by human tumors inhibits the functional maturation of dendritic cells. Nat Med 2(10):1096–1103
Jain RK, di Tomaso E, Duda DG et al (2007) Angiogenesis in brain tumours. Nat Rev Neurosci 8:610. doi:10.1038/NRN2175
Tamura R, Tanaka T, Miyake K et al (2016) Histopathological investigation of glioblastomas resected under bevacizumab treatment. Oncotarget 7(32):52423–52435
Laviv Y, Rappaport ZH (2014) Extremely late wound dehiscence following bevazicumab treatment in a long term survival glioblastoma patient. Clin Neurol Neurosurg 127:125–127. doi:10.1016/j.clineuro.2014.10.012
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (eds) (2007) WHO Classification of Tumours of the Central Nervous System, 4th edn. International Agency for Research on Cancer, Lyon
Clark AJ, Butowski NA, Chang SM et al (2011) Impact of bevacizumab chemotherapy on craniotomy wound healing. J Neurosurg 114:1609–1616. doi:10.3171/2010.10.JNS101042
Myers AL, Williams RF, Ng Cathy Y et al (2010) Bevacizumab-induced tumor vessel remodeling in rhabdomyosarcoma xenografts increases the effectiveness of adjuvant lonizing radiation. J Pediatr Surg 45(6):1080–1085
Winkler F, Kozin SV, Tong RT et al (2004) Kinetics of vascular normalization by VEGFR2 blockade governs brain tumor response to radiation: role of oxygenation, angiopoietin-1, and matrix metalloproteinases. Cancer Cell. doi:10.1016/j.ccr.2004.10.011
DeLay M, Jahangiri A, Carbonell W et al (2012) Microarray analysis verifies two distinct phenotypes of glioblastomas resistant to anti-angiogenic therapy. Clin Cancer Res 18(10):2930–2942
Von Baumgarten L, Brucker D, Tirniceru A et al (2011) Bevacizumab has differential and dose-dependent effects on glioma blood vessels and tumor cells. Clin Cancer Res 17:6192–6205. doi:10.1158/1078-0432.CCR-10-1868
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tokuda, Y., Tamura, R., Ohara, K. et al. A case of glioblastoma resected immediately after administering bevacizumab: consideration on histopathological findings and safety of surgery. Brain Tumor Pathol 34, 98–102 (2017). https://doi.org/10.1007/s10014-017-0285-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10014-017-0285-9