Abstract
Background
To retrospectively review lateral wall orbital decompression for thyroid eye disease (TED) and to evaluate pre-operative CT scans to analyse the variation in proptosis reduction.
Methods
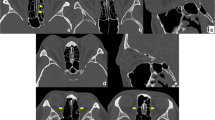
Consecutive lateral wall orbital decompressions performed by a single surgeon were retrospectively reviewed. Pre-operative CT scan features and post-operative proptosis reduction were analysed. The sphenoid trigone cross-sectional areas were summed and multiplied by the slice thickness to yield bone volume. Cumulative extraocular muscle thickness was calculated by combining the maximum thickness of the four recti. “Trigone volume” and “cumulative muscle thickness” were correlated with proptosis reduction at 3 months post-surgery.
Results
Out of 73 consecutive lateral wall orbital decompressions, 17 orbits had prior endonasal medial wall orbital decompression. In the remaining 56 orbits, the mean pre-operative and post-operative proptosis were 24.3 ± 1.6 mm and 20.9 ± 2.3 mm respectively. The proptosis reduction ranged from 1 to 7 mm (mean of 3.5 mm ± 1.3 (p < 0.001)). Mean sphenoid trigone volume was 895 ± 434.4 mm3. The mean cumulative muscle thickness was 20.4 ± 5 mm. The correlation coefficient between muscle thickness and proptosis reduction was − 0.3 and was statistically significant (p = 0.043). The correlation coefficient between sphenoidal trigone volume and proptosis reduction was 0.2 (p = 0.068). With a multivariate analysis, the coefficient of efficient of regression for muscle thickness was − 0.007 (p = 0.42) and the coefficient of regression for trigone volume was 0.0 (p = 0.046).
Conclusion
Proptosis reduction following lateral wall orbital decompression can be variable. Extraocular muscle thickness had a significant correlation with the outcome, with greater proptosis reduction in orbits with thin muscles. The sphenoidal trigone size had a weak correlation with decompression outcome.


Similar content being viewed by others
References
Mehta P, Durrani OM (2011) Outcome of deep lateral wall rim-sparing orbital decompression in thyroid-associated orbitopathy: a new technique and results of a case series. Orbit 30(6):265–268
Verity DH, Rose GE (2013) Acute thyroid eye disease (TED): principles of medical and surgical management. Eye (Lond) 27(3):308–319
Kim KW, Byun JS, Lee JK (2014) Surgical effects of various orbital decompression methods in thyroid-associated orbitopathy: computed tomography-based comparative analysis. J Craniomaxillofac Surg 42(7):1286–1291
Goldberg RA, Kim AJ, Kerivan KM (1998) The lacrimal keyhole, orbital door jamb, and basin of the inferior orbital fissure. Three areas of deep bone in the lateral orbit. Arch Ophthalmol 116(12):1618–1624
Fayers T, Barker LE, Verity DH, Rose GE (2013) Oscillopsia after lateral wall orbital decompression. Ophthalmology 120(9):1920–1923
Sellari-Franceschini S, Lenzi R, Santoro A et al (2010) Lateral wall orbital decompression in Graves’ orbitopathy. Int J Oral Maxillofac Surg 39(1):16–20
Borumandi F, Hammer B, Kamer L, von Arx G (2011) How predictable is exophthalmos reduction in Graves’ orbitopathy? A review of the literature. Br J Ophthalmol 95(12):1625–1630
Boboridis KG, Bunce C (2011) Surgical orbital decompression for thyroid eye disease. Cochrane Database Syst Rev 12:CD007630
Goldberg RA, Perry JD, Hortaleza V, Tong JT (2000) Strabismus after balanced medial plus lateral wall versus lateral wall only orbital decompression for dysthyroid orbitopathy. Ophthal Plast Reconstr Surg 16(4):271–277
Lukas K, Hansrudi N, Alexander S et al (2009) A step towards individualized, anatomy-based surgical concepts for orbital decompression in Graves’ orbitopathy. Orbit 28(4):237–240
Baujat B, Krastinova D, Bach CA et al (2006) Orbital morphology in exophthalmos and exorbitism. Plast Reconstr Surg 117(2):542–550 (discussion 551-542)
Baldeschi L, MacAndie K, Hintschich C et al (2005) The removal of the deep lateral wall in orbital decompression: its contribution to exophthalmos reduction and influence on consecutive diplopia. Am J Ophthalmol 140(4):642–647
Goncalves AC, Gebrim EM, Monteiro ML (2012) Imaging studies for diagnosing Graves’ orbitopathy and dysthyroid optic neuropathy. Clinics (Sao Paulo) 67(11):1327–1334
Kamer L, Noser H, Schramm A et al (2010) Anatomy-based surgical concepts for individualized orbital decompression surgery in graves orbitopathy. I. Orbital size and geometry. Ophthal Plast Reconstr Surg. 26(5):348–352
Kamer L, Noser H, Kirsch E, Hammer B (2012) Anatomy-based surgical concepts for individualized orbital decompression surgery in graves orbitopathy. II. Orbital rim position and angulation. Ophthal Plast Reconstr Surg 28(4):251–255
Borumandi F, Hammer B, Noser H, Kamer L (2013) Classification of orbital morphology for decompression surgery in Graves’ orbitopathy: two-dimensional versus three-dimensional orbital parameters. Br J Ophthalmol 97(5):659–662
Takahashi Y, Miyazaki H, Ichinose A, Nakano T, Asamoto K, Kakizaki H (2013) Anatomy of deep lateral and medial orbital walls: implications in orbital decompression surgery. Orbit (Amsterdam, Netherlands) 32(6):409–412. https://doi.org/10.3109/01676830.2013.833256
Cruz AAV, Equiterio BSN, Cunha BSA, Caetano FB, Souza RL (2021) Deep lateral orbital decompression for Graves orbitopathy: a systematic review. Int Ophthalmol 41(5):1929–1947. https://doi.org/10.1007/s10792-021-01722-3
Lefebvre DR, Yoon MK (2015) CT-based measurements of the sphenoid trigone in different sex and race. Ophthal Plast Reconstr Surg 31(2):155–158
Beden U, Edizer M, Elmali M et al (2007) Surgical anatomy of the deep lateral orbital wall. Eur J Ophthalmol 17(3):281–286
Bijlsma WR, Mourits MP (2006) Radiologic measurement of extraocular muscle volumes in patients with Graves’ orbitopathy: a review and guideline. Orbit 25(2):83–91
Stabile JR, Trokel SM (1983) Increase in orbital volume obtained by decompression in dried skulls. Am J Ophthalmol 95(3):327–331
Hu WD, Annunziata CC, Chokthaweesak W et al (2010) Radiographic analysis of extraocular muscle volumetric changes in thyroid-related orbitopathy following orbital decompression. Ophthal Plast Reconstr Surg 26(1):1–6
Alsuhaibani AH, Carter KD, Policeni B, Nerad JA (2011) Orbital volume and eye position changes after balanced orbital decompression. Ophthal Plast Reconstr Surg 27(3):158–163
Gupta A, Nobori A, Wang Y et al (2017) Lateral rectus muscle expands more than medial rectus following maximal deep balanced orbital decompression. Ophthal Plast Reconstr Surg 34(2):140–142
Acknowledgements
We acknowledge Dr Dympna McAteer, Radiologist at Aberdeen Royal Infirmary, and Dr Oliver Cram, Radiologist at Gartnavel General Hospital, for their expert opinion on radiological assessment and Margaret Daddow for facilitating data acquisition.
Author information
Authors and Affiliations
Contributions
All authors contributed to this study. Paul Cauchi and Manvi Sobti contributed to the study conception and design. Material preparation and data collection and analysis were performed by Manvi Sobti, Kerr Brogan and Radhika Patel. The first draft of the manuscript was written by Manvi Sobti and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This is an observational study. The West of Scotland Research Ethics Service has confirmed that no ethical approval is required.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Meeting presentation.
These results have been presented at the ESOPRS 2017 Meeting, Stockholm as an oral presentation and at BOPSS 2017 Meeting, London as a poster.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sobti, M., Brogan, K., Patel, R. et al. Impact of sphenoid trigone size and extraocular muscle thickness on the outcome of lateral wall orbital decompression for thyroid eye disease. Oral Maxillofac Surg 28, 307–313 (2024). https://doi.org/10.1007/s10006-023-01143-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-023-01143-9