Abstract
Objectives
To investigate the pain perception (PP) and condyle-fossa relationship (CFR) after botulinum toxin A (BoNTA) injection in the masseter muscles of painful muscular temporomandibular dysfunction (TMD) patients.
Materials and methods
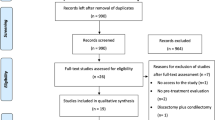
Fourteen women (aged 29.7 ± 5.4 years) diagnosed with myogenic TMD were randomized in the BoNTA-treated group (TG) and control group (CG). TG masseter muscles (n = 7) were bilaterally injected with 30 U. The CG (n = 7) were injected with saline injections. Condyle-fossa relationship (CFR) spaces were measured in sagittal (SP) and frontal planes (FP) of images of cone-beam computed tomography (CBCT) done before (T0) and after 30 days’ interventions (T1). Visual analogue scale (VAS) measured the patients’ TMD pain perception (PP). Data were compared by generalized linear models considering the results over time (α = .05).
Results
There were no statistical differences in CFR in the SP or FP for TG and CG over time (p ˃ .05), except for frontal lateral space CFR (p < .05). In both groups, the condyle was positioned medially after interventions. Frontal lateral space increased in TG for both, left and right sides, over time (p < .05), as well as PP decreased over time (p < .05) for TG and CG.
Conclusions
The results depicted that there was no significant association with BoNTA injection in TMD masseter muscles in PP and CFR, except considering the frontal lateral space of CFR.
Clinical relevance
BoNTA injection in the masseter muscles may not promote clinically significant shifts in the condyle-fossa relationships of muscular TMD patients.



Similar content being viewed by others
Data Availability
All data generated or analysed during this study are included in this published article (and its supplementary information files).
References
Fredrick CM, Lin G, Johnson EA (2017) Regulation of botulinum neurotoxin synthesis and toxin complex formation by arginine and glucose in Clostridium botulinum ATCC 3502. Appl Environ Microbiol 83(13):e00642-e717. https://doi.org/10.1128/AEM.00642-17
Dressler D, Saberi FA, Barbosa ER (2005) Botulinum toxin: mechanisms of action. Arq Neuropsiquiatr 63(1):180–185. https://doi.org/10.1590/s0004-282x2005000100035
Cahlin BJ, Lindberg C, Dahlström L (2019) Cerebral palsy and bruxism: effects of botulinum toxin injections-a randomized controlled trial. Clin Exp Dent Res 5(5):460–468. https://doi.org/10.1002/cre2.207
Stonehouse-Smith D, Begley A, Dodd M (2020) Clinical evaluation of botulinum toxin A in the management of temporomandibular myofascial pain. Br J Oral Maxillofac Surg 58(2):190–193. https://doi.org/10.1016/j.bjoms.2019.11.010
Aoki KR (2003) Evidence for antinociceptive activity of botulinum toxin type A in pain management. Headache 43(Suppl 1):S9-15. https://doi.org/10.1046/j.1526-4610.43.7s.3.x
Cui M, Khanijou S, Rubino J, Aoki KR (2004) Subcutaneous administration of botulinum toxin A reduces formalin-induced pain. Pain 107(1–2):125–133. https://doi.org/10.1016/j.pain.2003.10.008
DrinovacVlah V, Bach-Rojecky L, Lacković Z (2016) Antinociceptive action of botulinum toxin type A in carrageenan-induced mirror pain. J Neural Transm (Vienna) 123(12):1403–1413. https://doi.org/10.1007/s00702-016-1605-7
Lora VR, Clemente-Napimoga JT, Abdalla HB, Macedo CG, Canales GT, Barbosa CM (2017) Botulinum toxin type A reduces inflammatory hypernociception induced by arthritis in the temporomadibular joint of rats. Toxicon 129:52–57. https://doi.org/10.1016/j.toxicon.2017.02.010
Matak I, Lacković Z (2014) Botulinum toxin A, brain and pain. Prog Neurobiol 119–120:39–59. https://doi.org/10.1016/j.pneurobio.2014.06.001
Caleo M, Spinelli M, Colosimo F, Matak I, Rossetto O, Lackovic Z, Restani L (2018) Transynaptic action of botulinum neurotoxin type A at central cholinergic boutons. J Neurosci 38(48):10329–10337. https://doi.org/10.1523/JNEUROSCI.0294-18.2018
Lacković Z, Filipović B, Matak I, Helyes Z (2016) Activity of botulinum toxin type A in cranial dura: implications for treatment of migraine and other headaches. Br J Pharmacol 173(2):279–291. https://doi.org/10.1111/bph.13366
Matak I (2020) Evidence for central antispastic effect of botulinum toxin type A. Br J Pharmacol 177(1):65–76. https://doi.org/10.1111/bph.14846
DrinovacVlah V, Bach-Rojecky L (2020) What have we learned about antinociceptive effect of botulinum toxin type A from mirror-image pain models? Toxicon 15(185):164–173. https://doi.org/10.1016/j.toxicon.2020.07.014
Lacković Z (2020) New analgesic: Focus on botulinum toxin. Toxicon 179:1–7. https://doi.org/10.1016/j.toxicon.2020.02.008
Radu M, Marandici M, Hottel TL (2004) The effect of clenching on condylar position: a vector analysis model. J Prosthet Dent 91(2):171–179. https://doi.org/10.1016/j.prosdent.2003.10.011
Tsai CY, Lin YC, Su B, Yang LY, Chiu WC (2012) Masseter muscle fibre changes following reduction of masticatory function. Int J Oral Maxillofac Surg 41(3):394–399. https://doi.org/10.1016/j.ijom.2011.10.016
Igarashi Y, Yamashita S, Kuroiwa A (1999) Changes in interarch distance and condylar position related to loss of occlusal support for partially edentulous patients. a pilot study. Eur J Prosthodont Restor Dent 7(4):107–11
Chae JM, Park JH, Tai K, Mizutani K, Uzuka S, Miyashita W, Seo HY (2020) Evaluation of condyle-fossa relationships in adolescents with various skeletal patterns using cone-beam computed tomography. Angle Orthod 90(2):224–232. https://doi.org/10.2319/052919-369.1
Andrews LF (1972) The six keys to normal occlusion. Am J Orthod 62(3):296–309. https://doi.org/10.1016/s0002-9416(72)90268-0
Schiffman E, Ohrbach R, Truelove E et al (2014) International RDC/TMD consortium network, international association for dental research; orofacial pain special interest group, international association for the study of pain. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache 28(1):6–27. https://doi.org/10.11607/jop.1151
Banerjee S, Ray S, Narayan SV et al (2019) A Comparative study of photographic and cephalometric measurements in adult female Bengalee population. J Dent Med Sci 18:33–39
Martins LF, Vigorito JW (2012) Photometric analysis applied in determining facial type. Dental Press J Orthod 17:71–75
Patel DP, Trivedi R (2013) Photography versus lateral cephalogram: role in facial diagnosis. Indian J Dent Res 24(5):587–92. https://doi.org/10.4103/0970-9290.123378
Urbaniak GC, Plous S (2013) Research Randomizer. Available from: www.randomizer.org.
Villa S, Raoul G, Machuron F, Ferri J, Nicot R (2019) Improvement in quality of life after botulinum toxin injection for temporomandibular disorder. J Stomatol Oral Maxillofac Surg 120(1):2–6. https://doi.org/10.1016/j.jormas.2018.10.007
Lee SJ, McCall WD Jr, Kim YK, Chung SC, Chung JW (2010) Effect of botulinum toxin injection on nocturnal bruxism: a randomized controlled trial. Am J Phys Med Rehabil 89(1):16–23. https://doi.org/10.1097/PHM.0b013e3181bc0c78
Dutra EH, Yadav S (2019) The effects on the mandibular condyle of Botox injection into the masseter are not transient. Am J Orthod Dentofacial Orthop 156(2):193–202. https://doi.org/10.1016/j.ajodo.2018.08.023
Lelis ÉR, Guimarães Henriques JC, Tavares M, de Mendonça MR, Fernandes Neto AJ, Almeida GA (2015) Cone-beam tomography assessment of the condylar position in asymptomatic and symptomatic young individuals. J Prosthet Dent 114(3):420–425. https://doi.org/10.1016/j.prosdent.2015.04.006
Szklo M, Nieto JF (eds) (2000) Epidemiology: beyond the basics. Aspen Publishers, Gaithersburg
de Melo Júnior PC, Aroucha JMCNL, Arnaud M, Lima MGS, Gomes SGF, Ximenes R, Rosenblatt A, Caldas AF Jr (2019) Prevalence of TMD and level of chronic pain in a group of Brazilian adolescents. PLoS One 14(2):e0205874. https://doi.org/10.1371/journal.pone.0205874
LeResche L, Mancl LA, Drangsholt MT, Saunders K, Von Korff M (2005) Relationship of pain and symptoms to pubertal development in adolescents. Pain 118(1–2):201–209. https://doi.org/10.1016/j.pain.2005.08.011
Gonçalves DA, Dal Fabbro AL, Campos JA, Bigal ME, Speciali JG (2010) Symptoms of temporomandibular disorders in the population: an epidemiological study. J Orofac Pain 24(3):270–8
Yadav S, Yang Y, Dutra EH, Robinson JL, Wadhwa S (2018) Temporomandibular joint disorders in older adults. J Am Geriatr Soc 66(6):1213–1217. https://doi.org/10.1111/jgs.15354
Ernberg M, Hedenberg-Magnusson B, List T, Svensson P (2011) Efficacy of botulinum toxin type A for treatment of persistent myofascial TMD pain: a randomized, controlled, double-blind multicenter study. Pain 152(9):1988–1996. https://doi.org/10.1016/j.pain.2011.03.036
Pihut M, Ferendiuk E, Szewczyk M, Kasprzyk K, Wieckiewicz M (2016) The efficiency of botulinum toxin type A for the treatment of masseter muscle pain in patients with temporomandibular joint dysfunction and tension-type headache. J Headache Pain 17:29. https://doi.org/10.1186/s10194-016-0621-1
Özden MC, Atalay B, Özden AV, Çankaya A, Kolay E, Yıldırım S (2020) Efficacy of dry needling in patients with myofascial temporomandibular disorders related to the masseter muscle. Cranio 38(5):305–311. https://doi.org/10.1080/08869634.2018.1526848
Dib-Zakkour J, Flores-Fraile J, Montero-Martin J, Dib-Zakkour S, Dib-Zaitun I (2022) Evaluation of the effectiveness of dry needling in the treatment of myogenous temporomandibular joint disorders. Medicina (Kaunas) 58(2):256. https://doi.org/10.3390/medicina58020256
Lomas J, Gurgenci T, Jackson C, Campbell D (2018) Temporomandibular dysfunction. Aust J Gen Pract 47(4):212–215. https://doi.org/10.31128/AFP-10-17-4375
Kapos FP, Exposto FG, Oyarzo JF, Durham J (2020) Temporomandibular disorders: a review of current concepts in aetiology, diagnosis and management. Oral Surg 13(4):321–334. https://doi.org/10.1111/ors.12473
Plesh O, Adams SH, Gansky SA (2011) Temporomandibular joint and muscle disorder-type pain and comorbid pains in a national US sample. J Orofac Pain 25(3):190–8
Lerman SF, Campbell CM, Buenaver LF, Medak M, Phillips J, Polley M, Smith MT, Haythornthwaite JA (2018) Exploring the role of negative cognitions in the relationship between ethnicity, sleep, and pain in women with temporomandibular joint disorder. J Pain 19(11):1342–1351. https://doi.org/10.1016/j.jpain.2018.05.009
Gui MS, Pedroni CR, Aquino LM, Pimentel MJ, Alves MC, Rossini S, Reimão R, Berzin F, Marques AP, Rizzatti-Barbosa CM (2013) Facial pain associated with fibromyalgia can be marked by abnormal neuromuscular control: a cross-sectional study. Phys Ther 93(8):1092–1101. https://doi.org/10.2522/ptj.20120338
Pimentel MJ, Gui MS, Martins de Aquino LM, Rizzatti-Barbosa CM (2013) Features of temporomandibular disorders in fibromyalgia syndrome. Cranio 31(1):40–5. https://doi.org/10.1179/crn.2013.006
Meloto CB, Serrano PO, Ribeiro-DaSilva MC, Rizzatti-Barbosa CM (2011) Genomics and the new perspectives for temporomandibular disorders. Arch Oral Biol 56(11):1181–1191. https://doi.org/10.1016/j.archoralbio.2011.03.012
Meloto CB, Segall SK, Smith S et al (2015) COMT gene locus: new functional variants. Pain 156(10):2072–2083. https://doi.org/10.1097/j.pain.0000000000000273
De la Torre CG, Poluha RL, Pinzón NA, Da Silva BR, Almeida AM, Ernberg M, Manso AC, Bonjardim LR, Rizzatti-Barbosa CM (2022) Efficacy of botulinum toxin type-A I in the improvement of mandibular motion and muscle sensibility in myofascial pain TMD subjects: a randomized controlled trial. Toxins (Basel) 14(7):441. https://doi.org/10.3390/toxins14070441
Aoki KR (2004) Botulinum toxin: a successful therapeutic protein. Curr Med Chem 11(23):3085–3092. https://doi.org/10.2174/0929867043363802
De la Torre CG, Alvarez-Pinzon N, Muñoz-Lora VRM, Vieira Peroni L, Farias Gomes A, Sánchez-Ayala A, Haiter-Neto F, Manfredini D, Rizzatti-Barbosa CM (2020) Efficacy and safety of botulinum toxin type A on persistent myofascial pain: a randomized clinical trial. Toxins (Basel) 12(6):395. https://doi.org/10.3390/toxins12060395
Matthys T, Ho Dang HA, Rafferty KL, Herring SW (2015) Bone and cartilage changes in rabbit mandibular condyles after 1 injection of botulinum toxin. Am J Orthod Dentofacial Orthop 148(6):999–1009. https://doi.org/10.1016/j.ajodo.2015.05.034
Nazet U, Feulner L, Muschter D, Neubert P, Schatz V, Grässel S, Jantsch J, Proff P, Schröder A, Kirschneck C (2021) Mechanical stress induce PG-E2 in murine synovial fibroblasts originating from the temporomandibular joint. Cells 10(2):298. https://doi.org/10.3390/cells10020298
Nitzan DW (1994) Intraarticular pressure in the functioning human temporomandibular joint and its alteration by uniform elevation of the occlusal plane. J Oral Maxillofac Surg 52(7):671–9; discussion 679–80. https://doi.org/10.1016/0278-2391(94)90476-6.
Asakawa-Tanne Y, Su S, Kunimatsu R, Hirose N, Mitsuyoshi T, Okamoto Y, Tanaka E, Tanne K, Tanimoto K (2015) Effects of enzymatic degradation after loading in temporomandibular joint. J Dent Res 94(2):337–343. https://doi.org/10.1177/0022034514560588
Matak I, Bölcskei K, Bach-Rojecky L, Helyes Z (2019) Mechanisms of botulinum toxin type A action on pain. Toxins (Basel) 11(8):459. https://doi.org/10.3390/toxins11080459
Paknahad M, Shahidi S (2015) Association between mandibular condylar position and clinical dysfunction index. J Craniomaxillofac Surg 43(4):432–436. https://doi.org/10.1016/j.jcms.2015.01.005
Ramachandran A, Jose R, Tunkiwala A et al (2021) Effect of deprogramming splint and occlusal equilibration on condylar position of TMD patients - A CBCT assessment. Cranio 39(4):294–302. https://doi.org/10.1080/08869634.2019.1650216
Shokri A, Zarch HH, Hafezmaleki F, Khamechi R, Amini P, Ramezani L (2019) Comparative assessment of condylar position in patients with temporomandibular disorder (TMD) and asymptomatic patients using cone-beam computed tomography. Dent Med Probl 56(1):81–87. https://doi.org/10.17219/dmp/102946
Rabelo KA, Sousa Melo SL, Torres MGG, Peixoto LR, Campos PSF, Rebello IMCR, de Melo DP (2017) Assessment of condyle position, fossa morphology, and disk displacement in symptomatic patients. Oral Surg Oral Med Oral Pathol Oral Radiol 124(2):199–207. https://doi.org/10.1016/j.oooo.2017.04.007
Meral SE, Karaaslan S, Tüz HH, Uysal S (2022) Evaluation of the temporomandibular joint morphology and condylar position with cone-beam computerized tomography in patients with internal derangement. Oral Radiol. https://doi.org/10.1007/s11282-022-00618-x
Badel T, Pavicin IS, Jakovac M, Kern J, Zadravec D (2013) Disc and condylar head position in the temporomandibular joint with and without disc displacement. Coll Antropol 37(3):901–906
Robinson de Senna B, Marques LS, França JP, Ramos-Jorge ML, Pereira LJ (2009) Condyle-disk-fossa position and relationship to clinical signs and symptoms of temporomandibular disorders in women. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108(3):e117-24. https://doi.org/10.1016/j.tripleo.2009.04.034
Al-koshab M, Nambiar P, John J (2015) Assessment of condyle and glenoid fossa morphology using CBCT in South-East Asians. PLoS One. 10(3):e0121682. https://doi.org/10.1371/journal.pone.0121682
Bakke M, Møller E, Werdelin LM, Dalager T, Kitai N, Kreiborg S (2005) Treatment of severe temporomandibular joint clicking with botulinum toxin in the lateral pterygoid muscle in two cases of anterior disc displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 100(6):693–700. https://doi.org/10.1016/j.tripleo.2004.11.019
Omar R, Wise MD (1981) Mandibular flexure associated with muscle force applied in the retruded axis position. J Oral Rehabil 8(3):209–221. https://doi.org/10.1111/j.1365-2842.1981.tb00495.x
Hassall D (2021) Centric relation and increasing the occlusal vertical dimension: concepts and clinical techniques - part one. Br Dent J 230:17–22. https://doi.org/10.1038/s41415-020-2502-x
de Kattiney Oliveira L, Fernandes Neto AJ, Moraes Mundim Prado I, Guimarães Henriques JC, Beom Kim K, de Araújo Almeida G (2022) Evaluation of the condylar position in younger and older adults with or without temporomandibular symptoms by using cone beam computed tomography. J Prosthet Dent 127(3):445–452. https://doi.org/10.1016/j.prosdent.2020.10.019
Krasińska-Mazur M, Homel P, Gala A, Stradomska J, Pihut M (2022) Differential diagnosis of temporomandibular disorders - a review of the literature. Folia Med Cracov 62(2):121–137. https://doi.org/10.24425/fmc.2022.141703
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Julian Calegari Ayala and William Custodio. The first draft of the manuscript was written by Julian Calegari Ayala. Writing—review and editing were carried out by Célia Marisa Rizzatti-Barbosa and William Custodio. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The ethical committee approved the study protocol (CAAE:23745319.1.0000.5385.).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ayala, J.C., Rizzatti-Barbosa, C.M. & Custodio, W. Influence of botulinum toxin A in pain perception and condyle-fossa relationship after the management of temporomandibular dysfunction: a randomized controlled clinical trial. Oral Maxillofac Surg 28, 269–277 (2024). https://doi.org/10.1007/s10006-023-01141-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-023-01141-x