Abstract
Introduction
In severe TMJ ankylosis cases, the lack of growth of the mandible creates an anatomically narrow airway with a reduced pharyngeal airway space [PAS] which predisposes these patients towards obstructive apnoea [OSA]. There is evidence in the literature that such patients experience severe discomfort during physiotherapy if such airway abnormalities are not corrected prior to ankylosis release. This eventually leads to non-compliance towards physiotherapy and increases the risk of re-ankylosis.
Objective
In our study, pre-arthroplastic mandibular distraction osteogenesis [DO] was used to increase the PAS and resolve the underlying OSA prior to releasing the ankylosis.
Materials and methods
Twenty-five cases of TMJ ankylosis with micrognathia and OSA were included in this prospective observational sleep study. They were further divided into a paediatric group [14 subjects] and an adult group [11 subjects]. All cases presented with a history of onset of ankylosis during childhood [before the completion of craniofacial growth] as result of which there was a lack of forward growth of the mandible. Subjects included in our study underwent initial DO of the mandible followed by a second procedure for distractor removal and ankylosis release. Questionnaires, lateral cephalograms and sleep studies were taken pre-operatively (T0), immediate post-distraction to the desired length (T1) and 12 months post the distractor removal and ankylosis release (T2). The parameters studied were PAS width, apnoea hypopnea index [AHI], O2 saturation, mouth opening and mandibular advancement.
Results
The paediatric group variables were as follows: mean PAS width which increased from 3.5 mm [T0] to 9 mm [T2], mean AHI which decreased from 48.04 [T0] to 3.60 [T2], mouth opening which increased from 4.5 mm [T0] to 34 mm [T2] and mean O2 saturation which increased from 89.86% [T1] to 96.88% [T2]. The adult group variables were as follows: mean PAS width which increased from 5 mm [T0] to 11 mm [T2], mean AHI which decreased from 31.45 [T0] to 1.43 [T2], mouth opening which increased from 5 mm [T0] to 34 mm [T2] and mean O2 saturation which increased from 92.01% [T0] to 96.84% [T2]. Statistical analysis revealed that DO of the mandible significantly improved OSA by increasing the PAS which was evident by the lower AHI score. Mouth opening was also significantly improved post ankylosis release and maintained at the T2 interval. Ten subjects followed up beyond the T2 interval [mean 28 months post ankylosis release] and their data also revealed positive compliance towards physiotherapy, adequate mouth opening and maintenance of normal AHI.
Conclusion
Pre-arthroplastic mandibular DO has proved to be a successful modality for treatment of OSA in TMJ ankylosis patients with stable results at 12 months. By resolving the narrow airway and OSA, compliance towards physiotherapy was improved thus reducing the risk of re-ankylosis in the long term.
Similar content being viewed by others
Introduction
Temporo-mandibular joint [TMJ] ankylosis is a pathological condition which is characterised by the fusion of the mandibular condyle to the articular fossa by bony or fibrotic tissue. It may be unilateral or bilateral in nature. This leads to a reduction in mouth opening which interferes with normal day-to-day activities like mastication, oral hygiene and speech [1]. TMJ ankylosis in the growing child is also associated with severe dento-facial deformities like micrognathia, retrogenia and a retruded three-dimensional position of the mandible that persist through adult life. This leads to an anatomically narrow pharyngeal airway space and an increased propensity for retro-displacement of the tongue during sleep resulting in OSA in the patient [2].
The primary management goal of TMJ ankylosis is to increase mouth opening, correct the dento-facial deformity and prevent re-ankylosis. This is achieved by surgical release of the TMJ ankylosis [gap arthroplasty or inter-positional arthroplasty] and total joint reconstruction [if feasible]. In the post-operative period, aggressive physiotherapy [jaw stretching exercises] is the mainstay to prevent re-ankylosis [1]. However, patients of TMJ ankylosis with OSA are known to have a narrow pharyngeal airway space [PAS] that leads to the stimulation of the trigemino-cardiac reflex [respiratory distress, bradycardia and a drop in oxygen saturation] on post-operative physiotherapy [2]. This leads to non-compliance during jaw stretching exercises and increases the risk re-ankylosis. In the literature, many surgeons have supported the correction of underlying OSA and narrow airway prior to TMJ ankylosis release [2]. Furthermore, OSA is associated with multiple health problems like excessive day time somnolence, coronary artery disease, diabetes, hypertension, insomnia, behavioural changes and decreased concentration. Thus, it is necessary to diagnose and treat this condition to prevent the long-term adverse effects associated with it [3].
In this study, mandibular distraction osteogenesis [DO] was utilised for the correction of OSA and reduced PAS prior to TMJ ankylosis release. Theoretically, this should help to reduce the discomfort experienced during post-op physiotherapy and increase compliance towards the same. Lateral cephalometry, questionnaires and polysomnographic studies were the prime determinants [pre- and post-surgery] to judge the effectiveness of the treatment.
Materials and methods
Study framework
A prospective observational study was conducted in the Department of Oral and Maxillofacial Surgery [Nair Hospital Dental College, Mumbai, India] after institutional ethical approval. The inclusion criteria were: [a] patients presenting with a triad of TMJ ankylosis with OSA and micrognathia, [b] minimum age of 6 years for increased compliance to instructions in post-operative phase [4]. The exclusion criteria were as follows: [a] OSA other than secondary to temporomandibular joint ankylosis, [b] patients with fibrous ankylosis, [c] patients below 5 years of age, [d] patients considered as non-complaint and [e] medically compromised patients and those not fit to be taken under general anaesthesia.
Twenty-five patients of TMJ ankylosis, who met the above criteria, were included in the study after obtaining informed consent. It should be noted that all the patients gave a history of developing ankylosis before the completion of craniofacial growth [i.e. during childhood] as result of which there was a lack of forward growth of the mandible. The patients were operated between 2011 and 2015 and were followed up post-operatively for a period of at least 12 months. The patients presented with complaints of reduced mouth opening, snoring during sleep, episodes of awakening at night and day time somnolence. The subjects displayed severe dento-facial deformities like micrognathia and retrognathism. A CT scan was performed pre-operatively to evaluate the severity of the ankylosis and micrognathia.
The subjects were assessed with questionnaires, polysomnographic studies and lateral cephalometry at T0 [immediate pre-operative], T1 [immediate post-operative], T2 [late post-operative] time intervals. T1 refers to the time period immediately after the mandible has been distracted to the desired length. T2 refers to the time period 12 months post the distractor removal and TMJ ankylosis release. The study team consisted of four maxillofacial surgeons and two maxillofacial surgery residents and one consultant orthodontist. Different authors were assigned for the measurement of pre-op and post-op variables as a means to reduce bias [operating surgeons: NNA and SG, T0 cephalogram analysis: PCM and orthodontist, T1 cephalogram analysis: NA and orthodontist, T2 cephalogram analysis: KR/TN and orthodontist, pre-op questionnaire: PCM/KR, post-op questionnaire: NA/TN].
The questionnaire comprised three questions and was answered by the parents or the spouse of the patient at T0, T1 and T2 intervals. The first question [Q1] addressed the presence or absence of snoring while the patient was asleep. The second question [Q2] addressed the presence or absence of night time awakening episodes. The third question [Q3] addressed the presence or absence of day time somnolence.
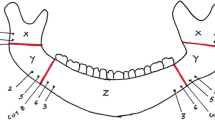
The lateral cephalogram was used to assess the amount of mandibular advancement and the width of the PAS. The lateral cephalogram was standardised with a cephalostat consisting of two ear-rods and a forehead clamp to help maintain a constant reproducible head position and the distance between the midsagittal plane of the subject’s head to the x-ray tube fixed at 5 ft. The same orthodontist was responsible for cephalometric tracing at all time intervals as a measure to maintain reproducibility of landmarks. The cephalometric analysis was made by the orthodontist together with the maxillofacial surgeon assigned according to the time interval [T0: PCM, T1: NA, T2: KR/TN]. The mandibular advancement was calculated as the difference of the distance between the gonion and the menton at T1 and T0 intervals. The degree of post-distraction relapse of mandibular advancement was calculated comparing the distance between the gonion and the menton at T1 and T2 intervals. The PAS width was measured from the point of intersection of the posterior border of the tongue and the inferior border of the mandible to the closest point on the posterior pharyngeal wall [McNamara lateral cephalometric analysis]. The PAS width was further classified as normal width [11–14 mm], mild narrowing [8–10.9 mm], moderate narrowing [5–7.9 mm] and severe narrowing [< 5 mm] [2] (Fig. 1).
Lateral Cephalogram Analysis: Distance from Gonion [Go] to Menton [Me] to determine mandibular advancement, Distance from X [point of intersection of the posterior border of the tongue and the inferior border of the mandible] to Y [closest point on the posterior pharyngeal wall] to determine the posterior pharyngeal airway space
The polysomnographic study [sleep study] variables included in this study were mean O2 saturation and apnoea hypopnea index [AHI]. The sleep study was performed at T0, T1 and T2 intervals.
Mandibular distraction and ankylosis release
The amount of mandibular advancement needed was calculated pre-operatively by lateral cephalometric analysis [taking the PAS width and the dental overjet into consideration]. An internal bone borne uni-directional horizontal body distractor was used. The span of the distractor used was 15 mm. The vector of DO was planned with the help of a stereolithographic model and 3d-CT and was primarily kept parallel to the inferior border of the body of the mandible. This vector helped gain a considerable increase in the horizontal antero-posterior dimension of the mandibular body with a mild increase in the anterior facial height (Fig. 2). Distractor placement took place under general anaesthesia via an extra-oral sub-mandibular incision and the activator port was introduced intra-orally. A latency period of 4 days was maintained. The appliance was activated for a total distance of 1 mm/day using two intervals of 0.5 mm each. Once the desired amount of mandibular advancement was achieved, a consolidation period of 3–4 months was maintained. Post the consolidation period, simultaneous removal of the distractor and TMJ ankylosis release was performed under general anaesthesia (Fig. 3). The distractor was removed via the same submandibular extra-oral approach. TMJ gap arthroplasty of 10–12 mm was preformed via a pre-auricular approach using conventional rotary technique with copious irrigation. An average mouth opening between 35 and 40 mm was achieved on table. Inter-position of the gap with abdominal dermis fat was the treatment of choice on account of its ability to prevent bone formation and maintain its volume by neo-adipogenesis [4, 5]. The subjects were then motivated to perform aggressive jaw stretching exercises. The subjects and their families were also counselled regarding the need to continue jaw-exercises in the long term to help maintain the surgically achieved mouth opening and reduce the risk of re-ankylosis.
Statistical analysis
The data obtained was compiled on MS Office Excel Sheet (v 2010) and was subjected to statistical analysis using the Statistical Package for Social Sciences (SPSS v 21.0, IBM) software. Comparison of numerical variables between age groups at T0, T1 and T2 intervals was done using the ‘independent t test’ for data following a normal distribution and the ‘Mann-Whitney U test’ for non-normal data. Comparison of frequencies of variables between the age groups was done using the Chi square test. Intra group comparison was done using the ‘paired t test’ [up to two observations] and ‘repeated measures ANOVA test’ [more than two observations] for data following a normal distribution and ‘Friedman test’ [more than two observations] for non-normal data. Post hoc tests like ‘Tukey HSD’ and ‘Wilcoxson signed rank test’ were performed to determine further significance by testing all pairwise comparisons among means. For all the statistical tests, p < 0.05 was considered to be statistically significant, keeping α error at 5% and β error at 20%, thus giving a power to the study as 80%.
Results
Baseline values
A total of 25 patients were included in the study of which 14 were male and 11 were female. Eighteen subjects had unilateral ankylosis and 7 had bilateral ankylosis. The subjects were further divided into a [PG] paediatric group [< 18 years] with 14 subjects and an [AG] adult group with 11 participants. The mean age of the PG was 11.85 years [range of 6 to 17 years] and that of the AG was 21.81 years [range of 18 to 26 years]. There was no statistically significant difference seen between the frequency distribution of affected TMJs and the age groups (Tables 1 and 2).
Paediatric group
The mean mandibular advancement at T1 was 10.14 mm and at T2 was 10.07 mm. The paired t test for the above values revealed that there was no statistically significant difference [p > 0.05] between these values. This indicated that the mandibular advancement gained from mandibular DO was stable at 12 months post the distractor removal (Table 4 and Figs. 4, 5 and 6).
Lateral cephalogram at T0 and T1 intervals showing a horizontal distractor in situ. There is an increase in the phayngeal airway space, reduction in the dental overjet and improvement in the facial profile on account of the mandibular distraction. The vector for distraction [red] has been maintained parallel to the inferior border of the mandible [yellow] as compared to the occlusal plane [green and blue]
Lateral cephalogram analysis at T1 and T2 intervals. Note that a slight open bite and increase in the overjet is seen at the T2 interval on account of the TMJ ankylosis release which caused the mandible to swing backwards leading to the creation of an anterior open bite and mild increase in the overjet
The mean PAS width at T0, T1 and T2 were 3.57 mm [severe narrowing], 8.68 mm [mild narrowing] and 9 mm [mild narrowing], respectively. ANOVA and post hoc Tukey HSD tests for significance were carried out for the above parameter. The PAS width with mandibular advancement revealed a statistically significant difference [p < 0.05] when the T1 vs. T0 and T2 vs. T0 values were compared. On comparison of T2 vs. T1 values, there was no statistically significant difference [p > 0.05], thus showing the stability of the result obtained by mandibular DO at 12 months post the distractor removal (Tables 5 and 6, Figs. 4, 5 and 6).
The mean AHI at T0, T1 and T2 were 48.04, 3.41 and 3.60, respectively. Friedman and post hoc Wilcoxon signed rank tests for significance were carried out for the above parameter. There was significant resolution of the OSA associated with the increase in the PAS width as shown by the difference for T1 vs. T0 and T2 vs. T0 values [p < 0.05]. On comparison of T2 vs. T1 values, there was no statistically significant difference [p > 0.05]. As both the T1 and T2 AHI scores were lesser than 5 [AHI 1–5 is mild for children], it indicated that the improvement in OSA obtained by mandibular DO was maintained at 12 months post the distractor removal [6] (Tables 5 and 6).
The mean SpO2 saturations at T0, T1 and T2 were 89.86%, 96.74% and 96.88%. ANOVA and post hoc Tukey HSD tests for significance were carried out for the above parameter. There was a statistically significant difference for T1 vs. T0 and T2 vs. T0 values [p < 0.05]. On comparison of T2 vs. T1 values, there was no statistically significant difference [p > 0.05], thus showing the stability of the result obtained by mandibular DO at 12 months post the distractor removal (Tables 5 and 6).
The mean pre-operative mouth opening at T0 and T1 was 4.64 mm. The mean post-ankylosis release mouth opening at T2 was 34.43 mm. The paired t test revealed that the increase in mouth opening was statistically significant [p < 0.05]. These findings are in accordance with the distraction first—release later protocol as already described previously) Table 4).
At the T0 interval, the questionnaire revealed that paediatric patients responded positively for Q1 [snoring] and Q2 [night time awakening] episodes. Only three patients of the paediatric group [T0 AHI 59.1, 100.5 and 117.7] responded positively for Q3 [day time somnolence] (Table 3).
At the T1 and T2 intervals, the questionnaire revealed that all subjects of the paediatric group reported complete resolution of night time awakening episodes and day time somnolence. Eleven subjects reported complete resolution of night time snoring. Three subjects reported positively for snoring at T1 and T2 intervals. These were the very same patients that reported with day time somnolence at the T0 interval. Furthermore, since their AHI values at the T1 and T2 intervals were more than 5, they continued to suffer from a mild form of OSA which was associated with some degree of snoring (Table 3).
Adult group
The mean mandibular advancement at T1 was 9.64 mm and at T2 was 9.36 mm. The paired t test for the above values revealed that there was no statistically significant difference [p > 0.05] between these values (Table 4, Figs. 4, 5 and 6).
The mean PAS width at T0, T1 and T2 was 5.18 mm [moderate narrowing], 10.09 mm [mild narrowing] and 10.91 mm [mild narrowing], respectively. ANOVA and post hoc Tukey HSD tests for significance were carried out for the above parameter. There was a statistically significant difference for T1 vs. T0 and T2 vs. T0 values [p < 0.05]. On comparison of T2 vs. T1 values, there was no statistically significant difference [p > 0.05] (Tables 5 and 6, Figs. 4, 5 and 6).
The mean AHI at T0, T1 and T2 was 31.45, 1.37 and 1.43, respectively. Friedman and post hoc Wilcoxon signed rank tests for significance were carried out for the above parameter. There was a statistically significant difference for T1 vs. T0 and T2 vs. T0 values [p < 0.05]. On comparison of T2 vs. T1 values, there was no statistically significant difference [p > 0.05]. As both the T1 and T2 AHI scores were lesser than 5 [AHI lesser than 5 is normal for adults], it indicated that the result obtained by mandibular DO was maintained at 12 months post the distractor removal [7] (Tables 5 and 6).
The mean SpO2 saturations at T0, T1 and T2 were 92.01, 96.80 and 96.84. ANOVA and post hoc Tukey HSD tests for significance were carried out for the above parameter. There was a statistically significant difference for T1 vs. T0 and T2 vs. T0 values [p < 0.05]. On comparison of T2 vs. T1 values, there was no statistically significant difference [p > 0.05] (Tables 5 and 6).
The mean pre-operative mouth opening at T0 and T1 was 5.18 mm. The mean post-ankylosis release mouth opening at T2 was 33.91 mm. The paired t test revealed that the increase in mouth opening was statistically significant [p < 0.05] (Table 4).
At the T0 interval, the questionnaire revealed that all adult patients responded positively for Q1 [snoring] and Q2 [night time awakening] episodes. None of the patients of the adult group responded positively for Q3 at the T0 interval (Table 3).
At the T1 and T2 intervals, the questionnaire revealed that all subjects of the adult group reported complete resolution of snoring, night time awakening episodes and day time somnolence (Table 3).
Inter-age group comparison of variables
Table 1 shows a comparison of the numerical variables between the age groups at T0, T1 and T2 time intervals using the independent t test for data with normal distribution and the Mann-Whitney U test for non-normal data. Majority of the variables were comparable to each other at all the time intervals with very few having a statistically significant difference between them.
The paediatric group T0 mean PAS width [3.57 mm] was lesser than that of the adult group [T0 mean PAS width 5.18 mm] and this difference was statistically significant [p < 0.05]. This could be attributed to the ongoing craniofacial growth in the paediatric group as compared to the already completed craniofacial growth in the adult group (Table 1).
The paediatric group T0 mean AHI [48.04] was greater than that of the adult group [T0 mean AHI 31.45]; however, this difference was not statistically significant [p > 0.05]. As per the literature, an AHI of > 30 is considered severe OSA in adult patients and an AHI of > 10 is considered severe OSA in paediatric patients (Table 1) [6, 7].
The paediatric group T1 mean AHI [3.41] was greater than that of the adult group [T1 mean AHI 1.37], and this difference was statistically significant [p < 0.05]. The paediatric group T2 mean AHI [3.60] was greater than that of the adult group [T2 mean AHI 1.43] and this difference was statistically significant [p < 0.05]. As per the literature, an AHI of less than 5 is considered benign/normal in adult patients and an AHI of 1–5 is considered mild OSA in paediatric patients (Table 1) [6, 7].
There was no statistically significant difference found between the age groups and the frequency of responses to the questionnaire using the Chi-square test [p > 0.05] (Table 3).
Follow up beyond T2 interval
Ten subjects maintained follow-up beyond the T2 interval, and their findings were summarised separately to avoid confounding the overall results of the study (Table 7).
Six paediatric subjects [mean age 14 years] followed up for a mean duration of 28 months post distractor removal and ankylosis release. The mean PAS width was 11.5 mm. The increase in the PAS width could be attributed to the craniofacial growth taking place in these subjects. The mouth opening, AHI and O2 saturation were maintained at 33.67 mm, 3 and 97.40%, respectively, and were comparable to the T2 interval findings (Table 7). Four adult subjects [mean age 21.25 years] followed up for a mean duration of 28.50 months post-distractor removal and ankylosis release. The mean PAS width, mouth opening, AHI and O2 saturation were maintained at 10 mm, 34.50 mm, 1.25 and 97.50%, respectively, and were comparable to the T2 interval findings. The above results indicate a stability of results maintained even 2 years after ankylosis release (Table 7).
Discussion
The American Academy of Sleep Medicine considers Continuous Positive Airway Pressure [CPAP] as the gold standard for the treatment of OSA. However, CPAP is limited by adherence issues. Furthermore, it is preferred for clinical scenarios with excessive/redundant tissue surrounding the airway as seen in obese patients [8].
When a patient suffers from a skeletal disharmony with a moderate to severe AHI, both of which are observed in TMJ ankylosis patients, surgical maxillo-mandibular advancement is considered the treatment of choice and can be achieved by conventional skeletal osteotomies or by distraction osteogenesis [DO] [9,10,11,12].
The abnormal mandibular anatomy in TMJ ankylosis patients significantly increases the difficulty of performing traditional skeletal osteotomies that are based on standard anatomical landmarks in normal mandibles. The need for large mandibular advancements increases the risk of relapse and incidence of inferior alveolar nerve damage. Hence, traditional skeletal osteotomies are less preferred in such cases [9,10,11,12].
Mandibular DO is preferred over traditional skeletal osteotomies when larger advancements [> 8 to 10 mm] are needed. The corticotomy is simple and can be easily performed on mandibles with an abnormal anatomy. The risk of relapse is lower on account of the slow adaptation of the soft tissue envelope to the gradual incremental mandibular advancement by distraction histogenesis. The risk of inferior alveolar nerve damage is lower. Bone grafting and the associated donor site morbidity can be avoided all together [12]. The effectiveness of mandibular DO for the correction of OSA in patients with micrognathia has been reported in the literature [13, 14].
As per the 2012 protocol by Andrade et al. [2], mandibular DO is performed prior to the TMJ ankylosis release in known cases of OSA. The subsequent increase of the PAS reduces or eliminates the underlying OSA. Once the TMJ is released, the enlarged airway space also helps reduce the risk of stimulation of the trigemino-cardiac reflex during active physiotherapy. Theoretically, this would lead to an increase in compliance to the post-operative jaw exercises thus reducing the risk of future re-ankylosis [2]. Mandibular DO after TMJ ankylosis release or simultaneous mandibular DO and TMJ ankylosis release are both not advisable due to the increased difficulty in DO vector control [as the proximal condyle bearing segment does not have a fixed stop post gap arthroplasty]. Simultaneous mandibular DO and TMJ ankylosis release also interferes with post-operative active physiotherapy [increased risk of damage to the distractor and the callous leading to undesirable outcomes] [14].
Majority of the ankylosis patients presented with a skeletal class 2 growth pattern and an increased overjet. At times, however, the expected increase in overjet was not encountered on account of naturally occurring dental compensations, e.g. the proclination of the mandibular anterior teeth. Under normal circumstances, pre-surgical orthodontics would have been performed to correct pre-existing dental compensations which would increase the overjet and create additional space for distraction. In our study, mandibular DO was performed prior to TMJ ankylosis release. Hence, the mouth remained closed during the distraction procedure and pre-surgical orthodontics could not be performed, which ultimately limited the amount of distraction. The presence of occlusal interferences on account of the severe crowding and malalignment also limited the amount of distraction. In certain situations, coronoplasty or extraction [only if grossly carious] of the interfering teeth had be considered. These can be considered as the limitations of the protocol given by Andrade et al. However, considering that the risk of re-ankylosis is reduced when following the protocol, we consider it to be the optimal line of treatment [2].
The results of the above study show that there was a statistically significant increase in the PAS width and the SpO2 on account of the mandibular advancement. There was a statistically significant drop in the AHI and a marked resolution of the OSA. The parameters measured at the T2 interval show that the results of mandibular DO were fairly stable at 12 months post-distractor removal. These clinical findings were similarly reflected in the conducted questionnaires. Mouth opening at T2 was adequate and considered a significant improvement to the mean pre-operative mouth opening. The patients also showed compliance with physiotherapy at the T2 interval and no evidence of re-ankylosis was present. Table 1 also shows that the results achieved were comparable between both age groups and pre-arthroplastic mandibular DO can be considered a valid tool in the management of triad TMJ ankylosis patients across age groups. An added advantage of pre-arthroplastic mandibular DO is the improvement in the facial profile prior to ankylosis release which can be a motivating factor for both the subjects and their families to undergo further treatment.
Ten out of 25 subjects followed up beyond the T2 interval [28-month mean follow-up duration beyond ankylosis release]. The parameters measured at this interval also reflect similar stability of results. However, on account of majority of the subjects being lost to follow-up, only descriptive statistical analysis of the same could be performed.
The primary drawback of our study was the limited follow-up duration. This short duration cannot be used to completely rule out the risk of re-ankylosis. However, the few subjects that did follow up beyond the T2 interval maintained an AHI value and mouth opening similar to that of the T2 interval which can be considered to be a positive indicator of the efficacy of pre-arthroplastic distraction in such cases. The study also had a small sample size on account of the rarity of triad TMJ ankylosis patients.
Every surgical modality has its own set of limitations. The distraction process is a long, staged surgical procedure with multiple prolonged hospital stays. This increases the medical risk undertaken by the patient and also further drives up the costs of the overall procedure. Linear distractors are disadvantaged by the inability to change the vector of distraction during the procedure. The distractors are also subject to hardware failure during the distraction process and the consolidation period as well. A similar complication was noted in one case during the distraction process and the failed distractor was replaced under general anaesthesia. When distractor activation ports are introduced intra-orally, the risk of infection also increases significantly. This complication was noted in three of our patients and was managed conservatively with a course of intra-venous antibiotics. The hygiene and patency of the intra-oral port were maintained by daily flushing with a diluted betadine solution and packing the region surrounding the port with chlorhexidine impregnated sofra-tulle. The infection did not affect the fate of the callous and the eventual bone regenerate that formed.
Conclusion
Our study proves that mandibular body distraction ostegenesis, prior to TMJ ankylosis release, successfully resolves OSA by increasing the PAS width. The results of our study were stable in the short term and a limited number of cases presented with similarly stable results in the medium term as well. There is also evidence in the literature that the correction of the narrow PAS helps increase compliance to jaw physiotherapy which may theoretically reduce the risk of future re-ankylosis. Lastly, the accompanying improvement in facial aesthetics following distraction is a motivating factor for such patients.
References
Movahed R, Mercuri LG (2015) Management of Temporomandibular Joint Ankylosis. Oral Maxillofac Surg Clin North Am 27(1):27–35
Andrade NN, Kalra R, Shetye SP (2012) New protocol to prevent TMJ reankylosis and potentially life threatening complications in triad patients. Int J Oral Maxillofac Surg 41(12):1495–1500
Madani M, Madani F (2007 Sep) The pandemic of obesity and its relationship to sleep apnea. Atlas Oral Maxillofac Surg Clin North Am 15(2):81–88
Al-Moraissi EA, El-Sharkawy TM, Mounair RM, El-Ghareeb TI (2015) A systematic review and meta-analysis of the clinical outcomes for various surgical modalities in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg 44(4):470–482
Dimitroulis G (2011) A critical review of interpositional grafts following temporomandibular joint discectomy with an overview of the dermis-fat graft. Int J Oral Maxillofac Surg 40(6):561–568
Dehlink E, Tan H-L (2016) Update on paediatric obstructive sleep apnoea. J Thorac Dis 8(2):224–235
Madani M, Madani F (2007) Definitions, abbreviations, and acronyms of sleep apnea. Atlas Oral Maxillofac Surg Clin North Am 15(2):69–80
Spicuzza L, Caruso D, Di Maria G (2015) Obstructive sleep apnoea syndrome and its management. Ther Adv Chronic Dis 6(5):273–285
Ephros HD, Madani M, Geller BM, Defalco RJ (2007) Developing a protocol for the surgical management of snoring and obstructive sleep apnea. Atlas Oral Maxillofac Surg Clin North Am 15(2):89–100
Boyd SB (2009) Management of obstructive sleep apnea by maxillomandibular advancement. Oral Maxillofac Surg Clin North Am 21(4):447–457
Weaver TE, Sawyer A (2009) Management of obstructive sleep apnea by continuous positive airway pressure. Oral Maxillofac Surg Clin North Am 21(4):403–412
Bouchard C, Troulis MJ, Kaban LB (2009) Management of obstructive sleep apnea: role of distraction osteogenesis. Oral Maxillofac Surg Clin North Am 21(4):459–475
Wang X, Wang X-X, Liang C, Yi B, Lin Y, Li Z-L (2003) Distraction osteogenesis in correction of micrognathia accompanying obstructive sleep apnea syndrome. Plast Reconstr Surg 112(6):1549–1557 discussion 1558-9
Anantanarayanan P, Narayanan V, Manikandhan R, Kumar D (2008) Primary mandibular distraction for management of nocturnal desaturations secondary to temporomandibular joint (TMJ) ankylosis. Int J Pediatr Otorhinolaryngol 72(3):385–389
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics committee approval
Obtained from the Institutional Ethics Committee [EC/004/2011].
Informed consent
Obtained.
Rights and permissions
About this article
Cite this article
Andrade, N.N., Mathai, P.C., Ganapathy, S. et al. Pre-arthroplastic mandibular distraction osteogenesis for the correction of OSA in TMJ ankylosis: a prospective observational study of 25 cases. Oral Maxillofac Surg 22, 409–418 (2018). https://doi.org/10.1007/s10006-018-0722-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-018-0722-x