Abstract
Purpose
Studies on preemptive analgesia in maxillofacial surgery have shown several controversial clinical results, mainly due to the absence of a methodological standard, besides a wide variety of studied drugs. This study intended to answer the following hypothesis: Is the administration of dipyrone preemptively capable of decreasing trans- and postoperative pain in the third molar surgical extraction?
Methods
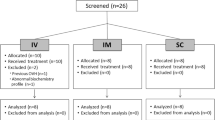
A pilot prospective double-blind placebo-controlled study was carried out with 25 patients submitted to the third molar surgical extraction at two moments, one side in each intervention. Dipyrone (1 g) was preemptively administered (study group) for the extraction of two third molars on the same side and, in a second surgical procedure, dipyrone (1 g) was administered in the immediate postoperative period (control group). Evaluated variables were the amount of anesthetic, pain perceived through the visual analogue scale (VAS) in transoperative and immediate postoperative periods, and over 12-h investigation period, analgesic consumption, duration of surgery, and time to rescue analgesia.
Results
The results were submitted to Student’s t test and statistical differences were observed in transoperative (p < 0.05) and immediate postoperative (p < 0.01) periods, while the other studied variables did not present statistical differences.
Conclusion
The preemptive administration of dipyrone decreased the perception of transoperative and immediate postoperative pain when compared to its use after surgery only.


Similar content being viewed by others
References
Bromley L (2006) Pre-emptive analgesia and protective premedication. What is the difference? Biomed Pharmacother 60(7):336–340. https://doi.org/10.1016/j.biopha.2006.06.012
Gottschalk A, Smith DS (2001) New concepts in acute pain therapy: preemptive analgesia. Am Fam Physician 63(10):1979–1984
Bauer HC, Duarte FL, Horliana AC, Tortamano IP, Perez FE, Simone JL, Jorge WA (2013) Assessment of preemptive analgesia with ibuprofen coadministered or not with dexamethasone in third molar surgery: a randomized double-blind controlled clinical trial. Oral Maxillofac Surg 17(3):165–171. https://doi.org/10.1007/s10006-012-0360-7
Ong CKS, Lirk P, Seymour RA, Jenkins BJ (2005) The efficacy of preemptive analgesia for acute postoperative pain management: a meta-analysis. Anesth Analg 100(3):757–773. https://doi.org/10.1213/01.ANE.0000144428.98767.0E
Savage MG, Henry MA, Colo D (2004) Preoperative nonsteroidal anti-inflammatory agents: review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 98(2):146–152. https://doi.org/10.1016/j.tripleo.2004.01.012
Jung YS, Kim MK, Um YJ, Park HS, Lee EW, Kang JW (2005) The effects on postoperative oral surgery pain by varying NSAID administration times: comparison on effect of preemptive analgesia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 100(5):559–563. https://doi.org/10.1016/j.tripleo.2005.02.065
Gutta R, Koehn CR, James LE (2013) Does ketorolac have a preemptive analgesic effect? A randomized, double-blind, control study. J Oral Maxillofac Surg 71(12):2029–2034. https://doi.org/10.1016/j.joms.2013.06.220
Cavalcanti IL, Cantinho FAF, Assad A. Medicina Perioperatória (2006). Rio de Janeiro: Sociedade de Anestesiologia do Estado do Rio de Janeiro, 1107–23
Neupert EA, Lee JW, Philput CB, Gordon JR (1992) Evaluation of dexamethasone for reduction of postsurgical sequelae of third molar removal. J Oral Maxillofac Surg 50(11):1177–1182. https://doi.org/10.1016/0278-2391(92)90149-T
Alcantara CEP, Falci SGM, Ferreira FO, Santos CRR, Pinheiro MLP (2014) Pre-emptive effect of dexamethasone and methylprednisolone on pain, swelling, and trismus after third molar surgery: a split-mouth randomized triple-blind clinical trial. Int J Oral Maxillofac Surg 43(1):93–98. https://doi.org/10.1016/j.ijom.2013.05.016
Ong KS, Seymour RA, Chen FG, Ho VCL (2004) Preoperative ketorolac has a preemptive effect for postoperative third molar surgical pain. Int J Oral Maxillofac Surg 33(8):771–776. https://doi.org/10.1016/j.ijom.2004.01.020
Ong KS, Tan JML (2004) Preoperative intravenous tramadol versus ketorolac for preventing postoperative pain after third molar surgery. Int J Oral Maxillofac Surg 33(3):274–278. https://doi.org/10.1006/ijom.2003.0515
Kaczmarzyk T, Wichlinski J, Stypulkowska J, Zaleska M, Woron J (2010) Preemptive effect of ketoprofen on postoperative pain following third molar surgery. A prospective, randomized, double-blinded clinical trial. Int J Oral Maxillofac Surg 39(7):647–652. https://doi.org/10.1016/j.ijom.2010.02.019
Bridgman JB, Gillgrass TG, Zacharias M (1996) The absence of any pre-emptive analgesic effect for non-steroidal anti-inflammatory drugs. Br J Oral Maxillofac Surg 34(5):428–431. https://doi.org/10.1016/S0266-4356(96)90101-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Favarini, V.T., Lima, C.A.A., da Silva, R.A. et al. Is dipyrone effective as a preemptive analgesic in third molar surgery? A pilot study. Oral Maxillofac Surg 22, 71–75 (2018). https://doi.org/10.1007/s10006-018-0669-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-018-0669-y