Abstract
Purpose
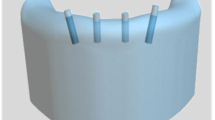
We will aim to develop implants made of a Ni-Ti shape memory alloy which can be applied for the treatment of midface fractures, such as isolated orbital floor fractures. These can then be implanted in a compressed form and unfold automatically in the body. With the help of newly developed application instruments, the implants can be applied along transnasal and transantral approaches into the maxillary sinus. Our objective is to evaluate the operation process and the functionality of these implants, already in a pre-investigation by an experienced surgeon on a phantom.
Methods
The functionality of the surgical procedure and an implant prototype were both evaluated with the help of a realistic phantom. The minimally invasive application was carried out using the transnasal and transantral approach. Instruments and implant were rated individually on a scale, from −2 (not at all) to +2 (very good) for vaious criteria, such as the implants functionality or the ergonomics of the entire procedure. For a geometric comparison between the manufactured implant and the planned target geometry, the implants were scanned by micro-computed tomography. CAD models were derived from the scans by using reverse engineering.
Results
Both the implants and the application procedure were assessed as good; thus, the implant concept is suitable for further development.
Conclusions
Implants made of shape memory alloys could allow in the future and allow less invasive access to treat orbital floor fractures. The implant design has to be modified that the implant can be stabilized and fixed with screws or a suture to avoid dislocation or implant loosening. The complication rates and risks of conventional orbital reconstructions should be lowered by this new method.






Similar content being viewed by others
References
Neff A, Rasse M, Prein J (2013) Die neue AO-CMF-Traumaklassifikation für Erwachsene–Überblick, Präzisions-Level und anatomische Module für Unterkiefer, Kiefergelenkfortsätze, Mittelgesicht und Orbita. OP-Journal 29:109–128
Bartoli D, Fadda MT, Battisti A et al (2015) Retrospective analysis of 301 patients with orbital floor fracture. J Cranio-Maxillofac Surg 43(2):244–247. doi:10.1016/j.jcms.2014.11.015
Nitsche T, Essig H, Wiltfang J, Mohr C (2013) S2e-Leitlinie: Rekonstruktion von Orbitadefekten. AWMF online
Baino F (2011) Biomaterials and implants for orbital floor repair. Acta Biomater 7(9):3248–3266. doi:10.1016/j.actbio.2011.05.016
de Riu G, Meloni SM, Gobbi R, Soma D, Baj A, Tullio A (2008) Subciliary versus swinging eyelid approach to the orbital floor. J Cranio-Maxillofac Surg 36(8):439–442. doi:10.1016/j.jcms.2008.07.005
Baumann A, Ewers R (2001) Use of the preseptal transconjunctival approach in orbit reconstruction surgery. J Oral Maxillofac Surg 59(3):287–291. doi:10.1053/joms.2001.20997
Kushner GM (2006) Surgical approaches to the infraorbital rim and orbital floor: the case for the transconjunctival approach. J Oral Maxillofac Surg 64(1):108–110
Hundepool AC, Willemsen MAP, Koudstaal MJ, van der Wal KGH (2012) Open reduction versus endoscopically controlled reconstruction of orbital floor fractures: a retrospective analysis. Int J Oral Maxillofac Surg 41(4):489–493. doi:10.1016/j.ijom.2012.01.006
Gander T, Essig H, Metzler P et al (2015) Patient specific implants (PSI) in reconstruction of orbital floor and wall fractures. J Cranio-Maxillofac Surg 43(1):126–130. doi:10.1016/j.jcms.2014.10.024
Holck DEE, Boyd EM, Ng J, Mauffray RO (1999) Benefits of stereolithography in orbital reconstruction. Ophthalmology 106(6):1214–1218
Klein A, Langmann G, Langmann A, Santler G (2002) CT-based three-dimensional patient models for reconstruction of sever orbital fracture. Eur Surg 34(2):33–35. doi:10.1007/BF02947628
Kumar PK, Lagoudas DC (2008) Introduction to Shape Memory Alloys. In: Shape memory alloys: modeling and engineering applications. Springer US, Boston
Morgan NB (2004) Medical shape memory alloy applications—the market and its products. Mater Sci Eng A 378(1):16–23
Petrini L, Migliavacca F (2011) Biomedical applications of shape memory alloys. J Metall. doi:10.1155/2011/501483
Mantovani D (2000) Shape memory alloys: properties and biomedical applications. JOM 52(10):36–44
Trepanier C, Venugopalan R, Pelton AR (2000) Corrosion resistance and biocompatibility of passivated NiTi. Shape Memory Implants 35–45. doi:10.1007/978-3-642-59768-8_3
Wever DJ, Veldhuizen AG, Sanders MM, Schakenraad JM, van Horn JR (1997) Cytotoxic, allergic and genotoxic activity of a nickel-titanium alloy. Biomaterials 18(16):1115–1120
Acknowledgements
The authors greatly acknowledge Casper Thorpe-Lowis for proofreading the paper as a native speaker.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The research project 13GW0017F was funded by the Federal Ministry of Education and Research within the “KMU-innovativ” funding programme.
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This article does not contain any studies with human participants or animals.
Rights and permissions
About this article
Cite this article
Grunert, R., Wagner, M., Rotsch, C. et al. Concept of patient-specific shape memory implants for the treatment of orbital floor fractures. Oral Maxillofac Surg 21, 179–185 (2017). https://doi.org/10.1007/s10006-017-0615-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-017-0615-4