Abstract
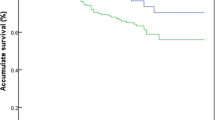
The purpose of this study was to assess the clinicopathological features of oropharyngeal cancer patients in Jordan based on their HPV status. Sixty-nine biopsies from two hospitals were included. Tissue microarrays were prepared from formalin-fixed paraffin-embedded (FFPE) specimens and stained with antibodies for CDKN2A/P16, EGFR, PI3K, PTEN, AKT, pS473AKT, PS2mTOR, and TIMAP. The cohort was divided according to P16 expression. Chi-square test and survival analyses were employed to evaluate the variations among the study variables and determine the prognostic factors, respectively. P16 expression was found in 55.1% of patients; however, there was no significant association between P16 expression and the patients’ clinicopathological features. The Kaplan–Meier test revealed that smoking in P16-positive group and younger age (< 58 years) negatively impacted disease-free survival (DFS) (P = 0.04 and P = 0.003, respectively). Multivariate Cox regression test indicated that smoking, age, PI3K, and AKT were negative predictors of DFS (P = 0.021, P = 0.002, P = 0.021, and P = 0.009, respectively), while TIMAP was a positive predictor (P = 0.045). Elevated P16 expression is found in more than half of the patients’ specimens. DFS is negatively affected by younger age and the combined effect of smoking and P16 overexpression. TIMAP is overexpressed in P16-positive oropharyngeal cancer, and it is a favorable predictor of DFS.



Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Park JO, Nam IC, Kim CS, Park SJ, Lee DH, Kim HB et al (2022) Sex differences in the prevalence of head and neck cancers: a 10-year follow-up study of 10 million healthy people. Cancers (Basel). 14(10):2521
Gillison ML, Koch WM, Capone RB, Spafford M, Westra WH, Wu L et al (2000) Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst 92(9):709–720
Baron AE, Franceschi S, Barra S, Talamini R, La Vecchia C (1993) A comparison of the joint effects of alcohol and smoking on the risk of cancer across sites in the upper aerodigestive tract. Cancer Epidemiol Biomarkers Prev. 2(6):519–523
Chen AM, Zahra T, Daly ME, Farwell DG, Luu Q, Gandour-Edwards R et al (2013) Definitive radiation therapy without chemotherapy for human papillomavirus-positive head and neck cancer. Head Neck 35(11):1652–1656
Smolensky D, Rathore K, Bourn J, Cekanova M (2017) Inhibition of the PI3K/AKT pathway sensitizes oral squamous cell carcinoma cells to anthracycline-based chemotherapy in vitro. J Cell Biochem 118(9):2615–2624
Laimer K, Spizzo G, Gastl G, Obrist P, Brunhuber T, Fong D et al (2007) High EGFR expression predicts poor prognosis in patients with squamous cell carcinoma of the oral cavity and oropharynx: a TMA-based immunohistochemical analysis. Oral Oncol 43(2):193–198
Hay N, Sonenberg N (2004) Upstream and downstream of mTOR. Genes Dev 18(16):1926–1945
Bussink J, van der Kogel AJ, Kaanders JHAM (2008) Activation of the PI3-K/AKT pathway and implications for radioresistance mechanisms in head and neck cancer. Lancet Oncol 9(3):288–296
Xie Ming S, Shen Jia L, Yin C, Ruan P, Yao X (2006) Expression of tumor suppressor gene PTEN, PIP3 and cyclin D1 in oral squamous cell carcinoma and their correlations. Zhonghua Kou Qiang Yi Xue Za Zhi. 41(7):407–410
Shashidhar K, Basti S, Swarnamba UN, Ajur S (2022) Surrogate marker P16 in oral/oropharyngeal carcinoma. Int J Health Sci Qassim. https://doi.org/10.53730/ijhs.v6nS4.12275
Cairns P, Polascik TJ, Eby Y, Tokino K, Califano J, Merlo A et al (1995) Frequency of homozygous deletion at p16/CDKN2 in primary human tumours. Nat Genet 11(2):210–212
Moharil R, Khandekar S, Dive A, Bodhade A (2020) Cyclin D1 in oral premalignant lesions and oral squamous cell carcinoma: an immunohistochemical study. J Oral Maxillofac Pathol. 24(2):397
Obeidat M, Bodoor K, Alqudah M, Masaadeh A, Barukba M, Almomani R (2021) TIMAP upregulation correlates negatively with survival in HER2- negative subtypes of breast cancer. Asian Pac J Cancer Prev 22(6):1899–1905
PPP1R16B protein expression summary-the human protein atlas
Obeidat M, Li L, Ballermann BJ (2014) TIMAP promotes angiogenesis by suppressing PTEN-mediated Akt inhibition in human glomerular endothelial cells. Am J Physiol Renal Physiol. https://doi.org/10.1152/ajprenal.00070.2014
Yang J, Yin S, Bi F, Liu L, Qin T, Wang H et al (2017) TIMAP repression by TGFβ and HDAC3-associated Smad signaling regulates macrophage M2 phenotypic phagocytosis. J Mol Med. https://doi.org/10.1007/s00109-016-1479-z
Csortos C, Czikora I, Bogatcheva NV, Adyshev DM, Poirier C, Olah G et al (2008) TIMAP is a positive regulator of pulmonary endothelial barrier function. Am J Physiol Lung Cell Mol Physiol. https://doi.org/10.1152/ajplung.00325.2007
Abdel-razeq H, Attiga F, Mansour A (2015) Cancer care in Jordan. Hematol Oncol Stem Cell Ther 8(2):64–70
Shukr B, Bartelli D, Ward KD, Ray M, Maziak W, Mzayek F (2023) The effect of exposure to tobacco smoking-related media messages on youths’ smoking behavior in Jordan: a longitudinal, school-based study. Prev Med (Baltim). 166:107386
Bodoor K, Almomani R, Alqudah M, Haddad Y, Samouri W (2020) LAT1 (SLC7A5) overexpression in negative her2 group of breast cancer: a potential therapy target. Asian Pacific J Cancer Prev. https://doi.org/10.31557/APJCP.2020.21.5.1453
Lydiatt WM, Patel SG, Osullivan B, Brandwein MS, Ridge JA, Migliacci JC et al (2017) Head and neck cancers—major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J Clin. 67(2):122
Vazquez-Guillen JM, Palacios-Saucedo GC, Alanis-Valdez AY, Huerta-Escobedo A, Zavala-Pompa A, Rivera-Morales LG et al (2023) p16INK4a and pRb expression in laryngeal squamous cell carcinoma with and without infection by EBV or different genotypes of HPV: a retrospective study. Infect Agent Cancer. https://doi.org/10.1186/s13027-023-00514-x
Khanna S, Palackdharry S, Roof L, Wicker CA, Mark J, Zhu Z et al (2020) Determining the molecular landscape and impact on prognosis in HPV-associated head and neck cancer. Cancers Head Neck. https://doi.org/10.1186/s41199-020-00058-2
Wendt M, Hammarstedt-Nordenvall L, Zupancic M, Friesland S, Landin D, Munck-Wikland E et al (2021) Long-term survival and recurrence in oropharyngeal squamous cell carcinoma in relation to subsites, HPV, and p16-status. Cancers (Basel). 13(11):2553
Bixofis RB, Sassi LM, Patussi C, Jung JE, Ioshii SO, Schussel JL (2014) Significance of p16 positive expression in oropharyngeal cancers. Asian Pacific J Cancer Prev. 15(23):10289
Ukpo OC, Flanagan JJ, Ma XJ, Luo Y, Thorstad WL, Lewis JS (2011) High-risk human papillomavirus E6/E7 mRNA detection by a novel in situ hybridization assay strongly correlates with p16 expression and patient outcomes in oropharyngeal squamous cell carcinoma. Am J Surg Pathol. 35(9):1343–50. https://doi.org/10.1097/pas.0b013e318220e59d
Yamashita Y, Ikegami T, Hirakawa H, Uehara T, Deng Z, Agena S et al (2019) Staging and prognosis of oropharyngeal carcinoma according to the 8th Edition of the American Joint Committee on Cancer Staging Manual in human papillomavirus infection. Eur Arch Otorhinolaryngol. 276(3):827–836
AJCC (2020) AJCC Cancer Staging Manual 8th Edition. In: Definitions [Internet]. Qeios. https://doi.org/10.32388/b30ldk
Alsbeih G, Al-Harbi N, Bin Judia S, Al-Qahtani W, Khoja H, El-Sebaie M et al (2019) Prevalence of human papillomavirus (HPV) infection and the association with survival in Saudi patients with head and neck squamous cell carcinoma. Cancers (Basel). 11(6):820
Hanna GJ, Kacew A, Chau NG, Shivdasani P, Lorch JH, Uppaluri R et al (2018) Improved outcomes in PI3K-pathway-altered metastatic HPV oropharyngeal cancer. JCI Insight. 3(17):e122799
Kwon HJ, Brasch HD, Benison S, Marsh RW, Itinteang T, Titchener GW et al (2016) Changing prevalence and treatment outcomes of patients with p16 human papillomavirus related oropharyngeal squamous cell carcinoma in New Zealand. Br J Oral Maxillofac Surg. 54(8):898–903. https://doi.org/10.1016/j.bjoms.2016.05.033
Berman TA, Schiller JT (2017) Human papillomavirus in cervical cancer and oropharyngeal cancer: one cause, two diseases. Cancer. 123:2219
Carlander AF, Jakobsen KK, Bendtsen SK, Garset-Zamani M, Lynggaard CD, Jensen JS et al (2021) A contemporary systematic review on repartition of HPV-positivity in oropharyngeal cancer worldwide. Viruses. 13(7):1326
Goulart J, Hay J, Thomson T (2009) 102 the prognostic value of P16 status in advanced stage oropharyngeal carcinoma according to treatment regime. Radiother Oncol. 92:S33. https://doi.org/10.1016/s0167-8140(12)72489-1
Sinha P, Karadaghy OA, Doering MM, Tuuli MG, Jackson RS, Haughey BH (2018) Survival for HPV-positive oropharyngeal squamous cell carcinoma with surgical versus non-surgical treatment approach: a systematic review and meta-analysis. Oral Oncol. 86:121–131. https://doi.org/10.1016/j.oraloncology.2018.09.018
Lewis JS Jr, Thorstad WL, Chernock RD, Haughey BH, Yip JH, Zhang Q et al (2010) p16 positive oropharyngeal squamous cell carcinoma: an entity with a favorable prognosis regardless of tumor HPV status. Am J Surg Pathol. 34(8):1088–1096
Culié D, Lisan Q, Leroy C, Modesto A, Schiappa R, Chamorey E et al (2021) Oropharyngeal cancer: first relapse description and prognostic factor of salvage treatment according to p16 status, a GETTEC multicentric study. Eur J Cancer. 143:168–177. https://doi.org/10.1016/j.ejca.2020.10.034
Anantharaman D, Muller DC, Lagiou P, Ahrens W, Holcátová I, Merletti F et al (2016) Combined effects of smoking and HPV16 in oropharyngeal cancer. Int J Epidemiol. 45(3):752
Bouland C, Dequanter D, Lechien JR, Hanssens C, De Saint Aubain N, Digonnet A et al (2021) Prognostic significance of a scoring system combining p16, smoking, and drinking status in a series of 131 patients with oropharyngeal cancers. Int J Otolaryngol. https://doi.org/10.1155/2021/8020826
Mehanna H, Taberna M, von Buchwald C, Tous S, Brooks J, Mena M et al (2023) Prognostic implications of p16 and HPV discordance in oropharyngeal cancer (HNCIG-EPIC-OPC): a multicentre, multinational, individual patient data analysis. Lancet Oncol. 24(3):239
Dahlstrom KR, Song J, Thall PF, Fuller CD, Hutcheson KA, Johnson FM et al (2021) Conditional survival among patients with oropharyngeal cancer treated with radiation therapy and alive without recurrence 5 years after diagnosis. Cancer. 127(8):1228–1237
Lai YH, Su CC, Wu SY, Hsueh WT, Wu YH, Chen HHW et al (2022) Impact of alcohol and smoking on outcomes of HPV-related oropharyngeal cancer. J Clin Med. 11(21):6510
Bar Ad V, Wang Z, Mishra M, Ahn P, Cognetti D, Curry J et al (2011) Combination of p16 levels and pre-radiotherapy factors predict for outcome in patients treated for oropharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 81(2):S500–S501. https://doi.org/10.1016/j.ijrobp.2011.06.1022
Lassen P, Eriksen JG, Hamilton-Dutoit S, Tramm T, Alsner J, Overgaard J (2009) Effect of HPV-associated p16INK4A expression on response to radiotherapy and survival in squamous cell carcinoma of the head and neck. J Clin Oncol. 27(12):1992–1998. https://doi.org/10.1200/jco.2008.20.2853
Gillison ML, D’Souza G, Westra W, Sugar E, Xiao W, Begum S et al (2008) Distinct risk factor profiles for human papillomavirus type 16–positive and human papillomavirus type 16–negative head and neck cancers. J Natl Cancer Inst. 100(6):407–20. https://doi.org/10.1093/jnci/djn025
Kelly JR, An Y, Park HSM, Yarbrough W, Burtness BA, Husain ZA (2017) Survival Outcomes Among Human Papillomavirus-Associated Oropharyngeal Squamous Cell Cancer Patients Treated with Upfront Surgery Versus Definitive Chemoradiation Therapy. Int J Radiat Oncol Biol Phys. 99(2):S43–S44. https://doi.org/10.1016/j.ijrobp.2017.06.114
Panda S, Mohanty N, Panda S, Mishra L, Gopinath D, Sahoo A et al (2022) Are survival outcomes different for young and old patients with oral and oropharyngeal squamous cell carcinoma? A systematic review and meta-analysis. Cancers (Basel). 14(8):1886
Choi I, Lee D, Son K, Bae S (2020) Incidence, cost and gender differences of oropharyngeal and noncervical anogenital cancers in South Korea [Internet]. Research Square Platform LLC. https://doi.org/10.21203/rs.2.23463/v1
Simpson DR, Mell LK, Cohen EEW (2015) Targeting the PI3K/AKT/mTOR pathway in squamous cell carcinoma of the head and neck. Oral Oncol. 51(4):291–8. https://doi.org/10.1016/j.oraloncology.2014.11.012
Janecka-Widła A, Majchrzyk K, Mucha-Małecka A, Biesaga B (2021) EGFR/PI3K/Akt/mTOR pathway in head and neck squamous cell carcinoma patients with different HPV status. Polish J Pathol. 72(4):296–314. https://doi.org/10.5114/pjp.2021.113073
García-Carracedo D, Villaronga MÁ, Álvarez-Teijeiro S, Hermida-Prado F, Santamaría I, Allonca E et al (2016) Impact of PI3K/AKT/mTOR pathway activation on the prognosis of patients with head and neck squamous cell carcinomas. Oncotarget [Internet]. 7(20):29780–93
Iglesias-Bartolome R, Martin D, Gutkind JS (2013) Exploiting the head and neck cancer oncogenome: widespread PI3K-mTOR pathway alterations and novel molecular targets. Cancer Discov. 3(7):722–5
Won HS, Jung CK, Chun SH, Kang JH, Kim YS, Sun DI et al (2012) Difference in expression of EGFR, pAkt, and PTEN between oropharyngeal and oral cavity squamous cell carcinoma. Oral Oncol. 48(10):985–90. https://doi.org/10.1016/j.oraloncology.2012.04.013
Chun SH, Jung CK, Won HS, Kang JH, Kim YS, Kim MS (2014) Divergence of P53, PTEN, PI3K, Akt and mTOR expression in tonsillar cancer. Head Neck. 37(5):636–43. https://doi.org/10.1002/hed.23643
Weber SM, Lu S, Wang XJ (2006) 08:00 AM: alterations in the PI3K/AKT pathway in head and neck cancer. Otolaryngol Head Neck Surg. 135(2):P85. https://doi.org/10.1016/j.otohns.2006.06.499
Larque AB, Conde L, Hakim S, Alos L, Jares P, Vilaseca I et al (2015) p16INK4a overexpression is associated with CDKN2A mutation and worse prognosis in HPV-negative laryngeal squamous cell carcinomas. Virchows Archiv. 466(4):375–82. https://doi.org/10.1007/s00428-015-1725-8
Lassen P, Overgaard J, Eriksen JG (2013) Expression of EGFR and HPV-associated p16 in oropharyngeal carcinoma: correlation and influence on prognosis after radiotherapy in the randomized DAHANCA 5 and 7 trials. Radiother Oncol. 108(3):489–94. https://doi.org/10.1016/j.radonc.2013.08.036
Kiessling SY, Broglie MA, Soltermann A, Huber GF, Stoeckli SJ (2018) Comparison of PI3K pathway in HPV-associated oropharyngeal cancer with and without tobacco exposure. Laryngoscope Investig Otolaryngol. 3(4):283–9
Horn D, Freudlsperger C, Holzinger D, Kunzmann K, Plinkert P, Dyckhoff G et al (2017) Upregulation of pAKT(Ser473) expression in progression of HPV-positive oropharyngeal squamous cell carcinoma. Head Neck. 39(12):2397–405. https://doi.org/10.1002/hed.24910
Obeidat M, Bodoor K, Alqudah M, Masaadeh A, Barukba M, Almomani R (2021) TIMAP upregulation correlates negatively with survival in HER2-negative subtypes of breast cancer. Asian Pac J Cancer Prev. 22(6):1899–1905 https://doi.org/10.31557/APJCP.2021.22.6.1899
Funding
Deanship of Scientific Research,Jordan university of science and technology.
Author information
Authors and Affiliations
Contributions
Conceptualization: MO, WA, and KB; data curation: MO; formal analysis: MO; investigation, MB, IM, FB, and SB; methodology: MO; resources: MO, SB, and WA; validation: MO, KB, SB, and WA; writing––original draft: MO, MB, and WA; Writing––review and editing: MO, KB, and WA.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Obeidat, M., Algargaz, W., Barukba, M. et al. Clinical and molecular characteristics of Jordanian oropharyngeal cancer patients according to P16 expression: a retrospective study and a report of a novel biomarker. Med Mol Morphol (2024). https://doi.org/10.1007/s00795-024-00383-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00795-024-00383-2