Abstract
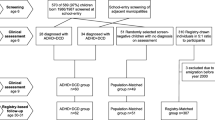
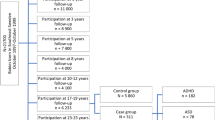
Studies have identified a higher prevalence of co-existing psychiatric and medical disorders in children with ADHD. There is a shortage of longitudinal studies providing an overview of potential medical disorders in children with ADHD. The objective of this study was to provide a broad overview of lifetime prevalence and relative risk of medical disorders in a nationwide Danish cohort of children with and without ADHD during the first 12 years of life. A population-based prospective follow-back cohort study used data from Danish national health registries to identify a cohort of all children born in Denmark between 1995 and 2002. The children were followed from birth until 12 years of age in two national registries. Children with ADHD had a significantly higher prevalence of recorded diagnoses across all included chapters of medical disorders in the ICD-10, except for neoplasms, where the association with ADHD was non-significant. The highest relative risk was observed for the chapter concerning diseases of the nervous system, with episodic and paroxysmal disorders being the most frequently registered underlying category. The findings indicate that children with ADHD have an increased risk of a broad range of medical disorders compared to the general population during the first 12 years of life, except for neoplasms.


Similar content being viewed by others
Abbreviations
- ADHD:
-
Attention-deficit hyperactivity disorder
- ADD:
-
Attention-deficit disorder
- DMBR:
-
Danish medical birth registry
- DPCRR:
-
Danish psychiatric central research register
- DNPR:
-
Danish national patient register
- ICD-10:
-
International classification of diseases 10th-edition
- RR:
-
Relative risk
- CI:
-
Confidence interval
References
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007) The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 164:942–948. https://doi.org/10.1176/ajp.2007.164.6.942
Thomas R, Sanders S, Doust J, Beller E, Glasziou P (2015) Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pedeatrics 135:e994-1001. https://doi.org/10.1542/peds.2014-3482
Leibson CL (2001) Use and costs of medical care for children and adolescents with and without attention-deficit/hyperactivity disorder. JAMA 285:60–66. https://doi.org/10.1001/jama.285.1.60
Efron D, Moisuc O, McKenzie V, Sciberras E (2016) Service use in children aged 6–8 years with attention deficit hyperactivity disorder. Arch Dis Child 101:161–165. https://doi.org/10.1136/archdischild-2015-309520
Silva D, Colvin L, Hagemann E, Stanley F, Bower C (2014) Children diagnosed with attention deficit disorder and their hospitalisations: population data linkage study. Eur Child Adolesc Psychiatry 23:1043–1050. https://doi.org/10.1007/s00787-014-0545-8
Laugesen B, Mohr-Jensen C, Boldsen SK et al (2018) Attention deficit hyperactivity disorder in childhood: healthcare use in a Danish birth cohort during the first 12 years of Life. J Pediatr 197:233–240. https://doi.org/10.1016/j.jpeds.2018.01.078
Mohr Jensen C, Hans-Christoph Steinhausen B (2014) Comorbid mental disorders in children and adolescents with attention-deficit/hyperactivity disorder in a large nationwide study. ADHD 7:27–38. https://doi.org/10.1007/s12402-014-0142-1
Larson K, Russ SA, Kahn RS, Halfon N (2011) Patterns of comorbidity, functioning, and service use for US children with ADHD, 2007. Pediatrics 127:462–470. https://doi.org/10.1542/peds.2010-0165
Nylander C, Fernell E, Tindberg Y (2015) Chronic conditions and coexisting ADHD—a complicated combination in adolescents. Eur J Pediatr 174:1209–1215. https://doi.org/10.1007/s00431-015-2521-9
Jameson ND, Sheppard BK, Lateef TM, Vande Voort JL, He JP, Merikangas KR (2016) Medical comorbidity of attention-deficit/hyperactivity disorder in US adolescents. J Child Neurol 31:1282–1289. https://doi.org/10.1177/0883073816653782
von Gontard A, Equit M (2015) Comorbidity of ADHD and incontinence in children. Eur Child Adolesc Psychiatry 24(2):127–140. https://doi.org/10.1007/s00787-014-0577-0
Muskens JB, Velders FP, Staal WG (2017) Medical comorbidities in children and adolescents with autism spectrum disorders and attention deficit hyperactivity disorders: a systematic review. Eur Child Adolesc Psychiatry 26:1093–1103. https://doi.org/10.1007/s00787-017-1020-0
Park KJ, Lee JS, Kim H-W (2017) Medical and psychiatric comorbidities in Korean children and adolescents with attention-deficit/hyperactivity disorder. Psychiatry Investig 14:817–824. https://doi.org/10.4306/pi.2017.14.6.817
Merikangas KR, Calkins ME, Burstein M et al (2015) Comorbidity of physical and mental disorders in the neurodevelopmental genomics cohort study. Pediatrics 135:e927–e938. https://doi.org/10.1542/peds.2014-1444
Nylander C, Tindberg Y, Haas J et al (2018) Self- and parent-reported executive problems in adolescents with type 1 diabetes are associated with poor metabolic control and low physical activity. Pediatr Diabetes 19:98–105. https://doi.org/10.1111/pedi.12520LK
Hilgard D, Konrad K, Meusers M et al (2017) Comorbidity of attention deficit hyperactivity disorder and type 1 diabetes in children and adolescents: analysis based on the multicentre DPV registry. Pediatr Diabetes 18:706–713. https://doi.org/10.1111/pedi.12431
Vinker-Shuster M, Golan-Cohen A, Merhasin I, Merzon E (2019) Attention-deficit hyperactivity disorder in pediatric patients with type 1 diabetes mellitus. J Dev Behav Pediatr 40:330–334. https://doi.org/10.1097/DBP.0000000000000670
Laugesen B, Lauritsen MB, Jørgensen R, Sørensen EE, Rasmussen P, Grønkjær M (2020) The complexities of everyday life and healthcare utilization in Danish children with ADHD: a mixed methods study. J Pediatr Nurs 52:33–41. https://doi.org/10.1016/j.pedn.2020.01.003
Pedersen CB, Gotzsche H, Moller JO, Mortensen PB (2006) The Danish civil registration system. A cohort of eight million persons. Dan Med Bull 53(4):441–449 (DMB3816 [pii])
Lynge E, Sandegaard JL, Rebolj M (2011) The Danish national patient register. Scand J Public Health 39:30–33. https://doi.org/10.1177/1403494811401482
Mors O, Perto GP, Mortensen PB (2011) The Danish psychiatric central research register. Scand J Public Health 39:54–57. https://doi.org/10.1177/1403494810395825
Pedersen CB (2011) The Danish civil registration system. Scand J Public Health 39:22–25. https://doi.org/10.1177/1403494810387965
World Health Organization (2016) http://www.who.int/en/. Published 2016.
WHO (1992) The ICD-10 Classification of mental and behavioural disorders clinical descriptions and diagnostic guidelines. World Health Organization, Geneva, p 1992
Lee SI, Schachar RJ, Chen SX, Ornstein TJ, Charach A, Barr C, Ickowicz A (2008) Predictive validity of DSM-IV and ICD-10 criteria for ADHD and hyperkinetic disorder. J Child Psychol Psychiatry 49:70–78. https://doi.org/10.1111/j.1469-7610.2007.01784.x
Dalsgaard S, Leckman JF, Mortensen PB, Nielsen HS, Simonsen M (2015) Effect of drugs on the risk of injuries in children with attention deficit hyperactivity disorder: prospective cohort study. Lancet Psychiatry 2:702–709. https://doi.org/10.1016/S2215-0366(15)00271-0
Ghirardi L, Chen Q, Chang Z, Kuja-Halkola R, Skoglund C, Quinn PD, Larsson H (2019) Use of medication for attention-deficit/hyperactivity disorder and risk of unintentional injuries in children and adolescents with co-occurring neurodevelopmental disorders. J Child Psychol Psychiatry 61:140–147. https://doi.org/10.1111/jcpp.13136
Laugesen B, Lauritsen MB, Jørgensen R, Sørensen EE, Rasmussen P, Grønkjær M (2016) Living with a child with attention deficit hyperactivity disorder: a systematic review. Int J Evid Based Healthc 14:150–165
Moen ØL, Hedelin B, Hall-Lord ML (2015) Parental perception of family functioning in everyday life with a child with ADHD. Scand J Public Health 43:10–17. https://doi.org/10.1177/1403494814559803
Moen ØL, Hedelin B, Hall-Lord ML (2016) Family functioning, psychological distress, and well-being in parents with a child having ADHD. SAGE Open. https://doi.org/10.1177/2158244015626767
Lemcke S, Parner ET, Bjerrum M, Thomsen PH, Lauritsen MB (2016) Early development in children that are later diagnosed with disorders of attention and activity: a longitudinal study in the Danish National Birth Cohort. Eur Child Adolesc Psychiatry 10:1055–1066. https://doi.org/10.1007/s00787-016-0825-6
Laugesen B, Lauritsen MB, Jørgensen R, Sørensen EE, Grønkjær M, Rasmussen P (2017) ADHD and everyday life: healthcare as a significant lifeline. J Pediatr Nurs 35:105–112. https://doi.org/10.1016/j.pedn.2017.03.001
Du RE, Jangmo A, Kuja-halkola R et al (2020) Trajectories of healthcare utilization and costs of psychiatric and somatic multimorbidity in adults with childhood ADHD : a prospective register-based study. J Child Psychol Psychiatry 61:959–968. https://doi.org/10.1111/jcpp.13206
Leffa DT, Torres ILS, Rohde LA (2019) A review on the role of inflammation in attention-deficit/hyperactivity disorder. Neuroimmunomodulation 25:328–333. https://doi.org/10.1159/000489635
Tong L, Shi H, Li X (2017) Associations among ADHD, abnormal eating and overweight in a non-clinical sample of Asian children. Sci Rep 7:2–9. https://doi.org/10.1038/s41598-017-03074-4
Tong L, Ye Y, Yan Q (2018) The moderating roles of bedtime activities and anxiety/depression in the relationship between attention-deficit/hyperactivity disorder symptoms and sleep problems in children. BMC Psychiatry 18:1–12. https://doi.org/10.1186/s12888-018-1879-4
Kavanagh J, Jackson DJ, Kent BD (2018) Sleep and asthma. Curr Opin Pulm Med 24:569–573. https://doi.org/10.1097/MCP.0000000000000526
Mann C, Dreher M, Weeß H, Staubach P (2020) Sleep disturbance in patients with urticaria and atopic dermatitis: an underestimated burden. Acta Derm Venereol 12:100. https://doi.org/10.2340/00015555-3416
Cortese S, Moreira-Maia CR, St. Fleur D, Morcillo-Peñalver C, Rohde LA, Faraone S V. (2009) Association between ADHD and obesity: a systematic review and meta-analysis. Am J Psychiatry 173:34–43. https://doi.org/10.1176/appi.ajp.2015.15020266
Levy LD, Fleming JP, Klar D (2009) Treatment of refractory obesity in severely obese adults following management of newly diagnosed attention deficit hyperactivity disorder. Int J Obes 33:326–334. https://doi.org/10.1038/ijo.2009.5
Cortese S, Tessari L (2017) Attention-deficit/hyperactivity disorder (ADHD) and obesity: update 2016. Curr Psychiatry Rep 19:4. https://doi.org/10.1007/s11920-017-0754-1
Mohr-Jensen C, Vinkel Koch S, Briciet Lauritsen M, Steinhausen HC (2016) The validity and reliability of the diagnosis of hyperkinetic disorders in the Danish Psychiatric Central Research Registry. Eur Psychiatry 35:16–24. https://doi.org/10.1016/j.eurpsy.2016.01.2427
Funding
No funding was received for this manuscript. The authors have no financial relationships relevant to this article to disclose.
Author information
Authors and Affiliations
Contributions
BL conceptualized and designed the study, applied for the data from the nationwide health registries, interpreted and discussed the results of the statistical analysis, drafted the initial manuscript, and reviewed and revised the manuscript. MBL conceptualized and designed the study, coordinated and supervised the collection of data from the nationwide health registries, interpreted and discussed the results of the statistical analysis and critically reviewed the manuscript. EF conceptualized and designed the study, performed the data management and statistical analysis, interpreted and discussed the results of the statistical analysis and critically reviewed the manuscript. CMJ conceptualized and designed the study, coordinated and supervised the collection of data from the nationwide health registries, interpreted and discussed the results of the statistical analysis, aided in drafting the initial manuscript, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Mohr Jensen has received speaker fees from Medice Nordic and Icepharma. The other authors declare no conflicts of interests.
Rights and permissions
About this article
Cite this article
Laugesen, B., Lauritsen, M.B., Færk, E. et al. Medical disorders in a Danish cohort of children with attention-deficit hyperactivity disorder. Eur Child Adolesc Psychiatry 31, 349–359 (2022). https://doi.org/10.1007/s00787-020-01693-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-020-01693-3