Abstract
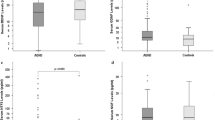
This study aimed to investigate serum levels of neurotrophins, including brain-derived neurotrophic factor (BDNF), glial-derived neurotrophic factor (GDNF), nerve growth factor (NGF) and neurotrophin-3 (NTF3), and hypothalamic–pituitary–adrenal axis (HPA) members including adrenocorticotropic hormone (ACTH) and cortisol in children with obsessive–compulsive disorder (OCD). The possible relationships between serum neurotrophins and HPA axis members were also addressed. A total of 60 medication-free children with OCD and 57 controls aged 8–18 years were enrolled in this study. The severity of OCD symptoms was determined by the Children’s Yale-Brown Obsessive Compulsive Scale. The severity of anxiety and depression symptoms were assessed by self-report inventories. The serum levels of neurotrophins, ACTH, and cortisol were measured using enzyme-linked immunosorbent assay kits. Serum BDNF levels were significantly higher in the OCD group than in the control group for either sex and for the whole sample. Compared to controls, serum ACTH levels were significantly higher in the OCD group for the whole sample. An analysis of covariance was also conducted for the whole sample and indicated that, while controlling the potential confounders, including body-mass index percentile, age, sex, and the severity of depression and anxiety, the results did not change. Strong negative correlations between BDNF, NGF and NTF3, and HPA axis members were determined in the patient group for either sex and for the whole sample. These findings suggest that dysregulations of BDNF and ACTH may be associated with childhood OCD. Furthermore, there may be inverse relationships between certain neurotrophins and HPA axis members in these patients.


Similar content being viewed by others
References
Thomsen PH (2013) Obsessive-compulsive disorders. Eur Child Adolesc Psychiatry 22(Suppl 1):S23-28
Wang S, Xu X, Yan P, Song M, Li J, Wang S (2019) Is brain-derived neurotrophic factor (BDNF) Val66Met polymorphism associated with obsessive-compulsive disorder? A meta-analysis. Psychiatr Danub 31:141–147
D’Addario C, Bellia F, Benatti B, Grancini B, Vismara M, Pucci M, De Carlo V, Vigano C, Galimberti D, Fenoglio C, Scarpini E, Maccarrone M, Dell’Osso B (2019) Exploring the role of BDNF DNA methylation and hydroxymethylation in patients with obsessive compulsive disorder. J Psychiatr Res 114:17–23
Fontenelle LF, Barbosa IG, Luna JV, Rocha NP, Silva Miranda A, Teixeira AL (2012) Neurotrophic factors in obsessive-compulsive disorder. Psychiatry Res 199:195–200
Maina G, Rosso G, Zanardini R, Bogetto F, Gennarelli M, Bocchio-Chiavetto L (2010) Serum levels of brain-derived neurotrophic factor in drug-naive obsessive-compulsive patients: a case-control study. J Affect Disord 122:174–178
Simsek S, Gencoglan S, Yuksel T, Kaplan I, Alaca R (2016) Cortisol and brain-derived neurotrophic factor levels prior to treatment in children with obsessive-compulsive disorder. J Clin Psychiatry 77:e855-859
Gustafsson PE, Gustafsson PA, Ivarsson T, Nelson N (2008) Diurnal cortisol levels and cortisol response in youths with obsessive-compulsive disorder. Neuropsychobiology 57:14–21
Melia CS, Soria V, Salvat-Pujol N, Cabezas A, Nadal R, Urretavizcaya M, Gutierrez-Zotes A, Monreal JA, Crespo JM, Alonso P, Vilella E, Palao D, Menchon JM, Labad J (2019) Sex-specific association between the cortisol awakening response and obsessive-compulsive symptoms in healthy individuals. Biol Sex Differ 10:55
Kluge M, Schussler P, Kunzel HE, Dresler M, Yassouridis A, Steiger A (2007) Increased nocturnal secretion of ACTH and cortisol in obsessive compulsive disorder. J Psychiatr Res 41:928–933
Lang UE, Jockers-Scherubl MC, Hellweg R (2004) State of the art of the neurotrophin hypothesis in psychiatric disorders: implications and limitations. J Neural Transm (Vienna) 111:387–411
Abdolhosseinzadeh S, Alizadeh N, Shams J, Asadi S, Ahmadiani A (2020) BDNF association study with obsessive-compulsive disorder, its clinical characteristics, and response to fluvoxamine-treatment in Iranian patients. Exp Clin Psychopharmacol 28:216–224
Taj MJR, Ganesh S, Shukla T, Deolankar S, Nadella RK, Sen S, Purushottam M, Reddy YCJ, Jain S, Viswanath B (2018) BDNF gene and obsessive compulsive disorder risk, symptom dimensions and treatment response. Asian J Psychiatr 38:65–69
Wang J, Zhang F, Zhu W, Liu Y, Zhou Z (2015) Meta-analysis of the association of brain-derived neurotrophic factor Val66Met polymorphism with obsessive-compulsive disorder. Acta Neuropsychiatr 27:327–335
Wang Y, Zhang H, Li Y, Wang Z, Fan Q, Yu S, Lin Z, Xiao Z (2015) BDNF Val66Met polymorphism and plasma levels in Chinese Han population with obsessive-compulsive disorder and generalized anxiety disorder. J Affect Disord 186:7–12
Colak Sivri R, Bilgic A, Kilinc I (2018) Cytokine, chemokine and BDNF levels in medication-free pediatric patients with obsessive-compulsive disorder. Eur Child Adolesc Psychiatry 27:977–984
Pedrotti Moreira F, Wiener CD, Jansen K, Portela LV, Lara DR, Souza LDM, da Silva RA, Oses JP (2018) Serum GDNF levels and anxiety disorders in a population-based study of young adults. Clin Chim Acta 485:21–25
Gasso P, Ortiz AE, Mas S, Morer A, Calvo A, Bargallo N, Lafuente A, Lazaro L (2015) Association between genetic variants related to glutamatergic, dopaminergic and neurodevelopment pathways and white matter microstructure in child and adolescent patients with obsessive-compulsive disorder. J Affect Disord 186:284–292
Muinos-Gimeno M, Guidi M, Kagerbauer B, Martin-Santos R, Navines R, Alonso P, Menchon JM, Gratacos M, Estivill X, Espinosa-Parrilla Y (2009) Allele variants in functional MicroRNA target sites of the neurotrophin-3 receptor gene (NTRK3) as susceptibility factors for anxiety disorders. Hum Mutat 30:1062–1071
Alonso P, Gratacos M, Menchon JM, Segalas C, Gonzalez JR, Labad J, Bayes M, Real E, de Cid R, Pertusa A, Escaramis G, Vallejo J, Estivill X (2008) Genetic susceptibility to obsessive-compulsive hoarding: the contribution of neurotrophic tyrosine kinase receptor type 3 gene. Genes Brain Behav 7:778–785
Real E, Labad J, Alonso P, Segalas C, Jimenez-Murcia S, Bueno B, Subira M, Vallejo J, Menchon JM (2011) Stressful life events at onset of obsessive-compulsive disorder are associated with a distinct clinical pattern. Depress Anxiety 28:367–376
Morgado P, Freitas D, Bessa JM, Sousa N, Cerqueira JJ (2013) Perceived stress in obsessive-compulsive disorder is related with obsessive but not compulsive symptoms. Front Psychiatry 4:21
Bigos KL, Folan MM, Jones MR, Haas GL, Kroboth FJ, Kroboth PD (2009) Dysregulation of neurosteroids in obsessive compulsive disorder. J Psychiatr Res 43:442–445
Kawano A, Tanaka Y, Ishitobi Y, Maruyama Y, Ando T, Inoue A, Okamoto S, Imanaga J, Kanehisa M, Higuma H, Ninomiya T, Tsuru J, Akiyoshi J (2013) Salivary alpha-amylase and cortisol responsiveness following electrical stimulation stress in obsessive-compulsive disorder patients. Psychiatry Res 209:85–90
Sousa-Lima J, Moreira PS, Raposo-Lima C, Sousa N, Morgado P (2019) Relationship between obsessive compulsive disorder and cortisol: Systematic review and meta-analysis. Eur Neuropsychopharmacol 29:1185–1198
Labad J, Soria V, Salvat-Pujol N, Segalas C, Real E, Urretavizcaya M, de Arriba-Arnau A, Ferrer A, Crespo JM, Jimenez-Murcia S, Soriano-Mas C, Alonso P, Menchon JM (2018) Hypothalamic-pituitary-adrenal axis activity in the comorbidity between obsessive-compulsive disorder and major depression. Psychoneuroendocrinology 93:20–28
Unal F, Oktem F, Cetin Cuhadaroglu F, Cengel Kultur SE, Akdemir D, Foto Ozdemir D, Cak HT, Unal D, Tiras K, Aslan C, Kalayci BM, Aydos BS, Kutuk F, Tasyurek E, Karaokur R, Karabucak B, Karakok B, Karaer Y, Artik A (2019) Reliability and Validity of the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version, DSM-5 November 2016-Turkish Adaptation (K-SADS-PL-DSM-5-T). Turk Psikiyatri Derg 30:42–50
Yucelen AG, Rodopman-Arman A, Topcuoglu V, Yazgan MY, Fisek G (2006) Interrater reliability and clinical efficacy of Children’s Yale-Brown Obsessive-Compulsive Scale in an outpatient setting. Compr Psychiatry 47:48–53
Oy B (1991) Children’s Depression Inventory: a study of reliability and validity. Turk Psychiatry Derg 2:137–140
Karaceylan F (2005) Reliability and validity of SCARED in Turkish children. Kocaeli University, Kocaeli
Al-Safi ZA, Polotsky A, Chosich J, Roth L, Allshouse AA, Bradford AP, Santoro N (2018) Evidence for disruption of normal circadian cortisol rhythm in women with obesity. Gynecol Endocrinol 34:336–340
Zamani M, Hosseini SV, Behrouj H, Erfani M, Dastghaib S, Ahmadi M, Shamsdin SA, Mokarram P (2019) BDNF Val66Met genetic variation and its plasma level in patients with morbid obesity: a case-control study. Gene 705:51–54
Wang Y, Mathews CA, Li Y, Lin Z, Xiao Z (2011) Brain-derived neurotrophic factor (BDNF) plasma levels in drug-naive OCD patients are lower than those in healthy people, but are not lower than those in drug-treated OCD patients. J Affect Disord 133:305–310
Pauls DL, Abramovitch A, Rauch SL, Geller DA (2014) Obsessive-compulsive disorder: an integrative genetic and neurobiological perspective. Nat Rev Neurosci 15(6):410–424
Boedhoe PS, Schmaal L, Abe Y, Ameis SH, Arnold PD, Batistuzzo MC, Benedetti F, Beucke JC, Bollettini I, Bose A, Brem S, Calvo A, Cheng Y, Cho KI, Dallaspezia S, Denys D, Fitzgerald KD, Fouche JP, Giménez M, Gruner P, Hanna GL, Hibar DP, Hoexter MQ, Hu H, Huyser C, Ikari K, Jahanshad N, Kathmann N, Kaufmann C, Koch K, Kwon JS, Lazaro L, Liu Y, Lochner C, Marsh R, Martínez-Zalacaín I, Mataix-Cols D, Menchón JM, Minuzzi L, Nakamae T, Nakao T, Narayanaswamy JC, Piras F, Piras F, Pittenger C, Reddy YC, Sato JR, Simpson HB, Soreni N, Soriano-Mas C, Spalletta G, Stevens MC, Szeszko PR, Tolin DF, Venkatasubramanian G, Walitza S, Wang Z, van Wingen GA, Xu J, Xu X, Yun JY, Zhao Q; ENIGMA OCD Working Group, Thompson PM, Stein DJ, van den Heuvel OA (2017) Distinct subcortical volume alterations in pediatric and adult OCD: a worldwide meta- and mega-analysis. Am J Psychiatry 174:60–69
Kong XZ, Boedhoe PSW, Abe Y, Alonso P, Ameis SH, Arnold PD, Assogna F, Baker JT, Batistuzzo MC, Benedetti F, Beucke JC, Bollettini I, Bose A, Brem S, Brennan BP, Buitelaar J, Calvo R, Cheng Y, Cho KIK, Dallaspezia S, Denys D, Ely BA, Feusner J, Fitzgerald KD, Fouche JP, Fridgeirsson EA, Glahn DC, Gruner P, Gürsel DA, Hauser TU, Hirano Y, Hoexter MQ, Hu H, Huyser C, James A, Jaspers-Fayer F, Kathmann N, Kaufmann C, Koch K, Kuno M, Kvale G, Kwon JS, Lazaro L, Liu Y, Lochner C, Marques P, Marsh R, Martínez-Zalacaín I, Mataix-Cols D, Medland SE, Menchón JM, Minuzzi L, Moreira PS, Morer A, Morgado P, Nakagawa A, Nakamae T, Nakao T, Narayanaswamy JC, Nurmi EL, O’Neill J, Pariente JC, Perriello C, Piacentini J, Piras F, Piras F, Pittenger C, Reddy YCJ, Rus-Oswald OG, Sakai Y, Sato JR, Schmaal L, Simpson HB, Soreni N, Soriano-Mas C, Spalletta G, Stern ER, Stevens MC, Stewart SE, Szeszko PR, Tolin DF, Tsuchiyagaito A, van Rooij D, van Wingen GA, Venkatasubramanian G, Wang Z, Yun JY; ENIGMA OCD Working Group, Thompson PM, Stein DJ, van den Heuvel OA, Francks C (2020) Mapping cortical and subcortical asymmetry in obsessive-compulsive disorder: findings from the ENIGMA consortium. Biol Psychiatry 87:1022–1034
Boedhoe PSW, Schmaal L, Abe Y, Alonso P, Ameis SH, Anticevic A, Arnold PD, Batistuzzo MC, Benedetti F, Beucke JC, Bollettini I, Bose A, Brem S, Calvo A, Calvo R, Cheng Y, Cho KIK, Ciullo V, Dallaspezia S, Denys D, Feusner JD, Fitzgerald KD, Fouche JP, Fridgeirsson EA, Gruner P, Hanna GL, Hibar DP, Hoexter MQ, Hu H, Huyser C, Jahanshad N, James A, Kathmann N, Kaufmann C, Koch K, Kwon JS, Lazaro L, Lochner C, Marsh R, Martínez-Zalacaín I, Mataix-Cols D, Menchón JM, Minuzzi L, Morer A, Nakamae T, Nakao T, Narayanaswamy JC, Nishida S, Nurmi E, O’Neill J, Piacentini J, Piras F, Piras F, Reddy YCJ, Reess TJ, Sakai Y, Sato JR, Simpson HB, Soreni N, Soriano-Mas C, Spalletta G, Stevens MC, Szeszko PR, Tolin DF, van Wingen GA, Venkatasubramanian G, Walitza S, Wang Z, Yun JY; ENIGMA-OCD Working Group, Thompson PM, Stein DJ, van den Heuvel OA; ENIGMA OCD Working Group (2018) Cortical abnormalities associated with pediatric and adult obsessive-compulsive disorder: findings from the ENIGMA obsessive-compulsive disorder working Group. Am J Psychiatry 175:453–462
Williams K, Shorser-Gentile L, Sarvode Mothi S, Berman N, Pasternack M, Geller D, Walter J (2019) Immunoglobulin A dysgammaglobulinemia is associated with pediatric-onset obsessive-compulsive disorder. J Child Adolesc Psychopharmacol 29:268–275
Ambrus L, Lindqvist D, Traskman-Bendz L, Westrin A (2016) Hypothalamic-pituitary-adrenal axis hyperactivity is associated with decreased brain-derived neurotrophic factor in female suicide attempters. Nord J Psychiatry 70:575–581
Hill TD, Uchino BN, Eckhardt JL, Angel JL (2016) Perceived social support trajectories and the all-cause mortality risk of older Mexican American women and men. Res Aging 38:374–398
Hennings JM, Kohli MA, Uhr M, Holsboer F, Ising M, Lucae S (2019) Polymorphisms in the BDNF and BDNFOS genes are associated with hypothalamus-pituitary axis regulation in major depression. Prog Neuropsychopharmacol Biol Psychiatry 95:109686
Schule C, Zill P, Baghai TC, Eser D, Zwanzger P, Wenig N, Rupprecht R, Bondy B (2006) Brain-derived neurotrophic factor Val66Met polymorphism and dexamethasone/CRH test results in depressed patients. Psychoneuroendocrinology 31:1019–1025
Givalois L, Naert G, Rage F, Ixart G, Arancibia S, Tapia-Arancibia L (2004) A single brain-derived neurotrophic factor injection modifies hypothalamo-pituitary-adrenocortical axis activity in adult male rats. Mol Cell Neurosci 27:280–295
Bakos J, Hlavacova N, Rajman M, Ondicova K, Koros C, Kitraki E, Steinbusch HW, Jezova D (2009) Enriched environment influences hormonal status and hippocampal brain derived neurotrophic factor in a sex dependent manner. Neuroscience 164:788–797
Naert G, Zussy C, Tran Van Ba C, Chevallier N, Tang YP, Maurice T, Givalois L (2015) Involvement of endogenous brain-derived neurotrophic factor in hypothalamic-pituitary-adrenal axis activity. J Neuroendocrinol 27:850–860
Acknowledgments
The authors wish to thank the patients and their family members who participated in this study.
Funding
Funding for this study was provided by a grant from the Scientific Research Project Coordination Unit of Necmettin Erbakan University (Project Number: 191218008).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no potential conflicts of interest.
Rights and permissions
About this article
Cite this article
Bilgiç, A., Sertdemir, M., Kılınç, İ. et al. Increased serum brain-derived neurotrophic factor and adrenocorticotropic hormone levels are associated with obsessive compulsive disorder in medication‑free children. Eur Child Adolesc Psychiatry 31, 325–335 (2022). https://doi.org/10.1007/s00787-020-01690-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-020-01690-6