Abstract
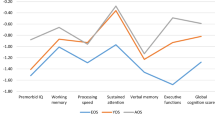
Neuropsychological underperformance is well described in young adults at clinical high risk for psychosis, but the literature is scarce on the cognitive profile of at-risk children and adolescents. The aim of this study is to describe the neuropsychological profile of a child and adolescent sample of patients with psychosis risk syndrome (PRS) compared to healthy controls and to analyze associations between attenuated psychotic symptoms and cognitive impairment. Cross-sectional baseline data analysis from a longitudinal, naturalistic, case–control, two-site study is presented. Eighty-one help-seeking subjects with PRS and 39 healthy controls (HC) aged between 10 and 17 years of age were recruited. PRS was defined by: positive or negative attenuated symptoms, Brief Limited Intermittent Psychotic Symptoms (BLIPS), genetic risk (first- or second-degree relative), or schizotypal personality disorder plus impairment in functioning. A neuropsychological battery was administered to assess general intelligence, verbal and visual memory, visuospatial abilities, speed processing, attention, and executive functions. The PRS group showed lower general neuropsychological performance scores at a multivariate level and lower scores than controls in general intelligence and executive functions. Lower scores on executive function and poorer attention were associated with high scores of positive attenuated psychotic symptoms. No association with attenuated negative symptoms was found. This study provides evidence of cognitive impairment in PRS children and adolescents and shows a relationship between greater cognitive impairment in executive functions and attention tasks and severe attenuated positive symptoms. However, longitudinal studies are needed to clarify the nature of cognitive impairment as a possible vulnerability marker.
Similar content being viewed by others
References
Yung AR, McGorry PD (1996) The initial prodrome in psychosis: descriptive and qualitative aspects. Aust N Z J Psychiatry 30:587–599. https://doi.org/10.3109/00048679609062654
McGorry P (1995) A treatment-relevant classification of psychotic disorders. Aust New Zeal J Psychiatry 29:555–558. https://doi.org/10.3109/00048679509064966
Miller TJ, McGlashan TH, Rosen JL et al (2003) Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull 29:703–715
Schultze-Lutter F, Michel C, Schmidt SJ et al (2015) EPA guidance on the early detection of clinical high risk states of psychoses. Eur Psychiatry 30:405–416. https://doi.org/10.1016/j.eurpsy.2015.01.010
Kirkbride JB, Fearon P, Morgan C et al (2006) Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes: Findings from the 3-center ÆSOP study. Arch Gen Psychiatry 63:250–258. https://doi.org/10.1001/archpsyc.63.3.250
Schimmelmann B, Walger P, Schultze-Lutter F (2013) The significance of at-risk symptoms for psychosis in children and adolescents. Can J Psychiatry 58:32–40. https://doi.org/10.1093/cid/cit520.3
McGorry PD, Edwards J, Mihalopoulos C et al (1996) EPPIC: an evolving system of early detection and optimal management. Schizophr Bull 22:305–326
Green MF, Kern RS, Braff DL, Mintz J (2000) Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull 26:119–136. https://doi.org/10.1093/oxfordjournals.schbul.a033430
Arango C (2011) Attenuated psychotic symptoms syndrome: how it may affect child and adolescent psychiatry. Eur Child Adolesc Psychiatry 20:67–70. https://doi.org/10.1007/s00787-010-0144-2
Ballageer T, Malla A, Manchanda R et al (2005) Is adolescent-onset first-episode psychosis different from adult onset? J Am Acad Child Adolesc Psychiatry 44:782–789. https://doi.org/10.1097/01.chi.0000164591.55942.ea
Joa I, Johannessen JO, Langeveld J et al (2009) Baseline profiles of adolescent vs. adult-onset first-episode psychosis in an early detection program. Acta Psychiatr Scand 119:494–500. https://doi.org/10.1111/j.1600-0447.2008.01338.x
Dominguez M-G, Fisher HL, Major B et al (2013) Duration of untreated psychosis in adolescents: ethnic differences and clinical profiles. Schizophr Res 150:526–532. https://doi.org/10.1016/j.schres.2013.08.018
Rajji TK, Ismail Z, Mulsant BH (2009) Age at onset and cognition in schizophrenia: meta-analysis. Br J Psychiatry 195:286–293. https://doi.org/10.1192/bjp.bp.108.060723
Nieto RG, Castellanos FX (2011) A meta-analysis of neuropsychological functioning in patients with early onset schizophrenia and pediatric bipolar disorder. J Clin Child Adolesc Psychol 40:266–280. https://doi.org/10.1080/15374416.2011.546049
Tor J, Dolz M, Sintes A et al (2017) Clinical high risk for psychosis in children and adolescents: a systematic review. Eur Child Adolesc Psychiatry. https://doi.org/10.1007/s00787-017-1046-3
Schultze-Lutter F, Renner F, Paruch J et al (2014) Self-reported psychotic-like experiences are a poor estimate of clinician-rated attenuated and frank delusions and hallucinations. Psychopathology 47:194–201. https://doi.org/10.1159/000355554
Kelleher I, Connor D, Clarke MC et al (2013) Prevalence of psychotic symptoms in childhood and adolescence: a systematic review and meta-analysis of population-based studies. Psychol Med. https://doi.org/10.1017/S0033291711002960
Calkins ME, Moore TM, Merikangas KR et al (2014) The psychosis spectrum in a young US community sample: findings from the Philadelphia Neurodevelopmental Cohort. World Psychiatry 13:296–305
Sugranyes G, de la Serna E, Borras R et al (2017) Clinical, cognitive, and neuroimaging evidence of a neurodevelopmental continuum in offspring of probands with schizophrenia and bipolar disorder. Schizophr Bull 43:1208–1219. https://doi.org/10.1093/schbul/sbx002
Seidman LJ, Giuliano AJ, Meyer EC et al (2010) Neuropsychology of the prodrome to psychosis in the NAPLS consortium: relationship to family history and conversion to psychosis. Arch Gen Psychiatry 67:578. https://doi.org/10.1001/archgenpsychiatry.2010.66
Giuliano AJ, Li H, Mesholam-Gately RI et al (2012) Neurocognition in the psychosis risk syndrome: a quantitative and qualitative review. Curr Pharm Des 18:399–415. https://doi.org/10.2174/138161212799316019
de la Serna E, Sugranyes G, Sanchez-Gistau V et al (2017) Neuropsychological characteristics of child and adolescent offspring of patients with schizophrenia or bipolar disorder. Schizophr Res 183:110–115. https://doi.org/10.1016/j.schres.2016.11.007
Zabala A, Rapado M, Arango C et al (2010) Neuropsychological functioning in early-onset first-episode psychosis: comparison of diagnostic subgroups. Eur Arch Psychiatry Clin Neurosci 260:225–233. https://doi.org/10.1007/s00406-009-0046-9
de la Serna E, Andrés-Perpiñá S, Puig O et al (2013) Cognitive reserve as a predictor of 2 years neuropsychological performance in early onset first-episode schizophrenia. Schizophr Res 143:125–131. https://doi.org/10.1016/j.schres.2012.10.026
Moritz S, Klein JP, Desler T et al (2017) Neurocognitive deficits in schizophrenia. Are we making mountains out of molehills? Psychol Med 47:2602–2612. https://doi.org/10.1017/S0033291717000939
Schaefer J, Giangrande E, Weinberger DR, Dickinson D (2013) The global cognitive impairment in schizophrenia: consistent over decades and around the world. Schizophr Res 150:42–50. https://doi.org/10.1016/j.schres.2013.07.009
Fusar-Poli P, Deste G, Smieskova R et al (2012) Cognitive functioning in prodromal psychosis: a meta-analysis. Arch Gen Psychiatry 69:562–571. https://doi.org/10.1001/archgenpsychiatry.2011.1592
Frommann I, Pukrop R, Brinkmeyer J et al (2011) Neuropsychological profiles in different at-risk states of psychosis: executive control impairment in the early- and additional memory dysfunction in the late-prodromal state. Schizophr Bull 37:861–873. https://doi.org/10.1093/schbul/sbp155
Pukrop R, Schultze-Lutter F, Ruhrmann S et al (2006) Neurocognitive functioning in subjects at risk for a first episode of psychosis compared with first- and multiple-episode schizophrenia. J Clin Exp Neuropsychol 28:1388–1407. https://doi.org/10.1080/13803390500434425
Ziermans T, de Wit S, Schothorst P et al (2014) Neurocognitive and clinical predictors of long-term outcome in adolescents at ultra-high risk for psychosis: a 6-year follow-up. PLoS ONE 9:e93994. https://doi.org/10.1371/journal.pone.0093994
Riecher-Rössler A, Pflueger MO, Aston J et al (2009) Efficacy of using cognitive status in predicting psychosis: a 7-year follow-up. Biol Psychiatry 66:1023–1030. https://doi.org/10.1016/j.biopsych.2009.07.020
Gur RC, Calkins ME, Satterthwaite TD et al (2014) Neurocognitive growth charting in psychosis spectrum youths. JAMA Psychiatry 71:366–374. https://doi.org/10.1001/jamapsychiatry.2013.4190
Woodberry KA, McFarlane WR, Giuliano AJ et al (2013) Change in neuropsychological functioning over 1 year in youth at clinical high risk for psychosis. Schizophr Res 146:87–94. https://doi.org/10.1016/j.schres.2013.01.017
Woodberry KA, Seidman LJ, Giuliano AJ et al (2010) Neuropsychological profiles in individuals at clinical high risk for psychosis: relationship to psychosis and intelligence. Schizophr Res 123:188–198. https://doi.org/10.1016/j.schres.2010.06.021
Seidman LJ, Shapiro DI, Stone WS et al (2016) Association of neurocognition with transition to psychosis: baseline functioning in the second phase of the North American Prodrome Longitudinal Study. JAMA Psychiatry 73:1239. https://doi.org/10.1001/jamapsychiatry.2016.2479
Dolz M, Tor J, De la Serna E et al (2018) Characterization of children and adolescents with psychosis risk syndrome: the Children and Adolescents Psychosis Risk Syndrome (CAPRIS) study. Early Interv Psychiatry. https://doi.org/10.1111/eip.12728
Ribolsi M, Lin A, Wardenaar KJ et al (2017) Clinical presentation of Attenuated Psychosis Syndrome in children and adolescents: is there an age effect? Psychiatry Res 252:169–174. https://doi.org/10.1016/j.psychres.2017.02.050
Lo CN, Saba R, Hauser M et al (2016) Attenuated psychotic and basic symptom characteristics in adolescents with ultra-high risk criteria for psychosis, other non-psychotic psychiatric disorders and early-onset psychosis. Eur Child Adolesc Psychiatry. https://doi.org/10.1007/s00787-016-0832-7
Welsh P, Tiffin PA (2014) The “at-risk mental state” for psychosis in adolescents: clinical presentation, transition and remission. Child Psychiatry Hum Dev 45:90–98. https://doi.org/10.1007/s10578-013-0380-z
Fusar-Poli P, Nelson B, Valmaggia L et al (2014) Comorbid depressive and anxiety disorders in 509 individuals with an at-risk mental state: impact on psychopathology and transition to psychosis. Schizophr Bull 40:120–131. https://doi.org/10.1093/schbul/sbs136
Hui C, Morcillo C, Russo DA et al (2013) Psychiatric morbidity, functioning and quality of life in young people at clinical high risk for psychosis. Schizophr Res 148:175–180. https://doi.org/10.1016/j.schres.2013.05.026
Lindgren M, Manninen M, Laajasalo T et al (2010) The relationship between psychotic-like symptoms and neurocognitive performance in a general adolescent psychiatric sample. Schizophr Res 123:77–85. https://doi.org/10.1016/j.schres.2010.07.025
Ziermans TB (2013) Working memory capacity and psychotic-like experiences in a general population sample of adolescents and young adults. Front Psychiatry. https://doi.org/10.3389/fpsyt.2013.00161
Niendam TA, Bearden CE, Johnson JK et al (2006) Neurocognitive performance and functional disability in the psychosis prodrome. Schizophr Res 84:100–111. https://doi.org/10.1016/j.schres.2006.02.005
Ohmuro N, Matsumoto K, Katsura M et al (2015) The association between cognitive deficits and depressive symptoms in at-risk mental state: a comparison with first-episode psychosis. Schizophr Res 162:67–73. https://doi.org/10.1016/j.schres.2015.01.008
Kim SJ, Lee YJ, Jang JH et al (2012) The relationship between psychotic-like experiences and attention deficits in adolescents. J Psychiatr Res 46:1354–1358. https://doi.org/10.1016/j.jpsychires.2012.07.002
Mathers C, Fat DM, Boerma T, World Health Organization (2004) The global burden of disease: 2004 update. World Health Organization, Geneva
Lencz T, Smith CW, Auther A et al (2004) Nonspecific and attenuated negative symptoms in patients at clinical high-risk for schizophrenia. Schizophr Res 68:37–48. https://doi.org/10.1016/S0920-9964(03)00214-7
Klosterkötter J, Birchwood M, Linszen D et al (2005) Overview on the recruitment, sample characteristics, and distribution of inclusion criteria of the European Prediction of Psychosis Study (EPOS). Eur Psychiatry Suppl 20:48
Miller TJ, McGlashan TH, Rosen JL et al (2002) Prospective diagnosis of the initial prodrome for schizophrenia based on the structured interview for prodromal syndromes: preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry 159:863–865. https://doi.org/10.1176/appi.ajp.159.5.863
Hollingshead AB, Redlich FC (2007) Social class and mental illness: a community study. 1958. Am J Public Health 97:1756–1757
Kaufman J, Birmaher B, Brent D et al (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988. https://doi.org/10.1097/00004583-199707000-00021
Rutter M, Bailey A, Lord C (2003) The social communication questionnaire: manual. Western Psychological Services, Los Angeles
Lord C, Risi S, Lambrecht L et al (2000) The autism diagnostic observation schedule—generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord 30:205–223. https://doi.org/10.1023/A:1005592401947
Hamilton M (1967) Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 6:278–296
Endicott J, Spitzer RL, Fleiss JL, Cohen J (1976) The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 33:766–771
Nuechterlein KH, Green MF, Kern RS et al (2008) The MATRICS consensus cognitive battery, part 1: test selection, reliability, and validity. Am J Psychiatry 165:203–213. https://doi.org/10.1176/appi.ajp.2007.07010042
Wechsler D (2003) Wechsler intelligence scale for children-IV (WISC-IV). TEA Edicio, Madrid
Wechsler D (2001) Escala de inteligencia de Wechsler para adultos (WAIS-III). TEA Edicio, Madrid
Niemi LT, Suvisaari JM, Tuulio-Henriksson A, Lönnqvist JK (2003) Childhood developmental abnormalities in schizophrenia: evidence from high-risk studies. Schizophr Res 60:239–258. https://doi.org/10.1016/S0920-9964(02)00234-7
Puig O, Penadés R, Baeza I et al (2012) Processing speed and executive functions predict real-world everyday living skills in adolescents with early-onset schizophrenia. Eur Child Adolesc Psychiatry 21:315–326. https://doi.org/10.1007/s00787-012-0262-0
Puig O, Penadés R, Baeza I et al (2014) Cognitive remediation therapy in adolescents with early-onset schizophrenia: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 53:859–868. https://doi.org/10.1016/j.jaac.2014.05.012
Reynolds CR, Bigler ED (2001) TOMAL: test de memoria y aprendizaje. TEA Edicio, Madrid
Wechsler D (1997) The Wechsler memory scale (WMS-III), 3rd edn. TEA Edicio, Madrid
Rey A (1964) L’examen clinique en psychologie. Presses Un, Paris
Reitan R (1985) The Halstead–Reitan neuropsychological test battery: theory and clinical interpretation. Reitan Neu, Tucson
Conners K (2000) Conners’ continuous performance test, CPT-II. MHS, Toronto
Heaton R, Chelune GJ, Talley JL et al (1997) Wisconsin card sorting test (WCST). TEA Edicio, Madrid
Loonstra AS, Tarlow AR, Sellers AH (2001) COWAT metanorms across age, education, and gender. Appl Neuropsychol Adult 8:161–166. https://doi.org/10.1207/S15324826AN0803
Savage CR, Baer L, Keuthen NJ et al (1999) Organizational strategies mediate nonverbal memory impairment in obsessive–compulsive disorder. Biol Psychiatry 45:905–916
Fusar-Poli P, Deste G, Smieskova R et al (2012) Cognitive functioning in prodromal psychosis. Arch Gen Psychiatry 69:562–571
de Paula ALD, Hallak JEC, Maia-de-Oliveira JP et al (2015) Cognition in at-risk mental states for psychosis. Neurosci Biobehav Rev 57:199–208. https://doi.org/10.1016/j.neubiorev.2015.09.006
van Rijn S, Schothorst P, van’t Wout M et al (2011) Affective dysfunctions in adolescents at risk for psychosis: emotion awareness and social functioning. Psychiatry Res 187:100–105. https://doi.org/10.1016/j.psychres.2010.10.007
Seidman LJ, Cherkerzian S, Goldstein JM et al (2013) Neuropsychological performance and family history in children at age 7 who develop adult schizophrenia or bipolar psychosis in the New England Family Studies. Psychol Med 43:119–131. https://doi.org/10.1017/S0033291712000773
Khandaker GM, Barnett JH, White IR, Jones PB (2011) A quantitative meta-analysis of population-based studies of premorbid intelligence and schizophrenia. Schizophr Res 132:220–227. https://doi.org/10.1016/j.schres.2011.06.017
Dickson H, Laurens KR, Cullen AE, Hodgins S (2012) Meta-analyses of cognitive and motor function in youth aged 16 years and younger who subsequently develop schizophrenia. Psychol Med 42:743–755. https://doi.org/10.1017/S0033291711001693
MacCabe JH, Lambe MP, Cnattingius S et al (2008) Scholastic achievement at age 16 and risk of schizophrenia and other psychoses: a National Cohort Study. Psychol Med 38:1133–1140. https://doi.org/10.1017/S0033291707002048
Hauser M, Zhang J-P, Sheridan EM et al (2017) Neuropsychological test performance to enhance identification of subjects at clinical high risk for psychosis and be most promising for predictive algorithms for conversion to psychosis: a meta-analysis. J Clin Psychiatry 78178:28–40. https://doi.org/10.4088/JCP.15r10197
Carrión RE, Goldberg TE, McLaughlin D et al (2011) Impact of neurocognition on social and role functioning in individuals at clinical high risk for psychosis. Am J Psychiatry 168:806–813. https://doi.org/10.1176/appi.ajp.2011.10081209
De Herdt A, Wampers M, Vancampfort D et al (2013) Neurocognition in clinical high risk young adults who did or did not convert to a first schizophrenic psychosis: a meta-analysis. Schizophr Res 149:48–55. https://doi.org/10.1016/j.schres.2013.06.017
Mayoral M, Zabala A, Robles O et al (2008) Neuropsychological functioning in adolescents with first episode psychosis: a 2-year follow-up study. Eur Psychiatry 23:375–383. https://doi.org/10.1016/j.eurpsy.2008.01.1420
Green MF (2006) Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatry 67:e12
Puig O, Baeza I, de la Serna E et al (2017) Persistent negative symptoms in first-episode psychosis. J Clin Psychiatry. https://doi.org/10.4088/JCP.16m11122
Penadés R, Catalán R, Puig O et al (2010) Executive function needs to be targeted to improve social functioning with Cognitive Remediation Therapy (CRT) in schizophrenia. Psychiatry Res 177:41–45. https://doi.org/10.1016/j.psychres.2009.01.032
Puig O, Penadés R, Gastó C et al (2008) Verbal memory, negative symptomatology and prediction of psychosocial functioning in schizophrenia. Psychiatry Res 158:11–17. https://doi.org/10.1016/j.psychres.2007.04.017
Kahn RS, Keefe RSE (2013) Schizophrenia is a cognitive illness. JAMA Psychiatry 70:1107. https://doi.org/10.1001/jamapsychiatry.2013.155
Bora E (2015) Neurodevelopmental origin of cognitive impairment in schizophrenia. Psychol Med 45:1–9. https://doi.org/10.1017/S0033291714001263
Ziermans TB, Schothorst PF, Sprong M, van Engeland H (2011) Transition and remission in adolescents at ultra-high risk for psychosis. Schizophr Res 126:58–64. https://doi.org/10.1016/j.schres.2010.10.022
Dickson H, Cullen AE, Reichenberg A et al (2014) Cognitive impairment among children at-risk for schizophrenia. J Psychiatr Res 50:92–99. https://doi.org/10.1016/j.jpsychires.2013.12.003
Addington J, Barbato M (2012) The role of cognitive functioning in the outcome of those at clinical high risk for developing psychosis. Epidemiol Psychiatr Sci 21:335–342. https://doi.org/10.1017/S204579601200042X
Seidman LJ, Mirsky AF (2017) Evolving notions of schizophrenia as a developmental neurocognitive disorder. J Int Neuropsychol Soc 23:881–892. https://doi.org/10.1017/S1355617717001114
Pukrop R, Klosterkötter J (2010) Neurocognitive indicators of clinical high-risk states for psychosis: a critical review of the evidence. Neurotox Res 18:272–286. https://doi.org/10.1007/s12640-010-9191-1
Karcher NR, O’Brien KJ, Kandala S, Barch DM (2019) Resting-state functional connectivity and psychotic-like experiences in childhood: results from the adolescent brain cognitive development study. Biol Psychiatry 86:7–15. https://doi.org/10.1016/j.biopsych.2019.01.013
Francey SM, Jackson HJ, Phillips LJ et al (2005) Sustained attention in young people at high risk of psychosis does not predict transition to psychosis. Schizophr Res 79:127–136. https://doi.org/10.1016/j.schres.2005.06.023
Perez VB, Shafer KM, Cadenhead KS (2012) Visual information processing dysfunction across the developmental course of early psychosis. Psychol Med 42:2167–2179. https://doi.org/10.1017/S0033291712000426
Gerritsen C, Maheandiran M, Lepock J et al (2019) Negative symptoms in the clinical high-risk state for psychosis: connection with cognition and primacy in impacting functioning. Early Interv Psychiatry. https://doi.org/10.1111/eip.12843
Leanza L, Egloff L, Studerus E et al (2018) The relationship between negative symptoms and cognitive functioning in patients at clinical high risk for psychosis. Psychiatry Res 268:21–27. https://doi.org/10.1016/j.psychres.2018.06.047
Meyer EC, Carrión RE, Cornblatt BA et al (2014) The relationship of neurocognition and negative symptoms to social and role functioning over time in individuals at clinical high risk in the first phase of the North American Prodrome Longitudinal Study. Schizophr Bull 40:1452–1461. https://doi.org/10.1093/schbul/sbt235
de Gracia DM, Viechtbauer W, Simons CJP et al (2009) Are psychotic psychopathology and neurocognition orthogonal? A systematic review of their associations. Psychol Bull 135:157–171. https://doi.org/10.1037/a0014415
Ventura J, Hellemann GS, Thames AD et al (2009) Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr Res 113:189–199. https://doi.org/10.1016/j.schres.2009.03.035
Schimmelmann BG, Michel C, Martz-Irngartinger A et al (2015) Age matters in the prevalence and clinical significance of ultra-high-risk for psychosis symptoms and criteria in the general population: findings from the BEAR and BEARS-kid studies. World Psychiatry 14:189–197. https://doi.org/10.1002/wps.20216
Armando M, Pontillo M, De CF et al (2015) Twelve-month psychosis-predictive value of the ultra-high risk criteria in children and adolescents. Schizophr Res 169:186–192. https://doi.org/10.1016/j.schres.2015.10.033
Thomas ML, Green MF, Hellemann G et al (2017) Modeling deficits from early auditory information processing to psychosocial functioning in schizophrenia. JAMA Psychiatry 74:37. https://doi.org/10.1001/jamapsychiatry.2016.2980
Vargas T, Ahmed AO, Strauss GP et al (2019) The latent structure of depressive symptoms across clinical high risk and chronic phases of psychotic illness. Transl Psychiatry 9:229. https://doi.org/10.1038/s41398-019-0563-x
Wigman JTW, van Nierop M, Vollebergh WAM et al (2012) Evidence that psychotic symptoms are prevalent in disorders of anxiety and depression, impacting on illness onset, risk, and severity—implications for diagnosis and ultra-high risk research. Schizophr Bull 38:247–257. https://doi.org/10.1093/schbul/sbr196
Häfner H, Maurer K, An Der Heiden W (2013) ABC schizophrenia study: an overview of results since 1996. Soc Psychiatry Psychiatr Epidemiol 48:1021–1031. https://doi.org/10.1007/s00127-013-0700-4
McCarthy JB, Weiss SR, Segovich KT, Barbot B (2016) Impact of psychotic symptoms on cognitive functioning in child and adolescent psychiatric inpatients with severe mood disorders. Psychiatry Res 244:223–228. https://doi.org/10.1016/j.psychres.2016.07.049
Schulze C, Zimmermann R, Gschwandtner U et al (2013) Can cognitive deficits facilitate differential diagnosis between at-risk mental state for psychosis and depressive disorders? Early Interv Psychiatry 7:381–390. https://doi.org/10.1111/eip.12004
Dohrenwend BP (1990) Socioeconomic status (SES) and psychiatric disorders. Soc Psychiatry Psychiatr Epidemiol 25:41–47. https://doi.org/10.1007/bf00789069
van Os J, Kenis G, Rutten BPF (2010) The environment and schizophrenia. Nature 468:203–212. https://doi.org/10.1038/nature09563
Miller GA, Chapman JP (2001) Misunderstanding analysis of co-variance. J Abnorm Psychol 110:40–48. https://doi.org/10.1037/0021-843X.110.1.40
Acknowledgements
This study was supported by Grants from the Carlos III Institute of Health, Spanish Department of Health, Instituto de Salud Carlos III (Fondo de Investigación Sanitaria PI11/1340; PI11/02684; PI15/0444 and PI15/00509), CIBERSAM Network and Fundación Alicia Koplowitz and FEDER “Otra manera de hacer Europa”. We thank the two anonymous reviewers whose comments and suggestions helped to improve this manuscript. Finally, we would like to thank all the participants in this study.
Funding
Study supported by grants from the Carlos III Institute of Health, Spanish Department of Health, Instituto de Salud Carlos III (Fondo de Investigación Sanitaria PI11/1349; PI11/02684; PI15/0444 and PI15/00509), CIBERSAM Network and Fundación Alicia Koplowitz.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jordina Tor has no conflict of interest. Anna Sintes-Estevez has no conflict of interest. Montserrat Dolz has received honoraria and travel support from Otsuka-Lundbeck and Janssen, research support from Fundación Alicia Koplowitz, and grants from the Spanish Ministry of Health, Instituto de Salud Carlos III. Olga Puig has no conflict of interest. Elena de la Serna has no conflict of interest. Marta Pardo has no conflict of interest. Daniel Muñoz-Samons has no conflict of interest. Marta Rodríguez-Pascual has no conflict of interest. Vanessa Sánchez-Gistau has no conflict of interest. Gisela Sugranyes has received honoraria from Lundbeck and Janssen, and research support from the Instituto de Salud Carlos III, Alicia Koplowitz Foundation, the Brain and Behaviour Foundation, and the Government of Catalonia (PERIS 2017). Inmaculada Baeza has received honoraria and travel support from Otsuka-Lundbeck and Janssen, research support from Fundación Alicia Koplowitz, and grants from the Spanish Ministry of Health, Instituto de Salud Carlos III.
Rights and permissions
About this article
Cite this article
Tor, J., Dolz, M., Sintes-Estevez, A. et al. Neuropsychological profile of children and adolescents with psychosis risk syndrome: the CAPRIS study. Eur Child Adolesc Psychiatry 29, 1311–1324 (2020). https://doi.org/10.1007/s00787-019-01459-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-019-01459-6