Abstract
Methylphenidate (MPH) is a common and effective treatment for attention deficit hyperactivity disorder (ADHD), but little is known about the relationship between early childhood intake of MPH and onset of antidepressant treatment during adolescence. The study aimed to examine whether adherence to MPH during early childhood predicts the initiation of antidepressants during adolescence. This is a 12-year historical prospective nationwide cohort study of children enrolled in an integrated care system who were first prescribed MPH between the ages of 6 and 8 years (N = 6830). We tested for an association between their adherence to MPH during early childhood (as indicated by medication possession ratio from MPH onset through the age of twelve) and the likelihood of being prescribed any antidepressant during adolescence (age 13–18). As all country citizens are covered by mandatory health insurance, and full services are provided by one of the four integrated care systems, data regarding patients’ diagnoses, prescriptions, and medical purchases are well documented. Logistic regression analysis indicated that those with higher adherence to MPH had a 50% higher risk (95% CI 1.16–1.93) of receiving antidepressants during adolescence when controlling for other comorbid psychiatric conditions and parental use of antidepressants. In this large-scale longitudinal study, MPH adherence during early childhood emerged as a predictor for antidepressant treatment during adolescence, which may reflect increased emotional and behavioral dysregulation in this group. The highly adherent patients are at higher risk and should be clinically monitored more closely, particularly into adolescence.

Similar content being viewed by others
References
APA (2013) The diagnostic and statistical manual of mental disorders. American Psychiatric Association, Arlington, VA
Barnard-Brak L, Roberts B, Valenzuela E (2018) Examining breaks and resistance in medication adherence among adolescents with ADHD as associated with school outcomes. J Attent Disord
Barner JC, Khoza S, Oladapo A (2011) ADHD medication use, adherence, persistence and cost among Texas Medicaid children. Curr Med Res Opin 27:13–22
Biederman J, Monuteaux MC, Spencer T, Wilens TE, Faraone SV (2009) Do stimulants protect against psychiatric disorders in youth with ADHD? A 10-year follow-up study. Pediatrics 124:71–78
Biederman J, Newcorn J, Sprich S (1991) Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. Am J Psychiatry 5:564–577
Bloch Y, Aviram S, Segev A, Nitzan U, Levkovitz Y, Braw Y, Mimouni Bloch A (2017) Methylphenidate reduces state anxiety during a continuous performance test that distinguishes adult ADHD patients from controls. J Atten Disord 21:46–51
Brinkman WB, Sherman SN, Zmitrovich AR, Visscher MO, Crosby LE, Phelan KJ, Donovan EF (2012) In their own words: adolescent views on ADHD and their evolving role managing medication. Acad Pediatr 12:53–61
Brinkman WB, Sucharew H, Majcher JH, Epstein JN (2018) Predictors of medication continuity in children with ADHD. Pediatrics 141:e20172580
Chilakamarri JK, Filkowski MM, Nassir Ghaemi S (2011) Misdiagnosis of bipolar disorder in children and adolescents: a comparison with ADHD and major depressive disorder. Ann Clin Psychiatry 23:25–29
Childress AC, Wigal SB, Brams MN, Turnbow JM, Pincus Y, Belden HW, Berry SA (2018) Efficacy and safety of amphetamine extended-release oral suspension in children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 28:306–313
Chinitz D, Shalev C, Galai N, Israeli A (1998) Israel's basket of health services: the importance of being explicitly implicit. BMJ 317:1005–1008
Clarfield AM, Manor O, Nun GB, Shvarts S, Azzam ZS, Afek A, Basis F, Israeli A (2017) Health and health care in Israel: an introduction. The Lancet 389: 2503-2513
Copeland W, Shanahan L, Erkanli A, Costello EJ, Angold A (2013) Indirect comorbidity in childhood and adolescence. Front Psychiatry 4:144
Coughlin CG, Cohen SC, Mulqueen JM, Ferracioli-Oda E, Stuckelman ZD, Bloch MH (2015) Meta-analysis: reduced risk of anxiety with psychostimulant treatment in children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 25:611–617
Daviss WB, Birmaher B, Diler RS, Mintz J (2008) Does pharmacotherapy for attention-deficit/hyperactivity disorder predict risk of later major depression? J Child Adolesc Psychopharmacol 18:257–264
Deshpande S, Quek RG, Forbes CA, de Kock S, Kleijnen J, Gandra SR, Simpson RJ Jr (2017) A systematic review to assess adherence and persistence with statins. Curr Med Res Opin 33:769–778
Gajria K, Lu M, Sikirica V, Greven P, Zhong Y, Qin P, Xie J (2014) Adherence, persistence, and medication discontinuation in patients with attention-deficit/hyperactivity disorder—a systematic literature review. Neuropsychiatr Dis Treat 10:1543
Gau S, Chen S-J, Chou W-J, Cheng H, Tang C-S, Chang H-L, Tzang R-F, Wu Y-Y, Huang Y-F, Chou M-C (2008) National survey of adherence, efficacy, and side effects of methylphenidate in children with attention-deficit/hyperactivity disorder in Taiwan. J Clin Psychiatry 69:131–140
Golubchik P, Kodesh A, Weizman A (2013) Attention-deficit/hyperactivity disorder and comorbid subsyndromal depression: what is the impact of methylphenidate on mood? Clin Neuropharmacol 36:141–145
Groenman AP, Schweren LJ, Dietrich A, Hoekstra PJ (2017) An update on the safety of psychostimulants for the treatment of attention-deficit/hyperactivity disorder. Expert Opin Drug Saf 16:455–464
Inglis SK, Carucci S, Garas P, Häge A, Banaschewski T, Buitelaar J, Dittmann R, Falissard B, Hollis C, Kovshoff H, ADDUCE Consortium (2016) Prospective observational study protocol to investigate long-term adverse effects of methylphenidate in children and adolescents with ADHD: the Attention Deficit Hyperactivity Disorder Drugs Use Chronic Effects (ADDUCE) study. BMJ open 6:e010433. https://doi.org/10.1136/bmjopen-2015-010433
Kortekaas-Rijlaarsdam AF, Luman M, Sonuga-Barke E, Oosterlaan J (2018) Does methylphenidate improve academic performance? A systematic review and meta-analysis. Eur Child Adolesc Psychiatry
Larson K, Russ SA, Kahn RS, Halfon N (2011) Patterns of comorbidity, functioning, and service use for US children with ADHD, 2007. Pediatrics 127:462–470
Lee H, Kim SW, Kim JM, Shin IS, Yang SJ, Yoon JS (2005) Comparing effects of methylphenidate, sertraline and placebo on neuropsychiatric sequelae in patients with traumatic brain injury. Hum Psychopharmacol Clin Exp 20:97–104
Lee MJ, Yang KC, Shyu YC, Yuan SS, Yang CJ, Lee SY, Lee TL, Wang L- (2016) Attention-deficit hyperactivity disorder, its treatment with medication and the probability of developing a depressive disorder: a nationwide population-based study in Taiwan. J Affect Disord 189:110–117
Lundervold AJ, Hinshaw SP, Sørensen L, Posserud M-B (2016) Co-occurring symptoms of attention deficit hyperactivity disorder (ADHD) in a population-based sample of adolescents screened for depression. Bmc Psychiatry 16(46):1–10
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG (2010) Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 67:220–229
Man KK, Coghill D, Chan EW, Lau WC, Hollis C, Liddle E, Banaschewski T, McCarthy S, Neubert A, Sayal K (2017) Association of risk of suicide attempts with methylphenidate treatment. Jama Psychiatry 74:1048–1055
Mannuzza S, Klein RG, Truong NL, Moulton PD III, John L, Roizen ER, Howell KH, Castellanos FX (2008) Age of methylphenidate treatment initiation in children with ADHD and later substance abuse: prospective follow-up into adulthood. Am J Psychiatry 165:604–609
Manor I, Gutnik I, Ben-Dor DH, Apter A, Sever J, Tyano S, Weizman A, Zalsman G (2010) Possible association between attention deficit hyperactivity disorder and attempted suicide in adolescents—a pilot study. Eur Psychiatry 25:146–150
McCabe SE, Dickinson K, West BT, Wilens TE (2016) Age of onset, duration, and type of medication therapy for attention-deficit/hyperactivity disorder and substance use during adolescence: a multi-cohort national study. J Am Acad Child Adolesc Psychiatry 55:479–486
Murray ML, Insuk S, Banaschewski T, Neubert AC, McCarthy S, Buitelaar JK, Coghill D, Dittmann RW, Konrad K, Panei P (2013) An inventory of European data sources for the long-term safety evaluation of methylphenidate. Eur Child Adolesc Psychiatry 22:605–618
Pappadopulos E, Jensen PS, Chait AR, Arnold LE, Swanson JM, Greenhill LL, Hechtman L, Chuang S, Wells KC, Pelham W (2009) Medication adherence in the MTA: saliva methylphenidate samples versus parent report and mediating effect of concomitant behavioral treatment. J Am Acad Child Adolesc Psychiatry 48:501–510
Patel NC, Crismon ML, Hoagwood K, Johnsrud MT, Rascati KL, Wilson JP, Jensen PS (2005) Trends in the use of typical and atypical antipsychotics in children and adolescents. J Am Acad Child Adolesc Psychiatry 44:548–556
Rasmussen K, Palmstierna T, Levander S (2015) Differences in psychiatric problems and criminality between individuals treated with central stimulants before and after adulthood. J Atten Disord :1–8
Reale L, Bartoli B, Cartabia M, Zanetti M, Costantino MA, Canevini MP, Termine C, Bonati M, Group LA (2017) Comorbidity prevalence and treatment outcome in children and adolescents with ADHD. Eur Child Adolesc Psychiatry 26:1443–1457
Scholle O, Banaschewski T, Enders D, Garbe E, Riedel O (2018) Use and characteristics of antipsychotic/methylphenidate combination therapy in children and adolescents with a diagnosis of attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 28:306–313
Schrantee A, Bouziane C, Bron E, Klein S, Bottelier M, Kooij J, Rombouts S, Reneman L (2017) Long-term effects of stimulant exposure on cerebral blood flow response to methylphenidate and behavior in attention-deficit hyperactivity disorder. Brain Imaging and Behavior:1–9
Schrantee A, Tamminga HG, Bouziane C, Bottelier MA, Bron EE, Mutsaerts H-JM, Zwinderman AH, Groote IR, Rombouts SA, Lindauer RJ (2016) Age-dependent effects of methylphenidate on the human dopaminergic system in young vs adult patients with attention-deficit/hyperactivity disorder: a randomized clinical trial. JAMA Psychiatry 73:955–962
Shaw P, Stringaris A, Nigg J, Leibenluft E (2014) Emotion dysregulation in attention deficit hyperactivity disorder. Am J Psychiatry 171:276–293
Song Q-Y, Guo L-T (2013) Trends in the prescribing of psychotropic medications for inpatient children and adolescents, 2000–2010: a study from China. Int Clin Psychopharmacol 28:193–199
Spencer TJ, Biederman J, Mick E (2007) Attention-deficit/hyperactivity disorder: diagnosis, lifespan, comorbidities, and neurobiology. Ambul Pediatr 7:73–81
Subcommittee on Attention-Deficit, Hyperactivity Disorder; Steering Committee on Quality Improvement and Management WM, Brown L, Brown RT, DuPaul G, Earls M, Feldman HM, Ganiats TG, Kaplanek B, Meyer B, Perrin J, Pierce K, Reiff M, Stein MT, Visser S. (2011) ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics 128:2011–2654
Tamblyn R, Lavoie G, Petrella L, Monette J (1995) The use of prescription claims databases in pharmacoepidemiological research: the accuracy and comprehensiveness of the prescription claims database in Quebec. J Clin Epidemiol 48:999–1009
Thomas R, Sanders S, Doust J, Beller E, Glasziou P (2015) Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics 135:e994–e1001
Toomey SL, Sox CM, Rusinak D, Finkelstein JA (2012) Why do children with ADHD discontinue their medication? Clin Pediatr 51:763–769
Urban KR, Gao WJ (2014) Performance enhancement at the cost of potential brain plasticity: neural ramifications of nootropic drugs in the healthy developing brain. Front Syst Neurosci 8:38
Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, Perou R, Blumberg SJ (2014) Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. J Am Acad Child Adolesc Psychiatry 53(34–46):e32
Wang LJ, Shyu YC, Yuan SS, Yang CJ, Yang KC, Lee T-, Lee SY (2016) Attention-deficit hyperactivity disorder, its pharmacotherapy, and the risk of developing bipolar disorder: A nationwide population-based study in Taiwan. J Psychiatr Res 72:6–14
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Appendix A
Appendix A
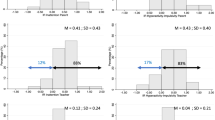
Variables included in the final model predicting dispensed prescription of ADM (unadjusted).
Variable | Coefficient | 95% CI |
|---|---|---|
MPH adherence | 1.26 | 1.04–1.52 |
Antipsychotics | 1.98 | 1.65–2.39 |
Parental ADM use | 3.51 | 2.81–4.36 |
Rights and permissions
About this article
Cite this article
Madjar, N., Shlosberg, D., Leventer-Roberts, M. et al. Childhood methylphenidate adherence as a predictor of antidepressants use during adolescence. Eur Child Adolesc Psychiatry 28, 1365–1373 (2019). https://doi.org/10.1007/s00787-019-01301-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-019-01301-z