Abstract
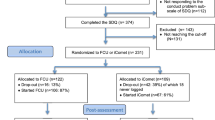
Externalizing problem behaviour is one of the most common childhood disorders. Parent training is an effective treatment for these children and there is growing interest in the effects of parent-administered interventions with minimal therapist contact. This randomized controlled study examined the efficacy of a telephone-assisted parent-administered behavioural intervention (bibliotherapy) in families with preschool children with externalizing problem behaviour. Families were randomly assigned to a treatment group (n = 26) and an untreated waitlist control group (n = 22). The intervention comprised the reading of an 11 chapter self-help book and 11 weekly telephone consultations. Compared to the control group, the treatment group demonstrated significant decreases in parent-reported externalizing and internalizing child problem behaviour and dysfunctional parenting practices. Moreover, treated parents reported less parenting-related strains and decreases in parental depression, anxiety, and stress. The results suggest that telephone-assisted self-administered parent training is an effective alternative to more intensive forms of behavioural family intervention for preschool children with externalizing problem behaviour.



Similar content being viewed by others

References
Bongers IL, Koot HM, Van Der Ende J, Verhulst FC (2004) Developmental trajectories of externalizing behaviors in childhood and adolescence. Child Dev 75:1523–1537. doi:10.1111/j.1467-8624.2004.00755.x
Lahey BB, Miller TL, Gordon RA, Riley AW (1999) Developmental epidemiology of the disruptive behavior disorders. In: Quay HC, Hogan A (eds) Handbook of the disruptive behavior disorders. Plenum, New York, pp 23–48
Nock MK, Kazdin AE, Hiripi E, Kessler RC (2007) Lifetime prevalence, correlates, and persistence of oppositional defiant disorder: results from the National Comorbidity Survey Replication. J Child Psychol Psychiatry 48:703–713. doi:10.1111/j.1469-7610.2007.01733.x
McCord J, Widom CS, Crowell NE (2001) Juvenile crime, juvenile justice. National Academy Press, Washington, DC
Tremblay RE (2000) The development of aggressive behavior during childhood: what have we learned in the past century? Int J Behav Dev 24:129–141. doi:10.1080/016502500383232
Kaminski JW, Valle LA, Filene JH, Boyle CL (2008) A meta-analytic review of components associated with parent training program effectiveness. J Abnorm Child Psychol 36:567–589. doi:10.1007/s10802-007-9201-9
Eyberg SM, Nelson MM, Boggs SR (2008) Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. J Clin Child Adolesc Psychol 37:215–237. doi:10.1080/15374410701820117
Farmer EMZ, Compton SN, Burns JB, Robertson E (2002) Review of the evidence base for treatment of childhood psychopathology: externalizing disorders. J Consult Clin Psychol 70:1267–1302. doi:10.1037/0022-006X.70.6.1267
Piquero AR, Farrington DP, Welsh BC, Tremblay R, Jennings WG (2009) Effects of early family/parent training programs on antisocial behavior and delinquency. J Exp Criminol 5:83–120. doi:10.1007/s11292-009-9072-x
Sanders MR (2012) Development, evaluation, and multinational dissemination of the triple p-positive parenting program. Annual Rev Clin Psychol 8:345–379. doi:10.1146/annurev-clinpsy-032511-143104
Sonuga-Barke EJ, Daley D, Thompson M (2002) Does maternal ADHD reduce the effectiveness of parent training for preschool children’s ADHD? J Am Acad Child Adolesc Psychiatry 40:402–408. doi:10.1097/00004583-200206000-00009
Van Zeijl J, Mesman J, Van IJzendoorn MH, Bakermans-Kranenburg MJ, Juffer F, Stolk MN, Koot HM, Alink LRA (2006) Attachment-based intervention for enhancing sensitive discipline in mothers of 1- to 3-year-old children at risk for externalizing behavior problems: A randomized controlled trial. J Consult Clin Psychol 74:994–1005. doi:10.1037/0022-006X.74.6.994
Döpfner M, Breuer D, Schurmann S, Wolff Metternich T, Rademacher C, Lehmkuhl G (2004) Effectiveness of an adaptive multimodal treatment in children with attention-deficit hyperactivity disorder—global outcome. Eur Child Adolesc Psychiatry 13(Suppl 1):I117–I129. doi:10.1007/s00787-004-1011-9
Hanisch C, Plück J, Meyer N, Brix G, Freund-Braier I, Hautmann C, Döpfner M (2006) Kurzzeiteffekte des indizierten Präventionsprogramms für Expansives Problemverhalten (PEP) auf das elterliche Erziehungsverhalten und auf das kindliche Problemverhalten [Short-term effects of the indicated Prevention Programme for externalizing Problem Behaviour (PEP)]. Z Klin Psychol Psychother 35:117–126. doi:10.1026/1616-3443.35.2.117
Hanisch C, Freund-Braier I, Hautmann C, Jänen N, Plück J, Brix G, Eichelberger I, Döpfner M (2010) Detecting effects of the indicated prevention programme for externalizing problem behaviour (PEP) on child symptoms, parenting, and parental quality of life in a randomized controlled trial. Behav Cogn Psychother 38:95–112. doi:10.1017/S1352465809990440
Hautmann C, Hanisch C, Mayer I, Plück J, Döpfner M (2008) Effectiveness of the prevention program for externalizing problem behaviour (PEP) in children with symptoms of attention deficit/hyperactivity disorder and oppositional defiant disorder—generalization to the real world. J Neural Transm 115:363–370. doi:10.1007/s00702-007-0866-6
Hautmann C, Hoijtink H, Eichelberger I, Görtz-Dorten A, Hanisch C, Plück J, Walter D, Döpfner M (2012) Any indication for bias due to participation? Comparison of the effects of a parent management training rated by participating and non-participating parent. Clin Psychol Psychother. doi:10.1002/cpp.1784 (published online 24 feb 2012)
Hutchings J, Bywater T, Daley D, Gardner F, Whitaker C, Jones K, Eames C, Edwards RT (2007) Parenting intervention in Sure Start services for children at risk of developing conduct disorder: pragmatic randomised controlled trial. Br Med J 334:678. doi:10.1136/bmj.39126.620799.55
Webster-Stratton C, Reid MJ, Hammond M (2004) Treating children with early-onset conduct problems: intervention outcomes for parent, child, and teacher training. J Clin Child Adolesc Psychol 33:105–124. doi:10.1207/S15374424JCCP3301_11
Kazdin AE, Holland L, Crowley M (1997) Family experience of barriers to treatment and premature termination from child therapy. J Consult Clin Psychol 65:453–463. doi:10.1037/0022-006X.65.3.453
Frude N (2004) Bibliotherapy as a means of delivering psychological therapy. Clin Psychol 39:8–10
McKenna G, Hevey D, Martin E (2010) Patients’ and providers’ perspectives on bibliotherapy in primary care. Clin Psychol Psychother 17:497–509. doi:10.1002/cpp.679
Gregory RJ, Canning SS, Lee TW, Wise JC (2004) Cognitive bibliotherapy for depression: a meta-analysis. Prof Psychol Res Pract 35:275–280. doi:10.1037/0735-7028.35.3.275
Lovell K, Ekers D, Fulford A, Baguley C, Bradshaw TJ (2004) A pilot study of a self-help manual with minimal therapist contact in the treatment of obsessive–compulsive disorder. Clin Eff Nurs 8:122–127. doi:10.1016/j.cein.2004.05.004
Morin CM, Mineault V, Gagne A (1999) Nonpharmacological treatment of late-life insomnia. J Psychosom Res 46:103–116. doi:10.1016/S0022-3999(98)00077-4
Scogin F, Bynum J, Stephens G, Calhoon S (1990) Efficacy of self-administered treatment programs: meta-analytic review. Prof Psychol Res Pract 21:42–47. doi:10.1037/0735-7028.21.1.42
Creswell C, Hentges F, Parkinson M, Sheffield P, Willetts L, Cooper P (2010) Feasibility of guided cognitive behaviour therapy (CBT) self-help for childhood anxiety disorders in primary care. Ment Health Fam Med 7:49–57
Leong J, Cobham VE, De Groot J, McDermott B (2009) Comparing different modes of delivery: a pilot evaluation of a family-focused, cognitive-behavioral intervention for anxiety-disordered children. Eur Child Adolesc Psychiatry 18:231–239. doi:10.1007/s00787-008-0723-7
Lyneham HJ, Rapee RM (2006) Evaluation of therapist-supported parent-implemented CBT for anxiety disorders in rural children. Behav Res Ther 44:1287–1300. doi:10.1016/j.brat.2005.09.009
McGrath PJ, Lingley-Pottie P, Thurston C, MacLean C, Cunningham C, Waschbusch DA, Watters C, Stewart S, Bagnell A, Santor D, Chaplin W (2011) Telephone-based mental health interventions for child disruptive behavior or anxiety disorders: randomized trials and overall analysis. J Am Acad Child Adolesc Psychiatry 50:1162–1172. doi:10.1016/j.jaac.2011.07.013
Lavigne JV, LeBailly SA, Gouze KR, Cicchetti C, Pochyly J, Arend R, Jessup BW, Binns HJ (2008) Treating oppositional defiant disorder in primary care: a comparison of three models. J Pediatr Psychol 33:449–461. doi:10.1093/jpepsy/jsm074
Swift MC, Roeger L, Walmsley C, Howard S, Furber G, Allison S (2009) Rural children referred for conduct problems: evaluation of a collaborative program. Aust J Prim Health 15:335–340. doi:10.1071/PY09029
Elgar FJ, McGrath PJ (2003) Self-administered psychosocial treatments for children and families. J Clin Psychol 59:321–339. doi:10.1002/jclp.10132
O’Brien M, Daley D (2011) Self-help parenting interventions for childhood behaviour disorders: a review of the evidence. Child Care Health Dev 37:623–637. doi:10.1111/j.1365-2214.2011.01231.x
Sanders MR, Bor W, Morawska A (2007) Maintenance of treatment gains: a comparison of enhanced, standard, and self-directed triple p-positive parenting program. J Abnorm Child Psychol 35:983–998. doi:10.1007/s10802-007-9148-x
Feldmann M, Heinrichs N, Hahlweg K, Betram H (2007) Bibliotherapie zur Verbesserung elterlicher Erziehungskompetenz: eine randomisierte Evaluationsstudie [Bibliotherapy to improve parental competency: a randomized evaluation study]. Verhaltenstherapie 17:26–35. doi:10.1159/000099629
Forehand RL, Merchant MJ, Long N, Garai E (2010) An examination of parenting the strong-willed child as bibliotherapy for parents. Behav Modif 34:57–76. doi:10.1177/0145445509356351
Hahlweg K, Heinrichs N, Kuschel A, Feldmann Albers M (2008) Therapist-assisted, self-administered bibliotherapy to enhance parental competence. Behav Modif 32:659–681. doi:10.1177/0145445508317131
Morawska A, Sanders MR (2006) Self-administered behavioral family intervention for parents of toddlers: Part I. Efficacy. J Consult Clin Psychol 74:10–19. doi:10.1037/0022-006X.74.1.10
Döpfner M, Schürmann S, Lehmkuhl G (2011) Wackelpeter & Trotzkopf. Hilfen für Eltern bei ADHS-Symptomen, hyperkinetischem und oppositionellem Verhalten, 4th edn. Beltz, Weinheim
Döpfner M, Schürmann S, Frölich J (2007) Therapieprogramm für Kinder mit hyperkinetischem und oppositionellem Problemverhalten (THOP), 4th edn. Beltz, Weinheim
Markie-Dadds C, Sanders MR (2006) Self-directed triple P (positive parenting program) for mothers with children at-risk of developing conduct problems. Behav Cogn Psychother 34:259–275. doi:10.1017/S1352465806002797
Sanders MR, Markie-Dadds C, Tully LA, Bor W (2000) The triple P-positive parenting program: a comparison of enhanced, standard, and self-directed behavioral family intervention for parents of children with early onset conduct problems. J Consult Clin Psychol 68:624–640. doi:10.1037/0022-006X.68.4.624
Webster-Stratton C, Kolpacoff M, Hollinsworth T (1988) Self-administered videotape therapy for families with conduct-problem children: comparison with two cost-effective treatments and a control group. J Consult Clin Psychol 56:558–566. doi:10.1037/0022-006X.56.4.558
Kierfeld F, Döpfner M (2006) Bibliotherapie als Behandlungsmöglichkeit bei Kindern mit externalen Verhaltensstörungen [Bibliotherapy as a self-help program for parents of children with externalizing problem behavior]. Z Kinder Jugendpsychiatrie 34:377–386. doi:10.1024/1422-4917.34.5.377
Wolff Metternich T, Plück J, Wieczorrek E, Freund-Braier I, Hautmann C, Brix G, Döpfner M (2002) PEP—Ein Präventionsprogramm für drei- bis sechsjährige Kinder mit expansivem Problemverhalten [PEP—a prevention program for 3- to 6-year-old children with externalizing problem behavior]. Kindheit und Entwicklung 11:98–106. doi:10.1026//0942-5403.11.2.98
Achenbach TM (1991) Manual for the Child Behaviour Checklist 4–18 and 1991 profile. University of Vermont, Burlington
Arbeitsgruppe Deutsche Child Behavior Checklist (1998) Elternfragebogen über das Verhalten von Kindern und Jugendlichen; deutsche Bearbeitung der Child Behavior Checklist (CBCL/4-18). Einführung und Anleitung zur Handauswertung mit deutschen Normen, bearbeitet von M Döpfner, J Plück, S Bölte, K Lenz, P Melchers, K Heim, 2nd edn. Arbeitsgruppe Kinder-, Jugend- und Familiendiagnostik (KJFD), Köln
Plück J, Hautmann C, Brix G, Freund-Braier I, Hahlweg K, Döpfner M (2008) Screening von Expansivem Problemverhalten bei Kindern im Kindergartenalter für Eltern und Erzieherinnen (PEP-Screen) [Screening of externalising behavior in preschool children for parents and educators]. Diagnostica 54:138–149. doi:10.1026/0012-1924.54.3.138
Arbeitsgruppe Deutsche Child Behavior Checklist (2002) Elternfragebogen für Klein- und Vorschulkinder (CBCL/1½–5). Deutsche Bearbeitung der Child Behavior Checklist 1½–5; bearbeitet von J Plück, M Döpfner. Arbeitsgruppe Kinder-, Jugend- und Familiendiagnostik (KJFD), Köln
Döpfner M, Görtz-Dorten A, Lehmkuhl G (2008) Diagnostik-System für psychische Störungen nach ICD-10 und DSM-IV für Kinder- und Jugendliche (DISYPS-II). Huber, Bern
Erhart M, Döpfner M, Ravens-Sieberer U, Bella Study Group (2008) Psychometric properties of two ADHD questionnaires: comparing the Conners’ scale and the FBB-HKS in the general population of German children and adolescents—results of the BELLA study. Eur Child Adolesc Psychiatry 17(supplement 1):106–115. doi:10.1007/s00787-008-1012-1
Görtz-Dorten A, Ise E, Hautmann C, Walter D, Döpfner M (submitted). Psychometric properties of a German parent rating scale for ODD and CD (FBB-SSV) in clinical and community samples
Barkley RA (1981) Hyperactive children: a handbook for diagnosis and treatment. Guildford, New York
Breuer D, Döpfner M (1997) Die Erfassung von problematischen Situationen in der Familie. Praxis der Kinderpsychologie und Kinderpsychiatrie 46:583–596
Strayhorn JM, Weidman CS (1988) A parent practices scale and its relation to parent and child mental health. J Am Acad Child Adolesc Psychiatry 27:613–618. doi:10.1097/00004583-198809000-00016
Miller Y (2001) Erziehung von Kindern im Kindergartenalter. Erziehungsverhalten und Kompetenzüberzeugungen von Eltern und der Zusammenhang zu kindlichen Verhaltensstörungen. Dissertation, University Braunschweig, Germany
Arnold DS, O’Leary SG, Wolff LS, Acker MM (1993) The Parenting Scale: a measure of dysfunctional parenting in discipline situations. Psychol Assess 5:137–144. doi:10.1037/1040-3590.5.2.137
Sanders MR, Woolley ML (2001) Parenting Tasks Checklist. PFSC, Brisbane
Lovibond SH, Lovibond PF (1995) Manual for the Depression Anxiety Stress Scales, 2nd edn. Psychology Foundation of Australia, Sydney
Lovibond PF, Lovibond SH (1995) The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 33:335–342
Majoros K (2001) Belastung ohne Ende? Die Entwicklung eines Belastungsfragebogens für Eltern mit hyperaktiven Kindern. Diploma, Julius-Maximillians University, Würzburg, Germany
Dadds MR, Powell MB (1991) The relationship of interparental conflict and global marital adjustment to aggression, anxiety, and immaturity in aggressive nonclinic children. J Abnorm Child Psychol 19:553–567. doi:10.1007/BF00925820
Heinrichs N, Bertram H, Kuschel A, Hahlweg K (2005) Parent recruitment and retention in a universal prevention program for child behavior and emotional problems: barriers to research and program participation. Prev Sci 6:275–286. doi:10.1007/s11121-005-0006-1
Connell S, Sanders MR, Markie-Dadds C (1997) Self-directed behavioral family intervention for parents of oppositional children in rural and remote areas. Behav Modif 21:79–408. doi:10.1177/01454455970214001
Schuhmann EM, Foote RC, Eyberg SM, Boggs SR, Algina J (1998) Efficacy of a parent-child interaction therapy: interim report of a randomized trial with short-term maintenance. J Clin Child Psychol 27:34–45. doi:10.1207/s15374424jccp2701_4
Lavigne JV, LeBailly SA, Gouze KR, Binns HJ, Keller J, Pate L (2010) Predictors and correlates of completing behavioral parent training for the treatment of oppositional defiant disorder in pediatric primary care. Behav Ther 41:198–211. doi:10.1016/j.beth.2009.02.006
Plück J, Freund-Braier I, Hautmann C, Beckers G, Wieczorrek E, Döpfner M (2010) Recruitment in an indicated prevention program for externalizing behavior—parental participation decisions. Child Adolesc Psychiatry Ment Health 4:15. doi:10.1186/1753-2000-4-15
Cunningham MJ, Wuthrich V (2008) Examination of barriers to treatment and used preferences with computer-based therapy using The Cool Teens CD for adolescent anxiety. E-J Appl Psychol 4:12–17
Williams C (2001) Use of written cognitive-behavioural therapy self-help materials to treat depression. Adv Psychiatric Treat 7:233–240. doi:10.1192/apt.7.3.233
Conflict of interest
Manfred Döpfner served in an advisory or consultancy role for Lilly, Medice, Novartis, Shire and Viforpharma. He received conference attendance support and conference support or received speaker’s fee by Lilly, Medice, Novartis and Shire. He is/has been involved in clinical trials conducted by Lilly and Vifor. He receives honorary as author of books and treatment manuals on child behaviour therapy and self-help.
Author information
Authors and Affiliations
Corresponding author
Additional information
F. Kierfeld and E. Ise contributed equally to the manuscript and are both considered as first author.
The work reported in this paper was done in partial fulfilment of the F. Kierfeld’s dissertation at University of Cologne, Germany.
Rights and permissions
About this article
Cite this article
Kierfeld, F., Ise, E., Hanisch, C. et al. Effectiveness of telephone-assisted parent-administered behavioural family intervention for preschool children with externalizing problem behaviour: a randomized controlled trial. Eur Child Adolesc Psychiatry 22, 553–565 (2013). https://doi.org/10.1007/s00787-013-0397-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-013-0397-7