Abstract
Objective
This study used image-based finite element analysis (FEA) to assess the biomechanical changes in mandibular first molars resulting from alterations in the position of the root canal isthmus.
Methods
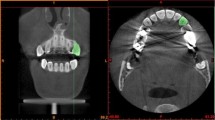
A healthy mandibular first molar, characterized by two intact root canals and a cavity-free surface, was selected as the subject. A three-dimensional model for the molar was established using scanned images of the patient's mandibular teeth. Subsequently, four distinct finite element models were created, each representing varied root canal morphologies: non-isthmus (Group A), isthmus located at the upper 1/3 of the root (Group B), middle 1/3 of the root (Group C), and lower 1/3 of the root (Group D). A static load of 200 N was applied along the tooth's longitudinal axis on the occlusal surface to simulate regular chewing forces. The biomechanical assessment was conducted regarding the mechanical stress profile within the root dentin. The equivalent stress (Von Mises stress) was used to assess the biomechanical features of mandibular teeth under mechanical loading.
Results
In Group A (without an isthmus), the maximum stress was 22.2 MPa, while experimental groups with an isthmus exhibited higher stresses, reaching up to 29.4 MPa. All maximum stresses were concentrated near the apical foramen. The presence of the isthmus modified the stress distribution in the dentin wall of the tooth canal. Notably, dentin stresses at specific locations demonstrated differences: at 8 mm from the root tip, Group B: 13.6 MPa vs. Group A: 11.4 MPa; at 3 mm from the root tip, Group C: 14.2 MPa vs. Group A: 4.5 MPa; at 1 mm from the root tip, Group D: 25.1 MPa vs. Group A: 10.3 MPa. The maximum stress in the root canal dentin within the isthmus region was located either at the top or bottom of the isthmus.
Conclusion
A root canal isthmus modifies the stress profile within the dentin. The maximum stress occurs near the apical foramen and significantly increases when the isthmus is located closer to the apical foramina.







Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Yang SF, Rivera EM, Walton RE (1995) Vertical root fracture in nonendodontically treated teeth. J Endod 21:337–339. https://doi.org/10.1016/s0099-2399(06)81013-7
Yeh CJ (1997) Fatigue root fracture: a spontaneous root fracture in non-endodontically treated teeth. Br Dent J 182:261–266. https://doi.org/10.1038/sj.bdj.4809363
Barreto MS, Moraes RA, Rosa RA, Moreira CH, Só MV, Bier CA (2012) Vertical root fractures and dentin defects: effects of root canal preparation, filling, and mechanical cycling. J Endod 38:1135–1139. https://doi.org/10.1016/j.joen.2012.05.002
Sabeti M, Kazem M, Dianat O, Bahrololumi N, Beglou A, Rahimipour K, Dehnavi F (2018) Impact of access cavity design and root canal taper on fracture resistance of endodontically treated teeth: an ex vivo investigation. J Endod 44:1402–1406. https://doi.org/10.1016/j.joen.2018.05.006
Xu HP, Fu J, Deng J, Zheng QH, Zhou W, Huang DM (2018) Effect of occlusal slope related to uneven attrition on root stress distribution and potential fracture. J Dent Sci 13:367–373. https://doi.org/10.1016/j.jds.2018.06.006
Chan CP, Lin CP, Tseng SC, Jeng JH (1999) Vertical root fracture in endodontically versus nonendodontically treated teeth: a survey of 315 cases in Chinese patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 87:504–507. https://doi.org/10.1016/s1079-2104(99)70252-0
Liao WC, Chen CH, Pan YH, Chang MC, Jeng JH (2021) Vertical Root Fracture in Non-Endodontically and Endodontically Treated Teeth: Current Understanding and Future Challenge. J Pers Med 11. https://doi.org/10.3390/jpm11121375
Patel S, Bhuva B, Bose R (2022) Present status and future directions: vertical root fractures in root filled teeth. Int Endod J 55 Suppl 3:804–826. https://doi.org/10.1111/iej.13737
Mizuhashi F, Ogura I, Sugawara Y, Oohashi M, Mizuhashi R, Saegusa H (2021) Diagnosis of root fractures using cone-beam computed tomography: difference of vertical and horizontal root fracture. Oral Radiol 37:305–310. https://doi.org/10.1007/s11282-020-00453-y
PradeepKumar AR, Shemesh H, Jothilatha S, Vijayabharathi R, Jayalakshmi S, Kishen A (2016) Diagnosis of Vertical Root Fractures in Restored Endodontically Treated Teeth: A Time-dependent Retrospective Cohort Study. J Endod 42:1175–1180. https://doi.org/10.1016/j.joen.2016.04.012
von Arx T, Maldonado P, Bornstein MM (2021) Occurrence of Vertical Root Fractures after Apical Surgery: A Retrospective Analysis. J Endod 47:239–246. https://doi.org/10.1016/j.joen.2020.10.012
von Arx T, Bosshardt D (2017) Vertical root fractures of endodontically treated posterior teeth: A histologic analysis with clinical and radiographic correlates. Swiss Dent J 127:14–23
Weller RN, Niemczyk SP, Kim S (1995) Incidence and position of the canal isthmus. Part 1. Mesiobuccal root of the maxillary first molar. J Endod 21:380–383. https://doi.org/10.1016/s0099-2399(06)80975-1
Estrela C, Rabelo LE, de Souza JB, Alencar AH, Estrela CR, Sousa Neto MD, Pécora JD (2015) Frequency of Root Canal Isthmi in Human Permanent Teeth Determined by Cone-beam Computed Tomography. J Endod 41:1535–1539. https://doi.org/10.1016/j.joen.2015.05.016
Kyaw Moe MM, Jo HJ, Ha JH, Kim SK (2021) Root Canal Configuration of Burmese (Myanmar) Maxillary First Molar: A Micro-Computed Tomography Study. Int J Dent 2021:3433343. https://doi.org/10.1155/2021/3433343
de Pablo OV, Estevez R, Péix Sánchez M, Heilborn C, Cohenca N (2010) Root anatomy and canal configuration of the permanent mandibular first molar: a systematic review. J Endod 36:1919–1931. https://doi.org/10.1016/j.joen.2010.08.055
Natanasabapathy V, Rajesh PS, Ashritha MCV, Mishra A, Namasivayam A, Kandaswamy D, Srinivasan MR (2020) Root canal isthmi and interorifice distance in human permanent teeth of an Indian subpopulation using cone-beam computed tomography: A retrospective cross-sectional study. J Conserv Dent 23:563–570. https://doi.org/10.4103/jcd.Jcd_576_20
Chai H, Tamse A (2015) The effect of isthmus on vertical root fracture in endodontically treated teeth. J Endod 41:1515–1519. https://doi.org/10.1016/j.joen.2015.04.003
Zeng Y, Wang JD (2005)[Establishment of the three-dimensional finite element model of the first permanent mandibular molar and its stress analysis]. Chinese. Zhonghua Kou Qiang Yi Xue Za Zhi 40:394–397.
Wang ZF, Fu BP (2022) Minimum residual root dentin thickness of mandibular premolars restored with a post: A finite element analysis study. J Prosthet Dent. https://doi.org/10.1016/j.prosdent.2022.03.024
Ma D, Qian J (2023) Three-dimensional finite element stress analysis of surface-mounted inlays in repairing pulp-penetrating non-carious cervical lesion of maxillary first premolar. Hua Xi Kou Qiang Yi Xue Za Zhi 41:541–553. https://doi.org/10.7518/hxkq.2023.2023123
Ferrario VF, Sforza C, Serrao G, Dellavia C, Tartaglia GM (2004) Single tooth bite forces in healthy young adults. J Oral Rehabil 31:18–22. https://doi.org/10.1046/j.0305-182x.2003.01179.x
Fu Y, Zhang L, Gao Y, Huang D (2022) A Comparison of Volume of Tissue Removed and Biomechanical Analysis of Different Access Cavity Designs in 2-rooted Mandibular First Molars: A Multisample 3-dimensional Finite Element Analysis. J Endod 48:362–369. https://doi.org/10.1016/j.joen.2021.12.007
Murakami N, Wakabayashi N (2014) Finite element contact analysis as a critical technique in dental biomechanics: a review. J Prosthodont Res 58:92–101. https://doi.org/10.1016/j.jpor.2014.03.001
Sugaya T, Nakatsuka M, Inoue K, Tanaka S, Miyaji H, Sakagami R, Kawamami M (2015) Comparison of fracture sites and post lengths in longitudinal root fractures. J Endod 41:159–163. https://doi.org/10.1016/j.joen.2014.09.017
Ou KL, Chang CC, Chang WJ, Lin CT, Chang KJ, Huang HM (2009) Effect of damping properties on fracture resistance of root filled premolar teeth: a dynamic finite element analysis. Int Endod J 42:694–704. https://doi.org/10.1111/j.1365-2591.2009.01570.x
Savruk P, Andrzej K (2016) Stress concentration near sharp and rounded V-notches in orthotropic and quasi-orthotropic bodies. Theoretical and Applied Fracture Mechanics. 84: 166–176. https://doi.org/10.1016/j.tafmec.2016.02.006
Zhou Y, Hu Z, Hu Y, Gao A, Pan X, Tang R, Lin Z (2023) Patterns of stress distribution of endodontically treated molar under different types of loading using finite element models-the exploring of mechanism of vertical root fracture. J Mech Behav Biomed Mater 144:105947. https://doi.org/10.1016/j.jmbbm.2023.105947
Cecchin D, Soares Giaretta V, Granella Cadorin B, Albino Souza M, Vidal CMP, Paula Farina A (2017) Effect of synthetic and natural-derived novel endodontic irrigant solutions on mechanical properties of human dentin. J Mater Sci Mater Med 28:141. https://doi.org/10.1007/s10856-017-5960-1
Abdulsamad Alskaf MK, Achour H, Alzoubi H (2022) The Effect of Bioceramic HiFlow and EndoSequence Bioceramic Sealers on Increasing the Fracture Resistance of Endodontically Treated Teeth: An In Vitro Study. Cureus 14:e33051. https://doi.org/10.7759/cureus.33051
Lertchirakarn V, Palamara JE, Messer HH (1999) Load and strain during lateral condensation and vertical root fracture. J Endod 25:99–104. https://doi.org/10.1016/s0099-2399(99)80005-3
Acknowledgements
We also thank Medjaden Inc. for its assistance in the preparation of this manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (No.81960207).
Author information
Authors and Affiliations
Contributions
Conceptualization, SH Li and QT Yao; Software, YM Zhuang and Yaerken Aji; methodology, SH Li , QT Yao and Yaerken Aji; investigation, QT Yao, QL Zhang, and YX Luo; project administration, SH Li and YM Zhuang; writing–original draft, SH Li, QT Yao, and YM Zhuang; writing–review and editing, SH Li, QT Yao, YM Zhuang, and Yaerken Aji. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the People's Hospital of the Xinjiang Uygur Autonomous Region (No. KY2018011852). Informed consent was obtained from the patient before sample collection.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
1. Developing finite element models with isthmus at various locations within root canals.
2. Offering in-depth insights into the biomechanical characteristics of mandibular molars.
3. Evaluating the biomechanical effects of the varied isthmus positions within root canals.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yao, Q., Zhuang, Y., Aji, Y. et al. Biomechanical impact of different isthmus positions in mandibular first molar root canals: a finite element analysis. Clin Oral Invest 28, 311 (2024). https://doi.org/10.1007/s00784-024-05715-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05715-1