Abstract
Objectives
To answer the following research question: does the clinical evaluation of restorations on permanent teeth with bioactive materials show greater retention rates than those with non-bioactive materials?
Materials and methods
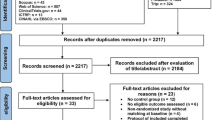
A search strategy was used in the following databases: MEDLINE via PubMed, Scopus, Web of Science, LILACS, BBO, Embase, The Cochrane Library, and OpenGrey. Randomized controlled trials (RCTs), with a minimum of 2-year follow-up and evaluating at least one bioactive material in permanent teeth were included. Risk of bias was detected according to the Cochrane Collaboration tool for assessing the risk of bias (RoB 2.0), and network meta-analysis was performed using a random-effects Bayesian-mixed treatment comparison model.
Results
Twenty-seven studies were included. The success of the restorations was assessed using modified USPHS system in 24 studies and the FDI criteria in 3 studies. Network meta-analysis revealed three networks based on restoration preparations. Resin composites were ranked with higher SUCRA values, indicating a greater likelihood of being the preferred treatment for class I, II, and III restorations. In class V, resin-modified glass ionomer cement was ranked with the highest value.
Conclusion
Bioactive restorative materials showed similar good clinical performance in terms of retention similarly to conventional resin composites.
Clinical significance
The findings must be interpreted with caution because many RCT on restorative materials aim to verify the equivalence of new materials over the gold standard material rather than their superiority. The present systematic review also suggests that new RCT with longer follow-up periods are necessary.









Similar content being viewed by others
References
Choi JE, Lyons KM, Kieser JA, Waddell NJ (2017) Diurnal variation of intraoral pH and temperature. BDJ Open 3. https://doi.org/10.1038/BDJOPEN.2017.15
Choi JE, Waddell JN, Lyons KM, Kieser JA (2016) Intraoral pH and temperature during sleep with and without mouth breathing. J Oral Rehabil 43:356–363. https://doi.org/10.1111/JOOR.12372
Demarco FF, Corrêa MB, Cenci MS, Moraes RR, Opdam NJM (2012) Longevity of posterior composite restorations: not only a matter of materials. Dent Mater 28:87–101. https://doi.org/10.1016/J.DENTAL.2011.09.003
Manhart J, García-Godoy F, Hickel R (2002) Direct posterior restorations: clinical results and new developments. Dent Clin North Am 46:303–339. https://doi.org/10.1016/S0011-8532(01)00010-6
Xu HH, Weir MD, Sun L, Moreau JL, Takagi S, Chow LC, Antonucci JM (2010) Strong nanocomposites with Ca, PO(4), and F release for caries inhibition. J Dent Res 89:19–28. https://doi.org/10.1177/0022034509351969
Mehdawi IM, Pratten J, Spratt DA, Knowles JC, Young AM (2013) High strength re-mineralizing, antibacterial dental composites with reactive calcium phosphates. Dent Mater 29:473–484. https://doi.org/10.1016/j.dental.2013.01.010
Turrer CL, Ferreira FPM (2008) Biomateriais em Cirurgia Craniomaxilofacial: princípios básicos e aplicações - revisão de literatura. Rev Bras Cir Plást 23(3):234–239
Whitlow J, Paul A, Polini A (2016) Bioactive materials: definitions and application in tissue engineering and regeneration therapy. In: Marchi J (ed) Biocompatible Glasses: From Bone Regeneration to Cancer Treatment. Springer International Publishing, Cham, pp 1–17
Pereira APV, Oréfice RL, WLV Novos biomateriais: híbridos orgânico-inorgânicos bioativos. Polímeros 9:104–109. https://doi.org/10.1590/S0104-14281999000400018
Liang K, Wang S, Tao S, Xiao S, Zhou H, Wang P, Cheng L, Zhou X, Weir MD, Oates TW, Li J, Xu HHK (2019) Dental remineralization via poly(amido amine) and restorative materials containing calcium phosphate nanoparticles. Int J Oral Sci 11:15. https://doi.org/10.1038/s41368-019-0048-z
Deligeorgi V, Mjör IA, Wilson NH (2001) An overview of reasons for the placement and replacement of restorations. Prim Dent Care 8:5–11. https://doi.org/10.1308/135576101771799335
Mjör IA, Moorhead JE, Dahl JE (2000) Reasons for replacement of restorations in permanent teeth in general dental practice. Int Dent J 50:361–366. https://doi.org/10.1111/j.1875-595x.2000.tb00569.x
Franco EB, Pascotto RC (1990) Motives for placement and replacement of dental restoration. Rev Odontol Univ Sao Paulo 4:234–240
Hicks J, Garcia-Godoy F, Donly K, Flaitz C (2003) Fluoride-releasing restorative materials and secondary caries. J Calif Dent Assoc 31:229–245
Goldstein GR (2010) The longevity of direct and indirect posterior restorations is uncertain and may be affected by a number of dentist-, patient-, and material-related factors. J Evidence Based Dental Pract 10:30–31. https://doi.org/10.1016/j.jebdp.2009.11.015
Park EY, Kang S (2020) Current aspects and prospects of glass ionomer cements for clinical dentistry. Yeungnam Univ J Med 37:169–178. https://doi.org/10.12701/yujm.2020.00374
Abdel-karim UM, El-Eraky M, Etman WM (2014) Three-year clinical evaluation of two nano-hybrid giomer restorative composites. Tanta Dental J 11:213–222. https://doi.org/10.1016/j.tdj.2014.10.004
Itota T, Carrick TE, Yoshiyama M, McCabe JF (2004) Fluoride release and recharge in giomer, compomer and resin composite. Dent Mater 20:789–795. https://doi.org/10.1016/j.dental.2003.11.009
Rusnac ME, Gasparik C, Irimie AI, Grecu AG, Mesaroş AŞ, Dudea D (2019) Giomers in dentistry – at the boundary between dental composites and glass-ionomers. Med Pharm Rep 92:123. https://doi.org/10.15386/MPR-1169
Helfer AR, Melnick S, Schilder H (1972) Determination of the moisture content of vital and pulpless teeth. Oral Surg Oral Med Oral Pathol 34:661–670. https://doi.org/10.1016/0030-4220(72)90351-9
Opdam NJ, van de Sande FH, Bronkhorst E, Cenci MS, Bottenberg P, Pallesen U, Gaengler P, Lindberg A, Huysmans MC, van Dijken JW (2014) Longevity of posterior composite restorations: a systematic review and meta-analysis. J Dent Res 93:943–949. https://doi.org/10.1177/0022034514544217
Delaviz Y, Finer Y, Santerre JP (2014) Biodegradation of resin composites and adhesives by oral bacteria and saliva: a rationale for new material designs that consider the clinical environment and treatment challenges. Dent Mater 30:16–32. https://doi.org/10.1016/j.dental.2013.08.201
Ástvaldsdóttir Á, Dagerhamn J, Van Dijken JWV, Naimi-Akbar A, Sandborgh-Englund G, Tranæus S, Nilsson M (2015) Longevity of posterior resin composite restorations in adults – A systematic review. J Dent 43:934–954. https://doi.org/10.1016/J.JDENT.2015.05.001
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JPA, Straus S, Thorlund K, Jansen JP, Mulrow C, Catala-Lopez F, Gotzsche PC, Dickersin K, Boutron I, Altman DG, Moher D (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162:777–784. https://doi.org/10.7326/M14-2385
Cochrane Handbook for Systematic Reviews of Interventions | Cochrane Training. https://training.cochrane.org/handbook. Accessed 14 Apr 2023
Rayyan - AI Powered Tool for Systematic Literature Reviews. https://www.rayyan.ai/. Accessed 14 Apr 2023
van Valkenhoef G, Lu G, de Brock B, Hillege H, Ades AE, Welton NJ (2012) Automating network meta-analysis. Res Synth. Methods 3:285–299. https://doi.org/10.1002/jrsm.1054
Heintze SD, Rousson V (2012) Clinical effectiveness of direct class II restorations - a meta-analysis. J Adhes Dent 14:407–431. https://doi.org/10.3290/j.jad.a28390
Salanti G, Higgins JP, Ades AE, Ioannidis JP (2008) Evaluation of networks of randomized trials. Stat Methods Med Res 17:279–301. https://doi.org/10.1177/0962280207080643
(2008) Methods guide for effectiveness and comparative effectiveness reviews [Internet]. Agency for Healthcare Research and Quality (US), Rockville (MD)
Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades AE (2013) Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Med Decis Making 33:641–656. https://doi.org/10.1177/0272989x12455847
Dias S, Welton NJ, Caldwell DM, Ades AE (2010) Checking consistency in mixed treatment comparison meta-analysis. Stat Med 29:932–944. https://doi.org/10.1002/SIM.3767
Salanti G, Ades AE, Ioannidis JP (2011) Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 64:163–171. https://doi.org/10.1016/j.jclinepi.2010.03.016
Puhan MA, Schünemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, Kessels AG, Guyatt GH (2014) A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ 349. https://doi.org/10.1136/BMJ.G5630
Miletić I, Baraba A, Basso M, Pulcini MG, Marković D, Perić T, Ozkaya CA, Turkun LS (2020) Clinical performance of a glass-hybrid system compared with a resin composite in the posterior region: results of a 2-year multicenter study. J Adhes Dent 22:235–247. https://doi.org/10.3290/j.jad.a44547
Mandari GJ, Frencken JE, van’t Hof MA (2003) Six-year success rates of occlusal amalgam and glass-ionomer restorations placed using three minimal intervention approaches. Caries Res 37:246–253. https://doi.org/10.1159/000070866
Wucher M, Grobler SR, Senekal PJ (2002) A 3-year clinical evaluation of a compomer, a composite and a compomer/composite (sandwich) in class II restorations. Am J Dent 15:274–278
Gurgan S, Kutuk ZB, Yalcin Cakir F, Ergin E (2020) A randomized controlled 10 years follow up of a glass ionomer restorative material in class I and class II cavities. J Dent 94:103175. https://doi.org/10.1016/j.jdent.2019.07.013
Mu HL, Tian FC, Wang XY, Gao XJ (2020) Evaluation of wear property of Giomer and universal composite in vivo. Beijing da xue xue bao Yi xue ban = J Pek Univ Health Sci 53:120–125. https://doi.org/10.19723/J.ISSN.1671-167X.2021.01.018
Gurgan S, Kutuk ZB, Ozturk C, Soleimani R, Cakir FY (2020) Clinical performance of a glass hybrid restorative in extended size class II cavities. Oper Dent 45:243–254. https://doi.org/10.2341/18-282-c
Demirci M, Yildiz E, Uysal O (2008) Comparative clinical evaluation of different treatment approaches using a microfilled resin composite and a compomer in class III cavities: two-year results. Oper Dent 33:7–14. https://doi.org/10.2341/07-34
van Dijken JW (2001) Durability of new restorative materials in class III cavities. J Adhes Dent 3:65–70
Brackett WW, Dib A, Brackett MG, Reyes AA, Estrada BE (2003) Two-year clinical performance of class V resin-modified glass-lonomer and resin composite restorations. Oper Dent 28:477–481
Burgess JO, Gallo JR, Ripps AH, Walker RS, Ireland EJ (2004) Clinical evaluation of four class 5 restorative materials: 3-year recall. Am J Dent 17:147–150
Çelik EU, Tunac AT, Yilmaz F (2018) A randomized, controlled, split-mouth trial evaluating the clinical performance of high-viscosity glass-ionomer restorations in noncarious cervical lesions: two-year results. J Adhes Dent 20:299–305. https://doi.org/10.3290/J.JAD.A40985
Fagundes TC, Barata TJ, Bresciani E, Santiago S, Franco EB, Lauris JR, Navarro MF (2014) Seven-year clinical performance of resin composite versus resin-modified glass ionomer restorations in noncarious cervical lesions. Oper Dent 39:578–587. https://doi.org/10.2341/13-054-c
Folwaczny M, Loher C, Mehl A, Kunzelmann KH, Hickel R (2001) Class V lesions restored with four different tooth-colored materials–3-year results. Clin Oral Investig 5:31–39. https://doi.org/10.1007/s007840000098
Franco EB, Benetti AR, Ishikiriama SK, Santiago SL, Lauris JR, Jorge MF, Navarro MF (2006) 5-year clinical performance of resin composite versus resin modified glass ionomer restorative system in non-carious cervical lesions. Oper Dent 31:403–408. https://doi.org/10.2341/05-87
Gallo JR, Burgess JO, Ripps AH, Walker RS, Ireland EJ, Mercante DE, Davidson JM (2005) Three-year clinical evaluation of a compomer and a resin composite as Class V filling materials. Oper Dent 30:275–281
Hatirli H, Yasa B, Çelik EU (2021) Clinical performance of high-viscosity glass ionomer and resin composite on minimally invasive occlusal restorations performed without rubber-dam isolation: a two-year randomised split-mouth study. Clin Oral Investig 25:5493–5503. https://doi.org/10.1007/s00784-021-03857-0
Kaurich M, Kawakami K, Perez P, Munn T, Hasse AL, Garrett NR (1991) A clinical comparison of a glass ionomer cement and a microfilled composite resin in restoring root caries: two-year results. Gen Dent 39:346–349
Koc Vural U, Meral E, Ergin E, Gürgan S (2020) Twenty-four-month clinical performance of a glass hybrid restorative in non-carious cervical lesions of patients with bruxism: a split-mouth, randomized clinical trial. Clin Oral Investig 24:1229–1238. https://doi.org/10.1007/S00784-019-02986-X
Levy SM, Jensen ME (1990) A clinical evaluation of the restoration of root surface caries. Spec Care Dentist 10:156–160. https://doi.org/10.1111/j.1754-4505.1990.tb00784.x
Matis BA, Cochran MJ, Carlson TJ, Guba C, Eckert GJ (2004) A three-year clinical evaluation of two dentin bonding agents. J Am Dent Assoc 135:451–457. https://doi.org/10.14219/jada.archive.2004.0209
Onal B, Pamir T (2005) The two-year clinical performance of esthetic restorative materials in noncarious cervical lesions. J Am Dent Assoc 136:1547–1555. https://doi.org/10.14219/jada.archive.2005.0085
Ozgünaltay G, Onen A (2002) Three-year clinical evaluation of a resin modified glass-ionomer cement and a composite resin in non-carious class V lesions. J Oral Rehabil 29:1037–1041. https://doi.org/10.1046/j.1365-2842.2002.00995.x
Pollington S, van Noort R (2008) A clinical evaluation of a resin composite and a compomer in non-carious Class V lesions. A 3-year follow-up. Am J Dent 21:49–52
Powell LV, Gordon GE, Johnson GH (1992) Clinical comparison of Class V resin composite and glass ionomer restorations. Am J Dent 5:249–252
Santiago SL, Passos VF, Vieira AHM, de L Navarro MF, Lauris JRP, Franco EB (2010) Two-year clinical evaluation of resinous restorative systems in non-carious cervical lesions. Braz Dent J 21:229–234. https://doi.org/10.1590/S0103-64402010000300010
Stojanac IL, Premovic MT, Ramic BD, Drobac MR, Stojsin IM, Petrovic LM (2013) Noncarious cervical lesions restored with three different tooth-colored materials: two-year results. Oper Dent 38:12–20. https://doi.org/10.2341/12-046-c
Türkün LS, Celik EU (2008) Noncarious class V lesions restored with a polyacid modified resin composite and a nanocomposite: a two-year clinical trial. J Adhes Dent 10:399–405
Cope S, Jansen JP (2013) Quantitative summaries of treatment effect estimates obtained with network meta-analysis of survival curves to inform decision-making. BMC Med Res Methodol 13. https://doi.org/10.1186/1471-2288-13-147
Mbuagbaw L, Rochwerg B, Jaeschke R, Heels-Andsell D, Alhazzani W, Thabane L, Guyatt GH (2017) Approaches to interpreting and choosing the best treatments in network meta-analyses. Syst Rev 6:1–5. https://doi.org/10.1186/S13643-017-0473-Z/FIGURES/2
Blatz MB (2021) Adhesive dentistry: just bond it! Compend Contin Educ Dent 42:536–537
Pazinatto FB, Gionordoli Neto R, Wang L, Mondelli J, Mondelli RF, Navarro MF (2012) 56-month clinical performance of class I and II resin composite restorations. J Appl Oral Sci 20:323–328. https://doi.org/10.1590/s1678-77572012000300005
Loguercio AD, Rezende M, Gutierrez MF, Costa TF, Armas-Vega A, Reis A (2019) Randomized 36-month follow-up of posterior bulk-filled resin composite restorations. J Dent 85:93–102. https://doi.org/10.1016/j.jdent.2019.05.018
Falacho RI, Melo EA, Marques JA, Ramos JC, Guerra F, Blatz MB (2022) Clinical evaluation of the effect of rubber dam isolation on bond strength to enamel. J Esthet Restor Dent. https://doi.org/10.1111/jerd.12979
Gaengler P, Hoyer I, Montag R (2001) Clinical evaluation of posterior composite restorations: the 10-year report. J Adhes Dent 3:185–194
Hellyer P (2022) The longevity of composite restorations. Br Dent J 232:459. https://doi.org/10.1038/s41415-022-4163-4
Dačić S, Miljković M, Mitić A, Radenković G, Anđelković-Apostolović M, Jovanović M (2021) Influence of etching mode and composite resin type on bond strength to dentin using universal adhesive system. Microsc Res Tech 84:1212–1219. https://doi.org/10.1002/jemt.23680
Da Rosa Rodolpho PA, Rodolfo B, Collares K, Correa MB, Demarco FF, Opdam NJM, Cenci MS, Moraes RR (2022) Clinical performance of posterior resin composite restorations after up to 33 years. Dent Mater 38:680–688. https://doi.org/10.1016/J.DENTAL.2022.02.009
Neto CCL, das Neves AM, Arantes DC, Sa TCM, Yamauti M, de Magalhães CS, Abreu LG, Moreira AN (2022) Evaluation of the clinical performance of GIOMERs and comparison with other conventional restorative materials in permanent teeth: a systematic review and meta-analysis. Evid Based Dent. https://doi.org/10.1038/s41432-022-0281-8
Gordan VV, Mondragon E, Watson RE, Garvan C, Mjör IA (2007) A clinical evaluation of a self-etching primer and a giomer restorative material: results at eight years. J Am Dent Assoc 138:621–627. https://doi.org/10.14219/jada.archive.2007.0233
Gordan VV, Blaser PK, Watson RE, Mjör IA, McEdward DL, Sensi LG, Riley JL (2014) A clinical evaluation of a giomer restorative system containing surface prereacted glass ionomer filler: results from a 13-year recall examination. J Am Dent Assoc 145:1036–1043. https://doi.org/10.14219/JADA.2014.57
Toz-Akalin T, Öztürk-Bozkurt F, Kusdemir M, Özsoy A, Yüzbaşıoğlu E, Özcan M (2023) Clinical evaluation of low-shrinkage bioactive material giomer versus nanohybrid resin composite restorations: a two-year prospective controlled clinical trial. Oper Dent 48:10–20. https://doi.org/10.2341/21-155-C
De Castro Kruly P, Giannini M, Pascotto RC, Tokubo LM, Suga USG, De Castro Ruiz Marques A, Terada RSS (2018) Meta-analysis of the clinical behavior of posterior direct resin restorations: low polymerization shrinkage resin in comparison to methacrylate composite resin. PLoS One 13. https://doi.org/10.1371/JOURNAL.PONE.0191942
Wilson MA, Cowan AJ, Randall RC, Crisp RJ, Wilson NHF (2002) A practice-based, randomized, controlled clinical trial of a new resin composite restorative: one-year results. Oper Dent 27:423–429
Moraschini V, Fai CK, Alto RM, Dos Santos GO (2015) Amalgam and resin composite longevity of posterior restorations: a systematic review and meta-analysis. J Dent 43:1043–1050. https://doi.org/10.1016/j.jdent.2015.06.005
Opdam NJ, Bronkhorst EM, Roeters JM, Loomans BA (2007) A retrospective clinical study on longevity of posterior composite and amalgam restorations. Dent Mater 23:2–8. https://doi.org/10.1016/j.dental.2005.11.036
Opdam NJ, Bronkhorst EM, Loomans BA, Huysmans MC (2010) 12-year survival of composite vs. amalgam restorations. J Dent Res 89:1063–1067. https://doi.org/10.1177/0022034510376071
Worthington HV, Khangura S, Seal K, Mierzwinski-Urban M, Veitz-Keenan A, Sahrmann P, Schmidlin PR, Davis D, Iheozor-Ejiofor Z, Rasines Alcaraz MG (2021) Direct composite resin fillings versus amalgam fillings for permanent posterior teeth. Cochrane Database Syst Rev 8:Cd005620. https://doi.org/10.1002/14651858.CD005620.pub3
Balaji S (2019) Mercury, dentistry, minamata convention and research opportunities. Indian J Dent Res 30:819. https://doi.org/10.4103/IJDR.IJDR_924_19
Jingarwar MM, Bajwa NK, Pathak A (2014) Minimal intervention dentistry – a new frontier in clinical dentistry. J Clin Diagn Res 8:ZE04. https://doi.org/10.7860/JCDR/2014/9128.4583
Wilson N, Lynch C (2013) Amalgam and minimal intervention: an incompatible relationship. Prim Dent J 2:18
Tibau AV, Grube BD (2019) Mercury contamination from dental amalgam. J Health Pollut 9:190612. https://doi.org/10.5696/2156-9614-9.22.190612
Frankenberger R, Garcia-Godoy F, Kramer N (2009) Clinical performance of viscous glass ionomer cement in posterior cavities over two years. Int J Dent 2009:781462. https://doi.org/10.1155/2009/781462
Sidhu SK (2011) Glass-ionomer cement restorative materials: a sticky subject? Aust Dent J 56(Suppl 1):23–30. https://doi.org/10.1111/j.1834-7819.2010.01293.x
Burke FJ (2013) Dental materials–what goes where? The current status of glass ionomer as a material for loadbearing restorations in posterior teeth. Dent Update 40:840–844. https://doi.org/10.12968/denu.2013.40.10.840
de Lima Navarro MF, Pascotto RC, Borges AFS, Soares CJ, Raggio DP, Rios D, Bresciani E, Molina GF, Ngo HC, Miletić I, Frencken J, Wang L, Menezes-Silva R, Puppin-Rontani RM, de Carvalho RM, Gurgan S, Leal SC, Tüzüner T, Fagundes TC, Nicholson JW, Sidhu SK (2021) Consensus on glass-ionomer cement thresholds for restorative indications. J Dent 107:103609. https://doi.org/10.1016/J.JDENT.2021.103609
Xie D, Brantley WA, Culbertson BM, Wang G (2000) Mechanical properties and microstructures of glass-ionomer cements. Dent Mater 16:129–138. https://doi.org/10.1016/S0109-5641(99)00093-7
Musanje L, Shu M, Darvell BW (2001) Water sorption and mechanical behaviour of cosmetic direct restorative materials in artificial saliva. Dent Mater 17:394–401. https://doi.org/10.1016/s0109-5641(00)00097-x
Yap AU, Chung SM, Rong Y, Tsai KT (2004) Effects of aging on mechanical properties of composite restoratives: a depth-sensing microindentation approach. Oper Dent 29:547–553
Ilie N, Hickel R (2009) Investigations on mechanical behaviour of dental composites. Clin Oral Investig 13:427–438. https://doi.org/10.1007/s00784-009-0258-4
Nicholson JW, Gjorgievska E, Bajraktarova B, McKenzie MA (2003) Changes in properties of polyacid-modified composite resins (compomers) following storage in acidic solutions. J Oral Rehabil 30:601–607. https://doi.org/10.1046/j.1365-2842.2003.01041.x
Demarco FF, Collares K, Coelho-de-Souza FH, Correa MB, Cenci MS, Moraes RR, Opdam NJ (2015) Anterior composite restorations: a systematic review on long-term survival and reasons for failure. Dent Mater 31:1214–1224. https://doi.org/10.1016/j.dental.2015.07.005
Shah YR, Shiraguppi VL, Deosarkar BA, Shelke UR (2021) Long-term survival and reasons for failure in direct anterior composite restorations: a systematic review. J Conserv Dent 24:415–420. https://doi.org/10.4103/jcd.jcd_527_21
Cargnin LL (2002) A Utilização das Resinas Compostas Modificadas por Poliácidos (compômeros) em Odontopediatria. Biblioteca Setorial de odontologia da UFSC
van Dijken JW (1996) 3-year clinical evaluation of a compomer, a resin-modified glass ionomer and a resin composite in Class III restorations. Am J Dent 9:195–198
Mohan Das U, Viswanath D, Azher U (2009) Clinical evaluation of resin composite and resin modified glass ionomer in class III restorations of primary maxillary incisors: a comparative in vivo study. Int J Clin Pediatr Dent 2:13–19. https://doi.org/10.5005/jp-journals-10005-1024
Perez CDR, Gonzalez MR, Prado NAS, De Miranda MSF, MacÊdo MDA, Fernandes BMP (2012) Restoration of noncarious cervical lesions: when, why, and how. Int J Dent 2012. https://doi.org/10.1155/2012/687058
Perez CR (2010) Alternative technique for class V resin composite restorations with minimum finishing/polishing procedures. Oper Dent 35:375–379. https://doi.org/10.2341/09-310-TR
Heintze SD, Ruffieux C, Rousson V (2010) Clinical performance of cervical restorations–a meta-analysis. Dent Mater 26:993–1000. https://doi.org/10.1016/J.DENTAL.2010.06.003
Gordan VV (2001) Clinical evaluation of replacement of class V resin based composite restorations. J Dent 29:485–488. https://doi.org/10.1016/S0300-5712(01)00030-6
Palamara JEA, Palamara D, Messer HH, Tyas MJ (2006) Tooth morphology and characteristics of non-carious cervical lesions. J Dent 34:185–194. https://doi.org/10.1016/J.JDENT.2005.05.005
Karan K, Yao X, Xu C, Wang Y (2012) Chemical characterization of etched dentin in non-carious cervical lesions. J Adhes Dent 14. https://doi.org/10.3290/J.JAD.A22766
Hoshika S, De Munck J, Sano H, Sidhu SK, Van Meerbeek B (2015) Effect of conditioning and aging on the bond strength and interfacial morphology of glass-ionomer cement bonded to dentin. J Adhes Dent 17:141–146. https://doi.org/10.3290/J.JAD.A33994
Van Dijken JWV (2005) Retention of a resin-modified glass ionomer adhesive in non-carious cervical lesions. A 6-year follow-up. J Dent 33:541–547. https://doi.org/10.1016/J.JDENT.2004.11.015
Ugurlu M (2020) Bonding of a resin-modified glass ionomer cement to dentin using universal adhesives. Restor Dent Endod 45. https://doi.org/10.5395/RDE.2020.45.E36
Saad A, Inoue G, Nikaido T, Ikeda M, Burrow MF, Tagami J (2017) Microtensile bond strength of resin-modified glass ionomer cement to sound and artificial caries–affected root dentin with different conditioning. Oper Dent 42:626–635. https://doi.org/10.2341/16-375-L
Fritz UB, Finger WJ, Uno S (1996) Resin-modified glass ionomer cements: bonding to enamel and dentin. Dent Mater 12:161–166. https://doi.org/10.1016/S0109-5641(96)80015-7
Coutinho E, Yoshida Y, Inoue S, Fukuda R, Snauwaert J, Nakayama Y, De Munck J, Lambrechts P, Suzuki K, Van Meerbeek B (2007) Gel phase formation at resin-modified glass-ionomer/tooth interfaces. J Dent Res 86:656–661. https://doi.org/10.1177/154405910708600714
Cardoso MV, Delmé KIM, Mine A, Neves ADA, Coutinho E, De Moor RJG, Van Meerbeek B (2010) Towards a better understanding of the adhesion mechanism of resin-modified glass-ionomers by bonding to differently prepared dentin. J Dent 38:921–929. https://doi.org/10.1016/J.JDENT.2010.08.009
Tay FR, Pashley DH (2004) Resin bonding to cervical sclerotic dentin: a review. J Dent 32:173–196. https://doi.org/10.1016/j.jdent.2003.10.009
Van Meerbeek B, Braem M, Lambrechts P, Vanherle G (1994) Morphological characterization of the interface between resin and sclerotic dentine. J Dent 22:141–146. https://doi.org/10.1016/0300-5712(94)90197-X
Van Dijken JWV (2000) Clinical evaluation of three adhesive systems in class V non-carious lesions. Dent Mater 16:285–291. https://doi.org/10.1016/S0109-5641(00)00019-1
van Dijken JWV (2004) Durability of three simplified adhesive systems in Class V non-carious cervical dentin lesions. Am J Dent 17:27–32
Perdigão J (2010) Dentin bonding-variables related to the clinical situation and the substrate treatment. Dent Mater 26. https://doi.org/10.1016/J.DENTAL.2009.11.149
Ozer F, Sengun A, Ozturk B, Say EC, Tagami J (2005) Effect of tooth age on microtensile bond strength of two fluoride-releasing bonding agents. J Adhes Dent 7:289–295
Karakaya S, Unlu N, Say EC, Özer F, Soyman M, Tagami J (2008) Bond strengths of three different dentin adhesive systems to sclerotic dentin. Dent Mater J 27:471–479. https://doi.org/10.4012/DMJ.27.471
Burrow MF, Tyas MJ (2012) Comparison of two all-in-one adhesives bonded to non-carious cervical lesions–results at 3 years. Clin Oral Investig 16:1089–1094. https://doi.org/10.1007/S00784-011-0595-Y
van Dijken JW (2001) Clinical effectiveness of 12 adhesive systems in class V non-retentive lesions: a 5-year evaluation (abstract 42). J Dent Res 80:1272
Momoi Y, Hirosaki K, Kohno A, McCabe JF (1995) Flexural properties of resin-modified “hybrid” glass-ionomers in comparison with conventional acid-base glass-ionomers. Dent Mater J 14:109–119. https://doi.org/10.4012/dmj.14.109
Khoroushi M, Keshani F (2013) A review of glass-ionomers: from conventional glass-ionomer to bioactive glass-ionomer. Dent Res J (Isfahan) 10:411–420
Sidhu SK, Watson TF (1995) Resin-modified glass ionomer materials. A status report for the American Journal of Dentistry. Am J Dent 8:59–67
Shen C, Grimaudo N (1994) Effect of hydration on the biaxial flexural strength of a glass ionomer cement. Dent Mater 10:190–195. https://doi.org/10.1016/0109-5641(94)90031-0
Gladys S, Van Meerbeek B, Braem M, Lambrechts P, Vanherle G (1997) Comparative physico-mechanical characterization of new hybrid restorative materials with conventional glass-ionomer and resin composite restorative materials. J Dent Res 76:883–894. https://doi.org/10.1177/00220345970760041001
Poggio C, Beltrami R, Scribante A, Colombo M, Lombardini M (2014) Effects of dentin surface treatments on shear bond strength of glass-ionomer cements. Ann Stomatol (Roma) 5:15–22
Nakanuma K, Hayakawa T, Tomita T, Yamazaki M (1998) Effect of the application of dentin primers and a dentin bonding agent on the adhesion between the resin-modified glass-ionomer cement and dentin. Dent Mater 14:281–286. https://doi.org/10.1016/S0109-5641(98)00040-2
Yap AUJ, Mok BYY (2002) Surface finish of a new hybrid aesthetic restorative material. Oper Dent 27:161–166
Koupis NS, Marks LA, Verbeeck RM, Martens LC (2007) Review: finishing and polishing procedures of (resin-modified) glass ionomers and compomers in paediatric dentistry. Eur Arch Paediatr Dent 8:22–28. https://doi.org/10.1007/BF03262566
Tarasingh P, Sharada Reddy J, Suhasini K, Hemachandrika I (2015) Comparative evaluation of antimicrobial efficacy of resin-modified glass ionomers, compomers and giomers – an invitro study. J Clin Diagn Res 9:CZ85. https://doi.org/10.7860/JCDR/2015/14364.6237
Swift EJ, Pawlus MA, Vargas MA (1995) Shear bond strengths of resin-modified glass-ionomer restorative materials. Oper Dent 20:138–143
Nicholson JW, Croll TP (1997) Glass-ionomer cements in restorative dentistry. Quintessence Int 28:705–714
Sidhu SK (2010) Clinical evaluations of resin-modified glass-ionomer restorations. Dent Mater 26:7–12. https://doi.org/10.1016/J.DENTAL.2009.08.015
Folwaczny M, Loher C, Mehl A, Kunzelmann KH, Hinkel R (2000) Tooth-colored filling materials for the restoration of cervical lesions: a 24-month follow-up study. Oper Dent 25:251–258
van Dijken JWV, Pallesen U (2008) Long-term dentin retention of etch-and-rinse and self-etch adhesives and a resin-modified glass ionomer cement in non-carious cervical lesions. Dent Mater 24:915–922. https://doi.org/10.1016/J.DENTAL.2007.11.008
Peumans M, Kanumilli P, De Munck J, Van Landuyt K, Lambrechts P, Van Meerbeek B (2005) Clinical effectiveness of contemporary adhesives: a systematic review of current clinical trials. Dent Mater 21:864–881. https://doi.org/10.1016/J.DENTAL.2005.02.003
Tyas MJ (1995) The Class V lesion–aetiology and restoration. Aust Dent J 40:167–170. https://doi.org/10.1111/J.1834-7819.1995.TB05631.X
Boing TF, de Geus JL, Wambier LM, Loguercio AD, Reis A, Gomes OMM (2018) Are glass-ionomer cement restorations in cervical lesions more long-lasting than resin-based composite resins? A systematic review and meta-analysis. J Adhes Dent 20. https://doi.org/10.3290/J.JAD.A41310
Peumans M, Politano G, Van Meerbeek B (2020) Treatment of noncarious cervical lesions: when, why, and how. Int J Esthet Dent 15:16–42
Wilson NHF, Gordan VV, Brunton PA, Wilson MA, Crisp RJ, Mjör IA (2006) Two-centre evaluation of a resin composite/ self-etching restorative system: three-year findings. J Adhes Dent 8:47–51
Sunico MC, Shinkai K, Katoh Y (2005) Two-year clinical performance of occlusal and cervical giomer restorations. Oper Dent 30:282–289
Brackett WW, Gunnin TD, Gilpatrick RO, Browning WD (1998) Microleakage of Class V compomer and light-cured glass ionomer restorations. J Prosthet Dent 79:261–263. https://doi.org/10.1016/S0022-3913(98)70234-3
Toledano M, Osorio E, Osorio R, García-Godoy F (1999) Microleakage of class V resin-modified glass ionomer and compomer restorations. J Prosthet Dent 81:610–615. https://doi.org/10.1016/S0022-3913(99)70217-9
Iwami Y, Shimizu A, Hayashi M, Takeshige F, Ebisu S (2005) Three-dimensional evaluation of gap formation of cervical restorations. J Dent 33:325–333. https://doi.org/10.1016/J.JDENT.2004.10.001
Chitnis D, Dunn WJ, Gonzales DA (2006) Comparison of in-vitro bond strengths between resin-modified glass ionomer, polyacid-modified composite resin, and giomer adhesive systems. Am J Orthod Dentofacial Orthop 129:330.e11-330.e16. https://doi.org/10.1016/J.AJODO.2005.11.011
Priyadarshini BI, Jayaprakash T, Nagesh B, Sunil CR, Sujana V, Deepa VL (2017) One-year comparative evaluation of Ketac Nano with resin-modified glass ionomer cement and Giomer in noncarious cervical lesions: a randomized clinical trial. J Conserv Dent 20:204–209. https://doi.org/10.4103/0972-0707.218305
Jyothi KN, Annapurna S, Anil Kumar S, Venugopal P, Jayashankara CM (2011) Clinical evaluation of giomer- and resin-modified glass ionomer cement in class V noncarious cervical lesions: an in vivo study. J Conserv Dent 14:409. https://doi.org/10.4103/0972-0707.87214
(2007) Restoration of teeth (simple restorations) and preventative dentistry. Restorative Dent 73–87. https://doi.org/10.1016/B978-0-443-10246-2.50011-3
Donly KJ, Sasa IS (2019) Dental materials. Pediatr Dent 293–303. https://doi.org/10.1016/B978-0-323-60826-8.00021-3
Nicholson JW (2007) Polyacid-modified composite resins (. Dent Mater 23:615–622. https://doi.org/10.1016/J.DENTAL.2006.05.002
Ermiş RB (2002) Two-year clinical evaluation of four polyacid-modified resin composites and a resin-modified glass-ionomer cement in Class V lesions. Quintessence Int 33:542–548
Hussainy S, Nasim I, Thomas T, Ranjan M (2018) Clinical performance of resin-modified glass ionomer cement, flowable composite, and polyacid-modified resin composite in noncarious cervical lesions: One-year follow-up. J Conserv Dent 21:510. https://doi.org/10.4103/JCD.JCD_51_18
Chinelatti MA, Ramos RP, Chimello DT, Palma-Dibb RG (2004) Clinical performance of a resin-modified glass-ionomer and two polyacid-modified resin composites in cervical lesions restorations: 1-year follow-up. J Oral Rehabil 31:251–257. https://doi.org/10.1046/J.0305-182X.2003.01221.X
Loguercio AD, Reis A, Barbosa AN, Roulet JF (2003) Five-year double-blind randomized clinical evaluation of a resin-modified glass ionomer and a polyacid-modified resin in noncarious cervical lesions. J Adhes Dent 5:323–332
Peumans M, De Munck J, Mine A, Van Meerbeek B (2014) Clinical effectiveness of contemporary adhesives for the restoration of non-carious cervical lesions. A systematic review. Dent Mater 30:1089–1103. https://doi.org/10.1016/J.DENTAL.2014.07.007
Pecie R, Krejci I, García-Godoy F, Bortolotto T (2011) Noncarious cervical lesions (NCCL)–a clinical concept based on the literature review. Part 2: restoration. Am J Dent 24:183–192
Bollen CM, Lambrechts P, Quirynen M (1997) Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: a review of the literature. Dent Mater 13:258–269. https://doi.org/10.1016/S0109-5641(97)80038-3
Madhyastha PS, Hegde S, Srikant N, Kotian R, Iyer SS (2017) Effect of finishing/polishing techniques and time on surface roughness of esthetic restorative materials. Dent Res J (Isfahan) 14:326–330. https://doi.org/10.4103/1735-3327.215962
Özgünaltay G, Yazici AR, Görücü J (2003) Effect of finishing and polishing procedures on the surface roughness of new tooth-coloured restoratives. J Oral Rehabil 30:218–224. https://doi.org/10.1046/J.1365-2842.2003.01022.X
McKinney JE, Antonucci JM, Rupp NW (1987) Wear and microhardness of glass-ionomer cements. 66:1134–1139. https://doi.org/10.1177/00220345870660060801
Ichim IP, Schmidlin PR, Li Q, Kieser JA, Swain MV (2007) Restoration of non-carious cervical lesions Part II. Restorative material selection to minimise fracture. Dent Mater 23:1562–1569. https://doi.org/10.1016/J.DENTAL.2007.02.002
Bezerra IM, Brito ACM, de Sousa SA, Santiago BM, Cavalcanti YW, de Almeida L de FD (2020) Glass ionomer cements compared with composite resin in restoration of noncarious cervical lesions: a systematic review and meta-analysis. Heliyon 6. https://doi.org/10.1016/J.HELIYON.2020.E03969
Kampanas NS, Antoniadou M (2018) Glass ionomer cements for the restoration of non-carious cervical lesions in the geriatric patient. J Funct Biomater 9. https://doi.org/10.3390/JFB9030042
Gryst MEI, Mount GJ (1999) The use of glass ionomer in special needs patients. Aust Dent J 44:268–274. https://doi.org/10.1111/J.1834-7819.1999.TB00231.X
Naganuma Y, Takahashi M, Takada Y, Hoshi K, Kitaoka A, Takahashi A, Sasaki K (2022) Usefulness of conventional glass ionomer cements in an environment of insufficient moisture exclusion. J Oral Sci 64:242–246. https://doi.org/10.2334/JOSNUSD.22-0012
Smales RJ, Yip HK (2000) The atraumatic restorative treatment (ART) approach for primary teeth: review of literature. Pediatr Dent 22:294–298
Cefaly DFG, Tapety CMC, Mondelli RFL, Lauris JRP, Phantumvanit P, Navarro MFL (2006) Three-year evaluation of the ART approach in class III and V restorations in permanent anterior teeth. Caries Res 40:389–392. https://doi.org/10.1159/000094283
Hu JY, Chen XC, Li YQ, Smales RJ, Yip KH (2005) Radiation-induced root surface caries restored with glass-ionomer cement placed in conventional and ART cavity preparations: results at two years. Aust Dent J 50:186–190. https://doi.org/10.1111/J.1834-7819.2005.TB00359.X
Francisconi LF, Scaffa PMC, dos Santos Paes de Barros VR, Coutinho M, Francisconi PAS (2009) Glass ionomer cements and their role in the restoration of non-carious cervical lesions. J Appl Oral Sci 17:364. https://doi.org/10.1590/S1678-77572009000500003
Chan AW, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, Dickersin K, Hróbjartsson A, Schulz KF, Parulekar WR, Krleza-Jeric K, Laupacis A, Moher D (2013) SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 346. https://doi.org/10.1136/bmj.e7586
Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. BMJ 340:698–702. https://doi.org/10.1136/BMJ.C332
Funding
This study was funded by São Paulo Research Foundation (FAPESP; grants 2019/14729–9 and 2020/15561–1).
Author information
Authors and Affiliations
Contributions
Conceptualization: T.M.F.C. and E.B. Methodology: J.B.F., S.M.C. and T.M.F.C. Statistical analysis: T.M.F.C and E.B. Writing—original draft: J.B.F., S.M.C., M.S.S, G.R.B., E.B. and T.M.F.C. Reviewing the manuscript: T.M.F.C. and M.S.S.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fernandes, J.B., Contreras, S.M., da Silva Spinola, M. et al. Do bioactive materials show greater retention rates in restoring permanent teeth than non-bioactive materials? A systematic review and network meta-analysis of randomized controlled trials. Clin Oral Invest 28, 44 (2024). https://doi.org/10.1007/s00784-023-05414-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-023-05414-3