Abstract
Objectives
Periodontitis is a chronic infectious disease, which leads to inflammatory destruction of periodontal supporting tissues. Interleukin 14 (IL-14), Interleukin 16 (IL-16) and serum amyloid A (SAA) have been demonstrated to be abnormally expressed in inflammatory diseases. Therefore, this study was performed to analyzed the expression and potential clinical values of IL-14, 1L-16 and SAA in periodontitis.
Materials and methods
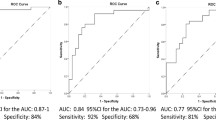
A total of 100 periodontitis patients and 100 healthy volunteers were recruited and the saliva and serum samples were collected. Then the C-reactive protein (CRP), procalcitonin (PCT), IL-14, 1L-16 and SAA levels in the saliva and serum of periodontitis patients were measured by Elisa kits. Besides, the significance of CRP, PCT, IL-14, 1L-16 and SAA in periodontitis patients were analyzed by receiver operating characteristic (ROC) analysis.
Results
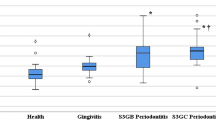
The results showed that CRP, PCT, IL-14, 1L-16 and SAA levels were significantly increased in the the saliva and serum of the periodontitis patients. Additionally, the area under the curve (AUC) of saliva CRP, PCT, IL-14, 1L-16 and SAA for the diagnosis of periodontitis were 0.9035, 0.9435, 0.9508, 0.9500 and 0.9467, respectively. The AUC of serum CRP, PCT, IL-14, 1L-16 and SAA for the diagnosis of periodontitis were 0.9035, 0.9435, 0.9508, 0.9500 and 0.9467, respectively. What’s more, the diagnostic value of IL-14, 1L-16 and SAA were enhanced when combining with CRP and PCT.
Conclusion and clinical relevance
This study demonstrated that IL-14, IL-16 and SAA expressions were upregulated in periodontitis patients and exhibited a significant significance for periodontitis diagnosis.






Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Kwon T, Lamster IB, Levin L (2021) Current concepts in the management of periodontitis. Int Dent J 71:462–476
Slots J (2017) Periodontitis: facts, fallacies and the future. Periodontology 2000 75:7–23
Taalab MR, Mahmoud SA, Moslemany R, Abdelaziz DM (2021) Intrapocket application of tea tree oil gel in the treatment of stage 2 periodontitis. BMC Oral Health 21:239
Oyaro B, Lokken E, Alumera H, Hussein S, Richardson B, Mandaliya K, Jaoko W, Kinuthia J, Dimba E, Kemoli A, McClelland RS (2022) Prevalence and correlates of periodontitis among Kenyan women planning to conceive. BMC Oral Health 22:216
Lindner M, Arefnia B, Ivastinovic D, Sourij H, Lindner E, Wimmer G (2022) Association of periodontitis and diabetic macular edema in various stages of diabetic retinopathy. Clin Oral Invest 26:505–512
Wong RL, Hiyari S, Yaghsezian A, Davar M, Lin YL, Galvan M, Tetradis S, Camargo PM, Pirih FQ (2017) Comparing the healing potential of late-stage periodontitis and peri-implantitis. J Oral Implantol 43:437–445
Bell S, Gibson JT, Harshfield EL, Markus HS (2020) Is periodontitis a risk factor for ischaemic stroke, coronary artery disease and subclinical atherosclerosis? A Mendelian randomization study. Atherosclerosis 313:111–117
Seoane T, Bullon B, Fernandez-Riejos P, Garcia-Rubira JC, Garcia-Gonzalez N, Villar-Calle P, Quiles JL, Battino M, Bullon P (2022) Periodontitis and other risk factors related to myocardial infarction and its follow-up. J Clin Med 11:2618
Yeh YT, Tseng YS, Wu YL, Yang SF, Wang BY, Wang YH, Yeh LT, Yeh YT, Chan CH (2022) Risk of peripheral arterial occlusive disease with periodontitis and dental scaling: a nationwide population-based cohort study. Int J Environ Res Public Health 19:10057
Salhi L, Rijkschroeff P, Van Hede D, Laine ML, Teughels W, Sakalihasan N, Lambert F (2021) Blood biomarkers and serologic immunological profiles related to periodontitis in abdominal aortic aneurysm patients. Front Cell Infect Microbiol 11:766462
Bengtsson VW, Persson GR, Berglund JS, Renvert S (2021) Periodontitis related to cardiovascular events and mortality: a long-time longitudinal study. Clin Oral Invest 25:4085–4095
Jaedicke KM, Preshaw PM, Taylor JJ (2016) Salivary cytokines as biomarkers of periodontal diseases. Periodontology 2000 70:164–183
Plemmenos G, Evangeliou E, Polizogopoulos N, Chalazias A, Deligianni M, Piperi C (2021) Central regulatory role of cytokines in periodontitis and targeting options. Curr Med Chem 28:3032–3058
Pan W, Wang Q, Chen Q (2019) The cytokine network involved in the host immune response to periodontitis. Int J Oral Sci 11:30
Lu H, Wu H, Yang Y, Feng X, Ma X, Xie Y, Xie D, Wang W, Lo E, Ye W (2022) Relationship between chronic periodontitis and inflammatory cytokines in patients undergoing maintenance hemodialysis. Clin Oral Invest 26:6699–6709
Zhang J, Huang X, Lu B, Zhang C, Cai Z (2016) Can apical periodontitis affect serum levels of CRP, IL-2, and IL-6 as well as induce pathological changes in remote organs? Clin Oral Invest 20:1617–1624
Zhang Y, Zhang J, Sheng H, Li H, Wang R (2019) Acute phase reactant serum amyloid A in inflammation and other diseases. Adv Clin Chem 90:25–80
Cheng N, Liang Y, Du X, Ye RD (2018) Serum amyloid A promotes LPS clearance and suppresses LPS-induced inflammation and tissue injury. EMBO Rep 19:n/a-n/a
Oertly M, Gerber V, Anhold H, Chan DS, Pusterla N (2021) The accuracy of serum Amyloid A in determining early inflammation in horses after long-distance transportation by air. J Equine Vet 97:103337
Turer CC, Balli U, Guven B (2017) Fetuin-A, serum amyloid A and tumor necrosis factor alpha levels in periodontal health and disease. Oral Dis 23:379–386
Helen Kemp E, Ajjan RA, Metcalfe RA, Watson PF, Weetman AP (2015) IL-14 and IL-16 are expressed in the thyroid of patients with either Graves’ disease or Hashimoto’s thyroiditis. Clin Endocrinol (Oxford) 83:726–732
Leca N, Laftavi M, Shen L, Matteson K, Ambrus JJ, Pankewycz O (2008) Regulation of human interleukin 14 transcription in vitro and in vivo after renal transplantation. Transplantation 86:336–341
Hayry A, Faustini F, Zickert A, Larsson A, Niewold TB, Svenungsson E, Oke V, Gunnarsson I (2022) Interleukin (IL) 16: a candidate urinary biomarker for proliferative lupus nephritis. Lupus Sci Med 9:e000744
Singh AR, Peirce SK, Joshi S, Durden DL (2014) PTEN and PI-3 kinase inhibitors control LPS signaling and the lymphoproliferative response in the CD19+ B cell compartment. Exp Cell Res 327:78–90
Cruikshank W, Little F (2008) lnterleukin-16: the ins and outs of regulating T-cell activation. Crit Rev Immunol 28:467–483
Souza VH, Visentainer J, Zacarias J, Alencar JB, Tsuneto PY, Silva CO, Salmeron S, Colli CM, Sell AM (2020) Association of IL16 polymorphisms with periodontitis in Brazilians: A case- control study. PLoS ONE 15:e239101
Sui YD, Xin WN, Feng LL (2020) Comparison of the clinical application values of PCT, hs-CRP and SAA detection in the early diagnosis of sepsis. Pak J Med Sci 36:1683–1687
Ardila CM, Guzman IC (2015) Comparison of serum amyloid A protein and C-reactive protein levels as inflammatory markers in periodontitis. J Periodontal Implant Sci 45:14–22
Caton JG, Armitage G, Berglundh T, Chapple ILC, Jepsen S, Kornman KS, Mealey BL, Papapanou PN, Sanz M, Tonetti MS (2018) A new classification scheme for periodontal and peri-implant diseases and conditions - Introduction and key changes from the 1999 classification. J Clin Periodontol 45(Suppl 20):S1–S8
Zeng J, Jia N, Ji C, Zhong S, Chai Q, Zou C, Chen L (2022) Plaque control alleviated renal damage that was aggravated by experimental periodontitis in obese rats. Oral Dis 28:1228–1239
Xu XW, Liu X, Shi C, Sun HC (2021) Roles of immune cells and mechanisms of immune responses in periodontitis. Chin J Dent Res: Off J Sci Sect Chin Stomatol Assoc (CSA) 24:219
Chen Z, Chen G (2021) Interleukin-16 rs4072111 polymorphism is associated with the risk of peri-implantitis in the Chinese population. Pharmacogenomics Pers Med 14:1629–1635
Bunte K, Beikler T (2019) Th17 cells and the IL-23/IL-17 axis in the pathogenesis of periodontitis and immune-mediated inflammatory diseases. Int J Mol Sci 20:3394
Zou S, Liu J, Yang Z, Xiao D, Cao D (2021) SAA and CRP are potential indicators in distinction and severity assessment for children with influenza. Int J Infect Dis 108:357–362
De Buck M, Gouwy M, Struyf S, Opdenakker G, Van Damme J (2019) The ectoenzyme-side of matrix metalloproteinases (MMPs) makes inflammation by serum amyloid A (SAA) and chemokines go round. Immunol Lett 205:1–8
Song LT, Lai W, Li JS, Mu YZ, Li CY, Jiang SY (2020) The interaction between serum amyloid A and Toll-like receptor 2 pathway regulates inflammatory cytokine secretion in human gingival fibroblasts. J Periodontol 91:129–137
Ambrus JJ, Contractor V, Joseph A, Long J, Blumenthal D (1995) A potential role for PGE and IL-14 (HMW-BCGF) in B-Cell hyperactivity of patients with systemic lupus erythematosus. Am J Ther 2:933–942
Glass WG, Sarisky RT, Vecchio AM (2006) Not-so-sweet sixteen: the role of IL-16 in infectious and immune-mediated inflammatory diseases. J Interferon Cytokine Res 26:511–520
Reinhold D, Guttek K, Reddig A, Voss L, Schubert C, Kahlfuss S, Grungreiff K, Schraven B, Reinhold A (2021) Zinc aspartate induces IL-16 secretion and apoptosis in human T cells. Biomedicines 9:246
Reich K, Hugo S, Middel P, Blaschke V, Heine A, Neumann C (2004) The maturation-dependent production of interleukin-16 is impaired in monocyte-derived dendritic cells from atopic dermatitis patients but is restored by inflammatory cytokines TNF-alpha and IL-1beta. Exp Dermatol 13:740–747
Vuletic S, Taylor BA, Tofler GH, Chait A, Marcovina SM, Schenck K, Albers JJ (2008) SAA and PLTP activity in plasma of periodontal patients before and after full-mouth tooth extraction. Oral Dis 14:514–519
Machado V, Botelho J, Escalda C, Hussain SB, Luthra S, Mascarenhas P, Orlandi M, Mendes JJ, D’Aiuto F (2021) Serum C-Reactive protein and periodontitis: a systematic review and meta-analysis. Front Immunol 12:706432
Murakami K, Suzuki C, Fujii A, Kobayashi F, Nakano A, Kamizono A (2014) Intravenous immunoglobulin preparation prevents the production of pro-inflammatory cytokines by modulating NFkappaB and MAPKs pathways in the human monocytic THP-1 cells stimulated with procalcitonin. Inflamm Res 63:711–718
Wen X, Han XR, Wang YJ, Fan SH, Zhang ZF, Wu DM, Lu J, Zheng YL (2018) Effects of S100A12 gene silencing on serum levels of anti-inflammatory/pro-inflammatory cytokines in septic rats through the ERK signaling pathway. J Cell Biochem 119:4038–4049
Tsai IS, Tsai CC, Ho YP, Ho KY, Wu YM, Hung CC (2005) Interleukin-12 and interleukin-16 in periodontal disease. Cytokine 31:34–40
Funding
This research was supported by Natural Science Research Project of Bengbu Medical College under grant number 2021byzd136; Natural Science Research Project of Anhui Educational Committee under grant number KJ2021A0790; Natural Science Research Project of Anhui Educational Committee under grant number 2023AH051941.
Author information
Authors and Affiliations
Contributions
All authors participated in the design, interpretation of the studies and analysis of the data and review of the manuscript. X L drafted the work and revised it critically for important intellectual content; P L, J L and J H were responsible for the acquisition, analysis, or interpretation of data for the work; R T made substantial contributions to the conception or design of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study protocol was performed in accordance with the Declaration of Helsinki and approved by the Ethics Committee of The First Affiliated Hospital of Bengbu Medical College (No. (2022)1). Informed consent was obtained from all subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lu, X., Li, P., Li, J. et al. Clinical diagnostic value of IL-14, 1L-16 and SAA in periodontitis. Clin Oral Invest 27, 6627–6635 (2023). https://doi.org/10.1007/s00784-023-05269-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05269-8