Abstract
Objectives
This study was designed to determine the optimal anterior-posterior (AP) position of upper incisors through Anterior Nasal Spine (ANS) point.
Materials and methods
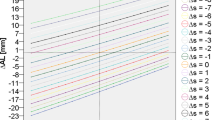
Lateral cephalometric radiographic images of 690 patients were collected and divided into a derivation group and a validation group, and the former were subdivided into a proper AP position (PAP) group and an improper AP position (iPAP) group. The distance from facia-axis (FA) point of upper incisors to the line perpendicular to Frankfort horizontal (FH) plane through ANS (FA-ANS) was measured, and the relationship between FA-ANS and several cephalometric indices were studied through Pearson correlation analysis. Receiver operating characteristic (ROC) curves for different clinical indices were analyzed to evaluate the diagnostic efficiency of optimal AP position of upper incisors.
Results
The average value of FA-ANS in PAP group was 0.57±1.99, which was significantly different from FA-ANS in iPAP group. Cephalometric indices such as U1-NA, U1-SN, AB-NPo, UL-TVL, Wits, and ANB were found to be correlated with FA-ANS. The receiver operating characteristic (ROC) curves represented a greater diagnostic efficiency of FA-ANS compared with other clinical indices.
Conclusions
ANS point, as a stable skeletal landmark, could be used to access an optimal AP position of upper incisors, providing aids to clinical diagnosis and treatment goal determination for clinical practice.
Clinical relevance
A new index FA-ANS, together with other traditional indices, could help determine the optimal position of upper incisors and provide a personalized therapeutic plan.




Similar content being viewed by others
References
He D, Gu Y, Sun Y (2019) Evaluation of aesthetic anteroposterior position of maxillary incisors in patients with extraction treatment using facial reference lines. J Int Med Res 47:2951–2960. https://doi.org/10.1177/0300060519850740
Gidaly MP, Tremont T, Lin CP, Kau CH, Souccar NM (2019) Optimal antero-posterior position of the maxillary central incisors and its relationship to the forehead in adult African American females. Angle Orthod 89:123–128. https://doi.org/10.2319/120517-833.1
Bueller H (2018) Ideal facial relationships and goals. Facial Plast Surg 34:458–465. https://doi.org/10.1055/s-0038-1669401
Hicks KE, Thomas JR (2020) The changing face of beauty: a global assessment of facial beauty. Otolaryngol Clin North Am 53:185–194. https://doi.org/10.1016/j.otc.2019.12.005
Samizadeh S, Wu W (2020) Ideals of facial beauty amongst the Chinese population: results from a large national survey. Aesthetic Plast Surg 44:1173–1183. https://doi.org/10.1007/s00266-020-01815-x
Young P (2019) Assessment of ideal dimensions of the ears, nose, and lip in the circles of prominence theory on facial beauty. JAMA. Facial Plast Surg 21:199–205. https://doi.org/10.1001/jamafacial.2018.1797
Simões D, Meyge de Brito G, Teixeira Cangussu MC, Machado AW (2019) Does the vertical position of maxillary central incisors in men influence smile esthetics perception? Am J Orthod Dentofacial Orthop 156:485–492. https://doi.org/10.1016/j.ajodo.2018.10.023
Steiner CC (1953) Cephalometrics for you and me. Am J Orthod 39:729–755. https://doi.org/10.1111/ocr.12542
Arnett GW, Bergman RT (1993) Facial keys to orthodontic diagnosis and treatment planning. Part I. Am J Orthod Dentofacial Orthop 103:299–312. https://doi.org/10.1016/0889-5406(93)70010-L
Arnett GW, Jelic JS, Kim J, Cummings DR, Beress A, Worley CM Jr, Chung B, Bergman R (1999) Soft tissue cephalometric analysis: diagnosis and treatment planning of dentofacial deformity. Am J Orthod Dentofacial Orthop 116:239–253. https://doi.org/10.1016/s0889-5406(99)70234-9
Andrews WA (2008) AP relationship of the maxillary central incisors to the forehead in adult white females. Angle Orthod 78:662–669. https://doi.org/10.2319/0003-3219(2008)078[0662:AROTMC]2.0.CO;2
Madsen DP, Sampson WJ, Townsend GC (2008) Craniofacial reference plane variation and natural head position. Eur J Orthod 30:532–540. https://doi.org/10.1093/ejo/cjn031
Carruitero MJ, Ambrosio-Vallejos XM, Flores-Mir C (2019) Glabellar vertical line as a reference goal for anteroposterior maxillary position. Dental Press. J Orthod 24:45.e1–45.e5. https://doi.org/10.1590/2177-6709.24.3.45.e1-5.onl
Imaizumi K, Taniguchi K, Ogawa Y, Matsuzaki K, Maekawa H, Nagata T, Mochimaru M, Kouchi M (2019) Three-dimensional shape variation and sexual dimorphism of the face, nose, and mouth of Japanese individuals. Forensic Sci Int 302:109878. https://doi.org/10.1016/j.forsciint.2019.109878
Kanavakis G, Silvola AS, Halazonetis D, Lähdesmäki R, Pirttiniemi P (2022) Profile shape variation and sexual dimorphism amongst middle-aged Northern Europeans. Eur J Orthod 44:30–36. https://doi.org/10.1093/ejo/cjab004
Skomina Z, Verdenik M, Hren NI (2020) Effect of aging and body characteristics on facial sexual dimorphism in the Caucasian Population. PLoS One 15:e0231983. https://doi.org/10.1371/journal.pone.0231983
Cassi D, De Biase C, Tonni I, Gandolfini M, Di Blasio A, Piancino MG (2016) Natural position of the head: review of two-dimensional and three-dimensional methods of recording. Br J Oral Maxillofac Surg 54:233–240. https://doi.org/10.1016/j.bjoms.2016.01.025
Jabbal A, Cobourne M, Donaldson N, Bister D (2016) Assessing lower incisor inclination change: a comparison of four cephalometric methods. Eur J Orthod 38:184–189. https://doi.org/10.1093/ejo/cjv027
Göstemeyer G, Preus M, Elhennawy K, Schwendicke F, Paris S, Askar H (2023) Accuracy of different approaches for detecting proximal root caries lesions in vitro. Clin Oral Investig 27:1143–1151. https://doi.org/10.1007/s00784-022-04709-1
Solem RC, Marasco R, Guiterrez-Pulido L, Nielsen I, Kim SH, Nelson G (2013) Three-dimensional soft-tissue and hard-tissue changes in the treatment of bimaxillary protrusion. Am J Orthod Dentofacial Orthop. 144:218–228. https://doi.org/10.1016/j.ajodo.2013.03.018
Resnick CM, Calabrese CE, Resnick AS (2018) Maxillary sagittal position in relation to the forehead: a target for orthognathic surgery. J Craniofac Surg 29:688–691. https://doi.org/10.1097/SCS.0000000000004267
Venkategowda PR, Prakash AT, Roy ET, Shetty KS, Thakkar S, Maurya R (2017) Stability of vertical, horizontal and angular parameters following superior repositioning of maxilla by Le Fort I osteotomy: a cephalometric study. J Clin Diagn Res 11:Zc10–Zc14. https://doi.org/10.7860/JCDR/2017/22455.9133
Barbera AL, Sampson WJ, Townsend GC (2009) An evaluation of head position and craniofacial reference line variation. Homo 60:1–28. https://doi.org/10.1016/j.jchb.2008.05.003
Jakobsone G, Vuollo V, Pirttiniemi P (2020) Reproducibility of Natural Head Position assessed with stereophotogrammetry. Orthod Craniofac Res 23:66–71. https://doi.org/10.1111/ocr.12344
Agbolade O, Nazri A, Yaakob R, Ghani AA, Cheah YK (2020) Morphometric approach to 3D soft-tissue craniofacial analysis and classification of ethnicity, sex, and age. PLoS One 15:e0228402. https://doi.org/10.1371/journal.pone.0228402
Gibelli D, Collini F, Porta D, Zago M, Dolci C, Cattaneo C, Sforza C (2016) Variations of midfacial soft-tissue thickness in subjects aged between 6 and 18 years for the reconstruction of the profile: a study on an Italian sample. Leg Med (Tokyo) 22:68–74. https://doi.org/10.1016/j.legalmed.2016.08.005
Devi SS, Dinesh S, Sivakumar A, Nivethigaa B, Alshehri A, Awadh W, Alam MK, Bhandi S, Raj AT, Patil S (2022) Reliability of Frankfort horizontal plane with true horizontal plane in cephalometric measurements. J Contemp Dent Pract 23:601–605. https://doi.org/10.5005/jp-journals-10024-3344
Nahhas RW, Valiathan M, Sherwood RJ (2014) Variation in timing, duration, intensity, and direction of adolescent growth in the mandible, maxilla, and cranial base: the Fels longitudinal study. Anat Rec (Hoboken) 297:1195–1207. https://doi.org/10.1002/ar.22918
Chen YJ, Chen SK, Chang HF, Chen KC (2000) Comparison of landmark identification in traditional versus computer-aided digital cephalometry. Angle Orthod 70:387–392. https://doi.org/10.1043/0003-3219(2000)070<0387:COLIIT>2.0.CO;2
Chien PC, Parks ET, Eraso F, Hartsfield JK, Roberts WE, Ofner S (2009) Comparison of reliability in anatomical landmark identification using two-dimensional digital cephalometrics and three-dimensional cone beam computed tomography in vivo. Dentomaxillofac Radiol 38:262–273. https://doi.org/10.1259/dmfr/81889955
Akhare PJ, Dagab AM, Alle RS, Shenoyd U, Garla V (2013) Comparison of landmark identification and linear and angular measurements in conventional and digital cephalometry. Int J Comput Dent 16:241–254
Bulatova G, Kusnoto B, Grace V, Tsay TP, Avenetti DM, Sanchez FJC (2021) Assessment of automatic cephalometric landmark identification using artificial intelligence. Orthod Craniofac Res 24:37–42. https://doi.org/10.1111/ocr.12542
Bayome M, Park JH, Kook YA (2013) New three-dimensional cephalometric analyses among adults with a skeletal Class I pattern and normal occlusion. Korean J Orthod 43:62–73. https://doi.org/10.4041/kjod.2013.43.2.62
Barros SE, Chiqueto K, Janson G, Faria J, Moraes L (2021) Effect of Class II camouflage treatment on anterior arch length ratio and canine relationship. Am J Orthod Dentofacial Orthop 159:e7–e16. https://doi.org/10.1016/j.ajodo.2020.08.007
Kim SJ, Kim KH, Yu HS, Baik HS (2014) Dentoalveolar compensation according to skeletal discrepancy and overjet in skeletal Class III patients. Am J Orthod Dentofacial Orthop 145:317–324. https://doi.org/10.1016/j.ajodo.2013.11.014
Uzuner FD, Aslan BI, Dinçer M (2019) Dentoskeletal morphology in adults with Class I, Class II Division 1, or Class II Division 2 malocclusion with increased overbite. Am J Orthod Dentofacial Orthop. 156:248–256.e2. https://doi.org/10.1016/j.ajodo.2019.03.006
Cao L, Zhang K, Bai D, Jing Y, Tian Y, Guo Y (2011) Effect of maxillary incisor labiolingual inclination and anteroposterior position on smiling profile esthetics. Angle Orthod 81:121–129. https://doi.org/10.2319/033110-181.1
Funding
This study was funded by the National Natural Science Foundation [32271364] and [31971240], Clinical Research Project of West China Hospital of Stomatology, Sichuan University [LCYJ2019-22], and Chengdu Artificial Intelligence Application Development Industrial Technology Basic Public Service Platform [2021-0166-1-2].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Research Ethics Committee of West China Hospital of Stomatology (Number: WCHSIRB-D-2021-136) and informed consent was taken from all individual participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Feng, Q., Zhou, J., Zhang, G. et al. Evaluation of optimal anterior-posterior position of upper incisors through ANS point: a retrospective study on a Chinese sample. Clin Oral Invest 27, 5947–5955 (2023). https://doi.org/10.1007/s00784-023-05208-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05208-7