Abstract
Objective
This study aimed to evaluate the long-term stability of surgical maxillary expansion using patient-specific fixation implants (PSFIs) without intraoral retention.
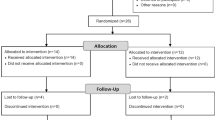
Materials and methods
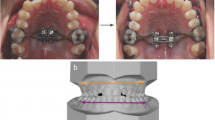
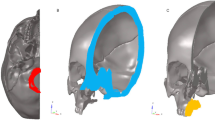
Fifteen patients who had undergone segmented Le Fort I osteotomy and PSFIs with available preoperative (t0) early (t1) and 1-year follow-up computed tomography (CT) scans (t2) were evaluated. The early and 1-year 3D models were superimposed to transfer the bony landmarks; the distances between each pair of landmarks at the different time points were then measured. The distances between the canines and second molars were also measured directly on the CT scans.
Results
The achieved maxillary expansions ranged from a median of 4.39 (2.00–6.27) mm at the greater palatine foramina to a median of 2.14 (1.56–2 > 83) mm at the canine level of the palatal bone. One year postoperatively, the changes in skeletal diameters ranged from a median of − 0.53 (− 1.65 to 0.41) mm at the greater palatine foramina (p = 0.12) to 0.17 (− 0.09 to 0.32) mm at the canine level of the palatal bone (p = 0.56). Changes in dental arch diameters ranged from a median of − 0.6 (− 2 to 0.00) mm between the second molars to − 1.3 (− 1.8 to − 0.25) mm between the canines (P < 0.05).
Conclusion
This study showed the stability of maxillary expansion osteotomy using PSFIs, even without postoperative intraoral retention.
Clinical relevance
PSFIs are a reliable method for the surgical treatment of transverse maxillary discrepancy. PFSIs are easy-to-use and improve surgical accuracy.









Similar content being viewed by others
References
McNamara JA (2000) Maxillary transverse deficiency. Am J Orthod Dentofacial Orthop 117:567–570. https://doi.org/10.1016/s0889-5406(00)70202-2
Reyneke JP, Conley RS (2020) Surgical/Orthodontic Correction of Transverse Maxillary Discrepancies. Oral Maxillofac Surg Clin North Am 32:53–69. https://doi.org/10.1016/j.coms.2019.08.007
Phillips C, Medland WH, Fields HW et al (1992) Stability of surgical maxillary expansion. Int J Adult Orthodon Orthognath Surg 7:139–146
Haas Junior OL, Guijarro-Martínez R, de Sousa Gil AP et al (2019) Hierarchy of surgical stability in orthognathic surgery: overview of systematic reviews. Int J Oral Maxillofac Surg 48:1415–1433. https://doi.org/10.1016/j.ijom.2019.03.003
Proffit WR, Turvey TA, Phillips C (1996) Orthognathic surgery: a hierarchy of stability. Int J Adult Orthodon Orthognath Surg 11:191–204
Yao W, Bekmezian S, Hardy D et al (2015) Cone-beam computed tomographic comparison of surgically assisted rapid palatal expansion and multipiece Le Fort I osteotomy. J Oral Maxillofac Surg 73:499–508. https://doi.org/10.1016/j.joms.2014.08.024
Marchetti C, Pironi M, Bianchi A, Musci A (2009) Surgically assisted rapid palatal expansion vs. segmental Le Fort I osteotomy: transverse stability over a 2-year period. J Craniomaxillofac Surg 37:74–78. https://doi.org/10.1016/j.jcms.2008.08.006
Alcalde RE, Bloomquist DS, Joondeph D (2012) Chapter 77 - Maxillary Deficiency: Transverse Plane Discrepancies. In: Bagheri SC, Bell RB, Khan HA (eds) Current Therapy In Oral and Maxillofacial Surgery. W.B. Saunders, Saint Louis, p 640–650
Seeberger R, Gander E, Hoffmann J, Engel M (2015) Surgical management of cross-bites in orthognathic surgery: Surgically assisted rapid maxillary expansion (SARME) versus two-piece maxilla. J Craniomaxillofac Surg 43:1109–1112. https://doi.org/10.1016/j.jcms.2015.05.012
Ismail M, Wessel J, Farrell B (2019) Maintenance of Segmental Maxillary Expansion: The Use of Custom, Virtually Designed, and Manufactured Palatal Appliances Without the Use of an Occlusal Splint. J Oral Maxillofac Surg 77:1468.e1-1468.e8. https://doi.org/10.1016/j.joms.2019.03.013
Huang GJ, Justus R, Kennedy DB, Kokich VG (1990) Stability of anterior openbite treated with crib therapy. Angle Orthod 60:17–24. https://doi.org/10.1043/0003-3219(1990)060%3c0017:SOAOTW%3e2.0.CO;2. (discussion 25-26)
Seemann J, Kundt G, Stahl de Castrillon F (2011) Relationship between occlusal findings and orofacial myofunctional status in primary and mixed dentition: part IV: interrelation between space conditions and orofacial dysfunctions. J Orofac Orthop 72:21–32. https://doi.org/10.1007/s00056-010-0004-1
Swennen GRJ, Mollemans W, Schutyser F (2009) Three-dimensional treatment planning of orthognathic surgery in the era of virtual imaging. J Oral Maxillofac Surg 67:2080–2092. https://doi.org/10.1016/j.joms.2009.06.007
Stokbro K, Aagaard E, Torkov P et al (2014) Virtual planning in orthognathic surgery. Int J Oral Maxillofac Surg 43:957–965. https://doi.org/10.1016/j.ijom.2014.03.011
Metzger MC, Hohlweg-Majert B, Schwarz U et al (2008) Manufacturing splints for orthognathic surgery using a three-dimensional printer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105:e1-7. https://doi.org/10.1016/j.tripleo.2007.07.040
Schouman T, Rouch P, Imholz B et al (2015) Accuracy evaluation of CAD/CAM generated splints in orthognathic surgery: a cadaveric study. Head Face Med 11:24. https://doi.org/10.1186/s13005-015-0082-9
Rückschloß T, Ristow O, Müller M et al (2019) Accuracy of patient-specific implants and additive-manufactured surgical splints in orthognathic surgery - A three-dimensional retrospective study. J Craniomaxillofac Surg 47:847–853. https://doi.org/10.1016/j.jcms.2019.02.011
Mazzoni S, Bianchi A, Schiariti G et al (2015) Computer-aided design and computer-aided manufacturing cutting guides and customized titanium plates are useful in upper maxilla waferless repositioning. J Oral Maxillofac Surg 73:701–707. https://doi.org/10.1016/j.joms.2014.10.028
Heufelder M, Wilde F, Pietzka S et al (2017) Clinical accuracy of waferless maxillary positioning using customized surgical guides and patient specific osteosynthesis in bimaxillary orthognathic surgery. J Craniomaxillofac Surg 45:1578–1585. https://doi.org/10.1016/j.jcms.2017.06.027
Schouman T, Murcier G, Goudot P (2015) The key to accuracy of zygoma repositioning: Suitability of the SynpliciTi customized guide-plates. J Craniomaxillofac Surg 43:1942–1947. https://doi.org/10.1016/j.jcms.2014.12.014
Kim H, Cha K-S (2018) Evaluation of the stability of maxillary expansion using cone-beam computed tomography after segmental Le Fort I osteotomy in adult patients with skeletal Class III malocclusion. Korean J Orthod 48:63–70. https://doi.org/10.4041/kjod.2018.48.1.63
Kretschmer WB, Baciut G, Baciut M et al (2011) Transverse stability of 3-piece Le Fort I osteotomies. J Oral Maxillofac Surg 69:861–869. https://doi.org/10.1016/j.joms.2010.05.024
Parizotto JOL, Borsato KT, Peixoto AP et al (2020) Can palatal splint improve stability of segmental Le Fort I osteotomies? Orthod Craniofac Res 23:486–492. https://doi.org/10.1111/ocr.12399
Pancherz H (1991) The nature of Class II relapse after Herbst appliance treatment: a cephalometric long-term investigation. Am J Orthod Dentofacial Orthop 100:220–233. https://doi.org/10.1016/0889-5406(91)70059-6
Hoppenreijs TJ, van der Linden FP, Freihofer HP et al (1998) Stability of transverse maxillary dental arch dimensions following orthodontic-surgical correction of anterior open bites. Int J Adult Orthodon Orthognath Surg 13:7–22
Rossetti RA, Cavanagh NJ, Goldberg MH (1993) Transpalatal rigid fixation of the maxillary sagittal osteotomy in Le Fort I orthognathic surgery. J Oral Maxillofac Surg 51:710–711. https://doi.org/10.1016/s0278-2391(10)80279-4
Acknowledgements
The authors would like to thank Guillaume Dubois and Mathieu Charles at Materialise Medical France (Malakoff, France) for providing a Mimics Suite licence and support in performing the measurements. We also thank the orthodontist, Laure Guittard, for her collaboration with this article, especially for the clinical analysis of occlusion stability.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent
Not applicable.
Conflict of interest
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Dr Thomas Schouman is a consultant for Materialise. Dr Thomas Schouman and Pr. Patrick Goudot are co-inventors of the SynpliciTi. The other authors declare no financial disclosures or conflicts of interest.
The Institutional Review Board that approved the study was the Research Ethics Committee of Sorbonne University. (Approval N°: CER-2020–101).
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Galli, P., Foy, JP., Le Roux, MK. et al. Stability of maxillary expansion osteotomy using patient-specific fixation implants without necessitating removable appliances: a retrospective analysis. Clin Oral Invest 27, 3393–3403 (2023). https://doi.org/10.1007/s00784-023-05082-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05082-3