Abstract
Objectives
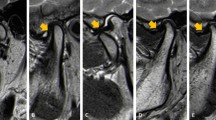
This pilot morphological study aimed to investigate the association between anterior disc displacement (ADD) and the status of the mandibular condyle and articular fossa.
Materials and methods
Thirty-four patients were divided into a normal articular disc position group and an ADD with and without reduction group. Images reconstructed were used to determine multiple group comparisons of these three different types of disc position, and the diagnostic efficacy for the morphological parameters with significant group difference was analyzed to assess.
Results
The condylar volume (CV), condylar superficial area (CSA), superior joint space (SJS), and medial joint space (MJS) all exhibited obvious changes (P < 0.05). Additionally, they all had a reliable diagnostic accuracy in differentiating between normal disc position and ADD with an AUC value from 0.723 to 0.858. Among them, the CV, SJS, and MJS (P < 0.05) had a significantly positive impact on the groups by analysis of multivariate logistic ordinal regression model.
Conclusions
The CV, CSA, SJS, and MJS are significantly associated with different disc displacement types. The condyle in ADD exhibited altered dimensions. These could be promising biometric markers for assessing ADD.
Clinical relevance
The morphological changes of mandibular condyle and glenoid fossa were significantly influenced by the status of disc displacement, and condyles with disc displacement had three-dimensionally altered condylar dimensions, irrespective of age and sex.






Similar content being viewed by others
Abbreviations
- ADD:
-
anterior disc displacement
- AJS:
-
anterior joint space
- AUC:
-
area under the curve
- CBCT:
-
cone beam computed tomography
- CSA:
-
condylar superficial area
- CSA%:
-
the proportion of the condylar superficial area in the articular fossa
- CV:
-
condylar volume
- CV%:
-
the proportion of the condylar volume in the articular fossa
- FSA:
-
fossa superficial area
- FV:
-
fossa volume
- MJS:
-
medial joint space
- MRI:
-
magnetic resonance imaging
- NADP:
-
normal articular disc position
- OR:
-
odds ratio
- PJS:
-
posterior joint space
- RDC/TMD:
-
Research Diagnostic Criteria for Temporomandibular Disorders
- ROC:
-
receiver-operating characteristic
- SJS:
-
superior joint space
- TMJ:
-
temporomandibular joint
References
Wieckiewicz M, Grychowska N, Wojciechowski K, Pelc A, Augustyniak M, Sleboda A, Zietek M (2014) Prevalence and correlation between TMD based on RDC/TMD diagnoses, oral parafunctions and psychoemotional stress in Polish university students. Biomed Res Int 2014:472346. https://doi.org/10.1155/2014/472346
Habib SR, Al Rifaiy MQ, Awan KH, Alsaif A, Alshalan A, Altokais Y (2015) Prevalence and severity of temporomandibular disorders among university students in Riyadh. Saudi Dent J 27(3):125–130. https://doi.org/10.1016/j.sdentj.2014.11.009
Cai XY, Jin JM, Yang C (2011) Changes in disc position, disc length, and condylar height in the temporomandibular joint with anterior disc displacement: a longitudinal retrospective magnetic resonance imaging study. J Oral Maxillofac Surg 69(11):e340–e346. https://doi.org/10.1016/j.joms.2011.02.038
Rd L, Previdelli IT, Rd S, Iwaki LC, Grossmann E, Filho LI (2016 Oct) Correlation of gender and age with magnetic resonance imaging findings in patients with arthrogenic temporomandibular disorders: a cross-sectional study. Int J Oral Maxillofac Surg 45(10):1222–1228. https://doi.org/10.1016/j.ijom.2016.04.016
Tanaka E, Detamore MS, Mercuri LG (2008) Degenerative disorders of the temporomandibular joint: etiology, diagnosis, and treatment. J Dent Res 87(4):296–307. https://doi.org/10.1177/154405910808700406
Lopes SL, Costa AL, Cruz AD, Li LM, de Almeida SM (2012) Clinical and MRI investigation of temporomandibular joint in major depressed patients. Dentomaxillofac Radiol 41(4):316–322. https://doi.org/10.1259/dmfr/27328352
Langendoen J, Müller J, Jull GA (1997) Retrodiscal tissue of the temporomandibular joint: clinical anatomy and its role in diagnosis and treatment of arthropathies. Man Ther 2(4):191–198. https://doi.org/10.1054/math.1997.0299
Keith DA, Shaefer JR (2003) Encyclopedia of the neurological sciences. ACADEMIC PRESS, Elsevier Science Inc, pp 495–498 (online version http://info.sciencedirect.com/reference_works/)
Buescher JJ (2007) Temporomandibular joint disorders. Am Fam Physician 76(10):1477–1482
Gauer RL, Semidey MJ (2015) Diagnosis and treatment of temporomandibular disorders. Am Fam Physician 91(6):378–386
Okeson JP, de Leeuw R (2011) Differential diagnosis of temporomandibular disorders and other orofacial pain disorders. Dent Clin North Am 55(1):105–120. https://doi.org/10.1016/j.cden.2010.08.007
Zakrzewska JM (2013) Differential diagnosis of facial pain and guidelines for management. Br J Anaesth 111(1):95–104. https://doi.org/10.1093/bja/aet125
Song H, Lee JY, Huh KH, Park JW (2020) Long-term changes of temporomandibular joint osteoarthritis on computed tomography. Sci Rep 10(1):6731. https://doi.org/10.1038/s41598-020-63493-8
Gundlach KK (2010) Ankylosis of the temporomandibular joint. J Craniomaxillofac Surg 38(2):122–130. https://doi.org/10.1016/j.jcms.2009.04.006
Movahed R, Mercuri LG (2015) Management of temporomandibular joint ankylosis. Oral Maxillofac Surg Clin North Am 27(1):27–35. https://doi.org/10.1016/j.coms.2014.09.003
Goh YC, Tan CC, Lim D (2020 Sep) Coronoid hyperplasia: a review. J Stomatol Oral Maxillofac Surg 121(4):397–403. https://doi.org/10.1016/j.jormas.2019.12.019
Farronato M, Lucchina AG, Mortellaro C, Fama A, Galbiati G, Farronato G, Maspero C (2019) Bilateral hyperplasia of the coronoid process in pediatric patients: what is the gold standard for treatment? J Craniofac Surg 30(4):1058–1063. https://doi.org/10.1097/SCS.0000000000004768
Taşkaya-Yilmaz N, Oğütcen-Toller M (2001) Magnetic resonance imaging evaluation of temporomandibular joint disc deformities in relation to type of disc displacement. J Oral Maxillofac Surg 59(8):860–865; discussion 865-6. https://doi.org/10.1053/joms.2001.25015
Lee PP, Stanton AR, Hollender LG (2017) Greater mandibular horizontal condylar angle is associated with temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol 123(4):502–507. https://doi.org/10.1016/j.oooo.2016.12.008
Torres MG, Crusoé-Rebello IM, Rosário M, Albuquerque MC, Campos PS (2016) Morphometric features of the mandibular condyle and association with disk abnormalities. Oral Surg Oral Med Oral Pathol Oral Radiol 121(5):566–572. https://doi.org/10.1016/j.oooo.2016.01.020
Westesson PL, Bifano JA, Tallents RH, Hatala MP (1991) Increased horizontal angle of the mandibular condyle in abnormal temporomandibular joints. A magnetic resonance imaging study. Oral Surg Oral Med Oral Pathol 72(3):359–363. https://doi.org/10.1016/0030-4220(91)90233-3
Larheim TA, Abrahamsson AK, Kristensen M, Arvidsson LZ (2015) Temporomandibular joint diagnostics using CBCT. Dentomaxillofac Radiol 44(1):20140235. https://doi.org/10.1259/dmfr.20140235
Reiter S, Goldsmith C, Emodi-Perlman A, Friedman-Rubin P, Winocur E (2012) Masticatory muscle disorders diagnostic criteria: the American Academy of Orofacial Pain versus the research diagnostic criteria/temporomandibular disorders (RDC/TMD). J Oral Rehabil 39(12):941–947. https://doi.org/10.1111/j.1365-2842.2012.02337.x
Li C, Liu X, Muhetaer B, Jumatai S, Gong Z Magnetic resonance imaging texture analysis of unilateral lateral pterygoid myospasm in patients with temporomandibular joint disorders: a pilot study. Digit Med [serial online] 2021 [cited 2022 9];7:2. Available from: http://www.digitmedicine.com/text.asp?2021/7/1/0/331949
Tomas X, Pomes J, Berenguer J, Quinto L, Nicolau C, Mercader JM, Castro V (2006) MR imaging of temporomandibular joint dysfunction: a pictorial review. Radiographics 26(3):765–781. https://doi.org/10.1148/rg.263055091
Fu KY, Hu M, Yu Q, Yang C, Cheng Y, Long X, Zhang ZG, Liu HC (2020) Experts consensus on MRI examination specification and diagnostic criteria of temporomandibular joint disc displacement. Chinese J Stomatol 55(9):608–612. https://doi.org/10.3760/cma.j.cn112144-20200514-00268
Fu KY, Hu M, Yu Q, Yang C, Cheng Y, Long X, Zhang ZG, Liu HC (2020) Experts consensus on cone-beam CT examination specification and diagnostic criteria of temporomandibular disorders. Chinese J Stomatol 55(9):613–616. https://doi.org/10.3760/cma.j.cn112144-20200514-00267
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Liu MQ, Zhang XW, Fan WP, He SL, Wang YY, Chen ZY (2020) Functional changes of the lateral pterygoid muscle in patients with temporomandibular disorders: a pilot magnetic resonance images texture study. Chin Med J (Engl) 133(5):530–536. https://doi.org/10.1097/CM9.0000000000000658
Dupuy-Bonafé I, Otal P, Montal S, Bonafé A, Maldonado IL (2014) Biometry of the temporomandibular joint using computerized tomography. Surg Radiol Anat 36(9):933–939. https://doi.org/10.1007/s00276-014-1277-7
Zhang Y, Xu X, Liu Z (2017) Comparison of morphologic parameters of temporomandibular joint for asymptomatic subjects using the two-dimensional and three-dimensional measuring methods. J Healthc Eng 2017:5680708. https://doi.org/10.1155/2017/5680708
Zhang YL, Song JL, Xu XC, Zheng LL, Wang QY, Fan YB, Liu Z (2016) Morphologic analysis of the temporomandibular joint between patients with facial asymmetry and asymptomatic subjects by 2D and 3D evaluation: a preliminary study. Medicine (Baltimore) 95(13):e3052. https://doi.org/10.1097/MD.0000000000003052
Kurita H, Uehara S, Yokochi M, Nakatsuka A, Kobayashi H, Kurashina K (2006) A long-term follow-up study of radiographically evident degenerative changes in the temporomandibular joint with different conditions of disk displacement. Int J Oral Maxillofac Surg 35(1):49–54. https://doi.org/10.1016/j.ijom.2005.04.004
Ueki K, Moroi A, Sotobori M, Ishihara Y, Marukawa K, Yoshizawa K, Kato K, Kawashiri S (2012) Changes in temporomandibular joint and ramus after sagittal split ramus osteotomy in mandibular prognathism patients with and without asymmetry. J Craniomaxillofac Surg 40(8):821–827. https://doi.org/10.1016/j.jcms.2012.03.003
Cevidanes LH, Hajati AK, Paniagua B, Lim PF, Walker DG, Palconet G, Nackley AG, Styner M, Ludlow JB, Zhu H, Phillips C (2010) Quantification of condylar resorption in temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110(1):110–117. https://doi.org/10.1016/j.tripleo.2010.01.008
Goncalves JR, Wolford LM, Cassano DS, da Porciuncula G, Paniagua B, Cevidanes LH (2013) Temporomandibular joint condylar changes following maxillomandibular advancement and articular disc repositioning. J Oral Maxillofac Surg 71(10):1759.e1–1759.15. https://doi.org/10.1016/j.joms.2013.06.209
Yang HJ, Hwang SJ (2014) Change in condylar position in posterior bending osteotomy minimizing condylar torque in BSSRO for facial asymmetry. J Craniomaxillofac Surg 42(4):325–332. https://doi.org/10.1016/j.jcms.2013.05.021
Chang MS, Choi JH, Yang IH, An JS, Heo MS, Ahn SJ (2018) Relationships between temporomandibular joint disk displacements and condylar volume. Oral Surg Oral Med Oral Pathol Oral Radiol 125(2):192–198. https://doi.org/10.1016/j.oooo.2017.11.001
Ahn SJ, Kim TW, Lee DY, Nahm DS (2006) Evaluation of internal derangement of the temporomandibular joint by panoramic radiographs compared with magnetic resonance imaging. Am J Orthod Dentofacial Orthop 129(4):479–485. https://doi.org/10.1016/j.ajodo.2005.12.009
Rao VM, Babaria A, Manoharan A, Mandel S, Gottehrer N, Wank H, Grosse S (1990) Altered condylar morphology associated with disc displacement in TMJ dysfunction: observations by MRI. Magn Reson Imaging 8(3):231–235. https://doi.org/10.1016/0730-725x(90)90094-i
Cevidanes LH, Walker D, Schilling J, Sugai J, Giannobile W, Paniagua B, Benavides E, Zhu H, Marron JS, Jung BT, Baranowski D, Rhodes J, Nackley A, Lim PF, Ludlow JB, Nguyen T, Goncalves JR, Wolford L, Kapila S, Styner M (2014) 3D osteoarthritic changes in TMJ condylar morphology correlates with specific systemic and local biomarkers of disease. Osteoarthr Cartil 22(10):1657–1667. https://doi.org/10.1016/j.joca.2014.06.014
Fernández Sanromán J, Gómez González JM, del Hoyo JA (1998) Relationship between condylar position, dentofacial deformity and temporomandibular joint dysfunction: an MRI and CT prospective study. J Craniomaxillofac Surg 26(1):35–42. https://doi.org/10.1016/s1010-5182(98)80033-4
Ueki K, Nakagawa K, Takatsuka S, Shimada M, Marukawa K, Takazakura D, Yamamoto E (2000) Temporomandibular joint morphology and disc position in skeletal class III patients. J Craniomaxillofac Surg 28(6):362–368. https://doi.org/10.1054/jcms.2000.0181
Nebbe B, Major PW, Prasad NG (1998) Adolescent female craniofacial morphology associated with advanced bilateral TMJ disc displacement. Eur J Orthod 20(6):701–712. https://doi.org/10.1093/ejo/20.6.701
Acknowledgements
The deepest appreciation is for Dr. Tao Bu (Parexel International) who provided a professional support for the statistics.
Data availability
The analyzed data sets generated during the study are available from the corresponding author on reasonable request.
Funding
This study was funded by the National Natural Science Foundation of China (grant number: 82160189); Hubei Province Key Laboratory of Oral and Maxillofacial Development and Regeneration, Wuhan 430022, China (grant number: 2022kqhm008); Tianshan Innovation Team of Xinjiang Uygur Autonomous Region (grant number: 2021D14001); and Open Project of Shaanxi Clinical Medical Research Center for Dental and Maxillofacial Diseases—School of Stomatology, Xi’an Jiaotong University (grant number 2020YHJB01).
Author information
Authors and Affiliations
Contributions
Prof. Gong conceptualized and designed the study and critically revised the manuscript for important intellectual content. Dr. Li conceptualized the study, designed the data collection, trained for measurement, optimized the statistical methods, and drafted the manuscript. Prof. Liu and Li supported MRI information extraction and interpreted the images and coordinated and supervised imaging data acquisition. X. Liu and Prof. Ling collected and integrated the clinical materials, took in charge of follow-up assignment, carried out the statistical analyses, and reviewed the manuscript.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. The requirements for authorship as stated earlier in this document have been met, and each author believes that the manuscript represents honest work.
Corresponding authors
Ethics declarations
Ethics approval
The present study was approved by the Ethics Committee of the First Affiliated Hospital of Xinjiang Medical University. Procedures operated in this research were completed in keeping with the standards set out in the Announcement of Helsinki and laboratory guidelines of research in China.
Consent for publication
Written consent was obtained by all patients, and they were willing to join our study and publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, Cx., Liu, H., Gong, Zc. et al. Effects of osseous structure based on three-dimensional reconstructive imaging evaluation in the assessment of temporomandibular joint disc position. Clin Oral Invest 27, 1449–1463 (2023). https://doi.org/10.1007/s00784-023-04936-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04936-0