Abstract
Objective
To investigate the effect of different concentrations of platelet-rich plasma (PRP) on collagen formation via periodontal ligament fibroblasts (PDLFs) on the surface of demineralised diseased tooth roots.
Methods
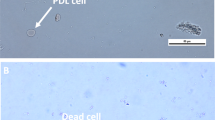
Various PDLFs were grown from tissue explants, with the cells between the fifth and eighth passage in the culture used. Human whole blood obtained from healthy subjects was collected in tubes containing an anticoagulant (acid-citrate-dextrose) and centrifuged (1300 rpm for 10 min) before the supernatant PRP layer was removed. A second spin at (2000 rpm for 10 min) produced the PRP fraction. The effect of PRP of various concentrations on the attachment of PDLFs on the diseased root surface of human teeth demineralised with ethylenediaminetetraacetic acid (EDTA) and treated with the PRP was then investigated in terms of PRP collagen formation, with the formation observed using the Sirius red staining method.
Results
The optical density values of the experimental groups were statistically significantly higher than those of the control groups (P < 0.05), while the Sirius red staining returned positive results for both the experimental group (A) and the control group (B). The images were analysed using a histogram, and a statistically significant difference was found (P < 0.05).
Conclusion
While PRP could promote the attachment and collagen formation of PDLFs on the diseased root surface of human teeth demineralised with EDTA and treated with PRP, the effect is potentially reduced when the dose exceeds 20%.




Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article.
References
Sedghi L, DiMassa V, Harrington A, Lynch SV, Kapila YL (2000) (2021) The oral microbiome: role of key organisms and complex networks in oral health and disease. Periodontol 87(1):107–131. https://doi.org/10.1111/prd.12393
Darveau RP, Curtis MA (2021) Oral biofilms revisited: a novel host tissue of bacteriological origin. Periodontology 2000 86(1):8–13. https://doi.org/10.1111/prd.12374
Joseph S, Curtis MA (2021) Microbial transitions from health to disease. Periodontology 2000 86(1):201–209. https://doi.org/10.1111/prd.12377
Jakubovics NS, Goodman SD, Mashburn-Warren L, Stafford GP, Cieplik F (2021) The dental plaque biofilm matrix. Periodontology 2000 86(1):32–56. https://doi.org/10.1111/prd.12361
Sodek J, Overall CM (1992) Metalloproteinases in periodontal tissue remodeling. Matrix Suppl 1:352–362
Lin CX, Hui NT (2003) PDGF-C and PDGF-D: novel members of the PDGF family. Mol Cardiol China 5(5):738–743. https://doi.org/10.3969/j.issn.1671-6272.2005.05.008
Wang JS (1996) Basic fibroblast growth factor for stimulation of bone formation in osteoinductive or conductive implants. Acta Orthop Scand Suppl 269:1–33. https://doi.org/10.3109/17453679609155229
Hammarstrom L (1997) The role of enamel matrix proteins in the development of cementum and periodontal tissues. Ciba Found Symp 205:246–55. https://doi.org/10.1002/9780470515303.ch17 (discussion 255-60)
Liu H, Wu ZF, Wang QT (1999) Effect of recombinant human Insulin-like growth factor-I and recombinant human bone morphogenetic protein-2 on proliferation of human periodontal ligament cells. Chin J Conser Dent 9(1):31–33
Ma WH, Shi XS, Li YF (2001) Study of osteogenesis of bone formation protein (BMP) in bone repair and its current application. Orthop J China 8(2):167–170. https://doi.org/10.3969/j.issn.1005-8478.2001.02.022
Antitua E (1999) Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. Int J Oral Maxillofac Implants 14(4):529–535
Luo K, Yan FH, Jin Y, Liu Y, Zhao Y, Wang XW (2003) Reconstruction of the guided tissue regeneration membrane combined with cultured cells by tissue engineering. Chin J Conserv Dent 13(03):139–141. https://doi.org/10.3969/j.issn.1005-2593.2003.03.007
Ripamonti U, Heliotis M, van den Heever B, Reddi AH (1994) Bone morphogenetic proteins induce periodontal regeneration in the baboon (Papio ursinus). J Periodontal Res 29(6):439–445. https://doi.org/10.1111/j.1600-0765.1994.tb01246.x
Okuda K, Kawase T, Momose M et al (2003) Platelet-rich plasma contains high levels of platelet-derived growth factor and transforming growth factor-beta and modulates the proliferation of periodontally related cells in vitro. J Periodontol 74(6):849–857. https://doi.org/10.1902/jop.2003.74.6.849
Liu Q, Victor M, Mark B (2004) Evaluation of effects of biodegradable membranes treated with platelet-rich plasma or platelet-poor plasma to the periodontal ligament fibroblasts by scanning electron microscopy. J Endod Periodontol 14(8):439–442. https://doi.org/10.3969/j.issn.1005-2593.2004.08.006
Li CZ, Fan MW, Tang ZJ (1997) Detection of type I, III and IV collagen in human dental bone, periodontium and alveolar bone. Chin J Stomatol 32(02):70–72
Narayanan AS, Baartold PM (1996) Biochemistry of periodontal connective tissues and their regeneration: a current perspective. Connect Tissue Res 34(3):191–201. https://doi.org/10.3109/03008209609000698
Gonshor A (2002) Technique for producing platelet-rich plasma and platelet concentrate: background and process. Int J Periodontics Restorative Dent 22(6):547–557
Pfeilschifter J, Oechsner M, Naumann A, Gronwald RG, Minne HW, Ziegler R (1990) Stimulation of bone matrix apposition in vitro by local growth factors: a comparison between insulin-like growth factor I, platelet-derived growth factor, and transforming growth factor beta. Endocrinology 127(1):69–75. https://doi.org/10.1210/endo-127-1-69
Whitman DH, Berry RL, Green DM (1997) Platelet gel: an autologous alternative to fibrin glue with applications in oral and maxillofacial surgery. J Oral Maxillofac Surg 55(11):1294–1299. https://doi.org/10.1016/s0278-2391(97)90187-7
Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR (1998) Platelet-rich plasma: growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 85(6):638–646. https://doi.org/10.1016/s1079-2104(98)90029-4
Camargo PM, Lekovic V, Weinlaender M, Vasilic N, Madzarevic M, Kenney EB (2002) Platelet-rich plasma and bovine porous bone mineral combined with guided tissue regeneration in the treatment of intrabony defects in humans. J Periodontal Res 37(4):300–306. https://doi.org/10.1034/j.1600-0765.2002.01001.x
Parkar MH, Kuru L, Giouzeli M, Olsen I (2001) Expression of growth-factor receptors in normal and regenerating human periodontal cells. Arch Oral Biol 46(3):275–284. https://doi.org/10.1016/s0003-9969(00)00099-6
Matsuda S, Shoumura M, Osuga N et al (2016) Migration and differentiation of GFP-transplanted bone marrow-derived cells into experimentally induced periodontal polyp in mice. Int J Med Sci 13(7):500–506
Somerman MJ, Archer SY, Imm GR, Foster RA (1988) A comparative study of human periodontal ligament cells and gingival fibroblasts in vitro. J Dent Res 67(1):66–70. https://doi.org/10.1177/00220345880670011301
SiTu ZQ, Wu JZ (1996) Cell culture. World Book Publishing Company, Xi ’an, p 6971
Lekovic V, Camargo PM, Weinlaender M, Vasilic N, Kenney EB (2002) Comparison of platelet-rich plasma, bovine porous bone mineral, and guided tissue regeneration versus platelet-rich plasma and bovine porous bone mineral in the treatment of intrabony defects: a reentry study. J Periodontol 73(2):198–205. https://doi.org/10.1902/jop.2002.73.2.198
Kassolis JD, Rosen PS, Reynolds MA (2000) Alveolar ridge and sinus augmentation utilizing platelet-rich plasma in combination with freeze-dried bone allograft: case series. J Periodontol 71(10):1654–1661. https://doi.org/10.1902/jop.2000.71.10.1654
de Obarrio JJ, Araúz-Dutari JI, Chamberlain TM, Croston A (2000) The use of autologous growth factors in periodontal surgical therapy: platelet gel biotechnology–case reports. Int J Periodontics Restorative Dent 20(5):486–497
Petrungaro PS (2001) Using platelet - rich plasma to accelerate soft tissue maturation in esthetic periodontal surgery. Compend Contin Educ Dent 22(9):729–32 (734, 736 passim; quiz 746)
Landesberg R, Roy M, Glickman RS (2000) Quantification of growth factor levels using simplified method of platelet-rich plasma gel preparation. J Oral Maxillofac Surg 58(3):297–300. https://doi.org/10.1016/s0278-2391(00)90058-2 (discussion 300-1)
Marx RE (2001) Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent 10(4):225–228. https://doi.org/10.1097/00008505-200110000-00002
Metcalfe P, Williamson LM, Reutelingsperger CP, Swann I, Ouwehand WH, Goodall AH (1997) Activation during preparation of therapeutic platelets affects deterioration during storage: a comparative flow cytometric study of different production methods. Br J Haematol 98(1):86–95. https://doi.org/10.1046/j.1365-2141.1997.1572983.x
Dugrillon A, Eichler H, Kern S, Klüter H (2002) Autologous concentrated platelet-rich plasma (cPRP) for local application in bone regeneration. Int J Oral Maxillofac Surg 31(6):615–619. https://doi.org/10.1054/ijom.2002.0322
Carlson NE, Roach RB Jr (2002) platelet-rich:clinical applications in dentistry. J Am Dent Assoc 33(10):1383–1386. https://doi.org/10.14219/jada.archive.2002.0054
Sonnleitner D, Huemer P, Sullivan DY (2000) A simplified technique for producing platelet-rich plasma and platelet concentrate for inraoral bone grafting Techniques: a tectnical note. Int J Oral Maxillofac Implants 15(6):879–882
Schilephake H (2002) Bone growth factors in maxillofacial skeletal reconstruction. Int J Oral Maxillofac Surg 31(5):469–484. https://doi.org/10.1054/ijom.2002.0244
Lucarelli E, Beccheroni A, Donati D et al (2003) Platelet-drived growth factor enhance proliferation of human stromal stem cells. Biomaterials 24(18):3095–100. https://doi.org/10.1016/s0142-9612(03)00114-5
Weibrich G, Kleis WK, Hafner G, Hitzler WE (2002) Growth factor levels in platelet-rich plasma and correlations with donor age, sex, and platelet count. J Craniomaxillofac Surg 30(2):97–102. https://doi.org/10.1054/jcms.2002.0285
Dai HY, Liu Q, Zhang HY (2007) Promoting the attachment and proliferation of periodontal fibroblasts on the root surface of diseased teeth. J Pract Dent 23(04):595–597. https://doi.org/10.3969/j.issn.1001-3733.2007.04.042
Liu Q, Victor M, Mark B (2006) Development of novel cell delivery carrier for Periodontal Regeneration in vitro. West China J Stomatol 24(1):15–17, 35. https://doi.org/10.3321/j.issn:1000-1182.2006.01.004
Lowenguth RA, Blieden TM (1993) Periodontal regeneration: root surface. Periodontol 2000 1:5468
Pitaru S, Melcher AH (1987) Organization of and oriented fiber system in vitro by human gingival fibroblasts attached to dental tissues: relationship between cell sand mineralized and demineralized tissue. J Periodont Res 22(1):6–13. https://doi.org/10.1111/j.1600-0765.1987.tb01533.x
Blomlöf J, Jansson L, Blomlöf L, Lindskog S (1996) Root surface etching at neutral pH promotes periodontal healing. J Clin Periodontol 23(1):50–55. https://doi.org/10.1111/j.1600-051x.1996.tb00504.x
Sculean A, Donos N, Brecx M, Reich E, Karring T (2000) Treatment of intrabony defects with guided tissue regeneration and enamel-matrix-proteins. An experimental study in monkeys. J Clin Periodontol 27(7):466–72. https://doi.org/10.1034/j.1600-051x.2000.027007466.x
Butler WT, Birkeda-HansenH BWF, Taylor RE, Chung E (1975) Proteins of the periodontium. Identification of collagens with the [alpha1(I)]2alpha2 and [alpha1(III)]3 structures in bovine periodontal ligament. J Biol Chem 250:8907–8912
Hillmann G, Gebert A, Geurtsen W (1999) Matrix expression and proliferation of primary gingival fibroblasts in a three-dimensional cell culture model. J Cell Sci 112(Pt 17):2823–2832
Giannobile WV, Lee CS, Tomala MP, Tejeda KM, Zhu Z (2001) Platelet-derived growth factor (PDGF) gene delivery for application in periodontal tissue engineering. J Periodontol 72(6):815–823. https://doi.org/10.1902/jop.2001.72.6.815
Author information
Authors and Affiliations
Contributions
QY have made substantial contributions to conception and design; QY and XXB acquisition of data, analysis and interpretation of data; QY and XXB have been involved in drafting the manuscript and revising it critically for important intellectual content; XXB have given final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Hefei stomatological hospital (NO. 2021–201010). Written informed consent was obtained from all parents/local guardians for participants.
Consent for publication
The manuscript is not submitted for publication or consideration elsewhere.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qian, Y., Qian, X. & Xu, XB. Effect of platelet-rich plasma on the attachment of periodontal ligament fibroblasts to the diseased root surface and the attendant collagen formation. Clin Oral Invest 27, 529–539 (2023). https://doi.org/10.1007/s00784-022-04748-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04748-8