Abstract
Objectives
Free fibula flap is the first choice for jaw reconstruction in head and neck oncology, but postoperative complications in donor site are ignored always. The main purpose of this study was to investigate the long-term complications and potential risk factors of donor site after vascularized fibular transplantation, and to explore the precautions of preparing vascularized fibular flap and the measures of preventing donor site complications.
Materials and methods
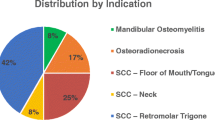
Data were retrospectively collected on 31 patients who had undergone immediate mandibular reconstruction with a fibular flap after segmental mandibulectomy from 2013 to 2018 in Shanghai Ninth People’s Hospital. Thirty-one patients (24 male, 7 female) were available for the long-term complications in donor site analysis from 25 to 96 months after surgery. The data were collected and analyzed, including age at time of operation, early postoperative complications, incidence of dorsiflexion weakness of hallux, donor site missing fibula length, proximal and distal stump fibula length, and subjective evaluation of foot function (AOFAS-hallux, AOFAS-ankle hindfoot, Enneking lower limb function score). In the single-factor analysis in this study, the correlation between related factors and long-term complications was statistically analyzed. For inter-group comparisons of quantitative data, if the normal distribution was satisfied, two independent sample t-tests were used; p < 0.05 was statistical significant. If the normal distribution was not satisfied, Wilcoxon rank-sum test was used, and p < 0.05 was considered statistically significant. For qualitative data, the Fisher exact probability method was compared between group differences, and p < 0.05 was statistically significant.
Results
The most commonly encountered complication in our series was dorsiflexion disorder, flexion deformity, numbness of the lateral side of the lower leg, and dorsum of the foot. Ten patients (32.26%) developed hallux flexion deformity after operation, 17 patients (54.84%) had hallux dorsiflexion dysfunction after operation, and 10 patients (32.26%) had numbness of the lateral side of the lower leg and dorsum of the foot. The incidence of hallux dorsiflexion dysfunction, thumb flexion deformity, and sensory disturbance was higher than that of other long-term complications in the donor area. The residual length of fibular distal was related to the dorsiflexion dysfunction and flexion deformity of hallux (p < 0.05). The early complications of donor site were correlated with the hallux dorsiflexion dysfunction (p < 0.05).
Conclusions
The incidence of dorsiflexion disorder and flexion deformity is higher in patients after fibula transplantation. The less the residual length of fibular distal, the more obvious the long-term complications in the donor site, and the higher the incidence of dorsiflexion dysfunction and flexion deformity of hallux.
Clinical relevance
The long-term complications of donor site after fibular transplantation seriously affect the quality of life of patients and provide clinical reference for further reducing the occurrence of donor site complications.






Similar content being viewed by others
References
Di Giuli R, Zago M, Beltramini GA, Pallotta ML, Bolzoni A, Baj A, Giannì AB, Sforza C (2019) Donor-Site Morbidity After Osteocutaneous Free Fibula Transfer: Longitudinal Analysis of Gait Performance. J Oral Maxillofac Surg 77(3):648–657
Ling XF, Peng X (2012) What is the price to pay for a free fibula flap? A systematic review of donor-site morbidity following free fibula flap surgery. Plast Reconstr Surg 129(3):657–674
Xu ZF, Bai S, Zhang ZQ, Duan WY, Wang ZQ, Sun CF (2017) A critical assessment of the fibula flap donor site. Head Neck 39(2):279–287
Harris BN, Bewley AF (2016) Minimizing free flap donor-site morbidity. Curr Opin Otolaryngol Head Neck Surg 24(5):447–452
Momoh AO, Yu P, Skoracki RJ, Liu S, Feng L, Hanasono MM (2011) A prospective cohort study of fibula free flap donor-site morbidity in 157 consecutive patients. Plast Reconstr Surg 128(3):714–720
Lin JY, Djohan R, Dobryansky M, Chou SW, Hou WH, Chen MH, Wei FC (2009) Assessment of donor-site morbidity using balance and gait tests after bilateral fibula osteoseptocutaneous free flap transfer. Ann Plast Surg 62(3):246–251
Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ (1993) A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res (286):241–246
Zhang S, Han ZX (2015) Evaluation of donor site complications and function after transplantation of vascularized fibula. Beijing J Stomatol 23(06):325–328
Ni Y, Zhang X, Zhang Z, Liang W, Zhao L, Li Z, Li S, Lu P, Xu Z, Dai W, Duan W, Tan X, Sun C, Liu F (2020) Assessment of fibula flap with flexor hallucis longus’s effect on head & neck tumor patients’ quality of life and function of donor site. Oral Oncol 100:104489
Sieg P, Taner C, Hakim SG, Jacobsen HC (2010) Long-term evaluation of donor site morbidity after free fibula transfer. Br J Oral Maxillofac Surg 48(4):267–270
Rendenbach C, Rashad A, Hansen L, Kohlmeier C, Dyck ML, Suling A, Assaf AT, Amling M, Heiland M, Wikner J, Riecke B, Kreutzer K (2018) Functional donor site morbidity longer than one year after fibula free flap: a prospective biomechanical analysis. Microsurgery 38(4):395–401
Barla M, Polirsztok E, Peltié E, Jouve JL, Legré R, Dautel G, Barbary S, Journeau P (2017) Free vascularised fibular flap harvesting in children: An analysis of donor-site morbidity. Orthop Traumatol Surg Res 103(7):1109–1113
Ling XF, Peng X, Samman N. Donor-site morbidity of free fibula and DCIA flaps (2013) J Oral Maxillofac Surg 71(9):1604-1612
Wang YY, Fan S, Zhang DM, Lin ZY, Chen WL, Li JS (2016) Novel Local Full-Thickness Skin Grafts for Closure of Free Fibular Osteocutaneous Flap Donor Sites. J Oral Maxillofac Surg 74(1):200–203
Shindo M, Fong BP, Funk GF, Karnell LH (2000) The fibula osteocutaneous flap in head and neck reconstruction: a critical evaluation of donor site morbidity. Arch Otolaryngol Head Neck Surg 126(12):1467–1472
Kuvat SV, Keklik B, Özden BC, Uçar A, Cizmeci O (2012) Major donor area complication after a mandibular reconstruction with an osseous fibular free flap: pseudo-compartment syndrome. J Craniofac Surg 23(2):499–501
Ni Y, Zhang X, Zhang Z, Liang W, Zhao L, Li Z, Li S, Lu P, Xu Z, Dai W, Duan W, Tan X, Sun C, Liu F (2020) Assessment of fibula flap with flexor hallucis longus's effect on head & neck tumor patients' quality of life and function of donor site. Oral Oncol 100:104489
Wolff K-D, Hölzle F (2011) Raising of microvascular flaps a systematic approach (2nd ed. 2011.), Springer Berlin Heidelberg
Funding
This research was supported by the National Natural Science Foundation of China (no. 82170923) and Clinical Research Plan of SHDC” (SHDC2020CR3008A). Project funded by China Postdoctoral Science Foundation (2021TQ0206, 2021M690105).
Author information
Authors and Affiliations
Contributions
(I) Conception and design: all authors; (II) administrative support: corresponding author; (III) provision of study materials or patients: all authors; (IV) collection and assembly of data: the first author and common author; (V) data analysis and interpretation: all authors; (VI) manuscript writing: the first author; (VII) final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Ethics approval
The study protocol was approved by Medical Ethics Committee of the Ninth People’s Hospital Affiliated to Shanghai Jiaotong University School of Medicine (SH9H-2022-T58-1).
Consent to participate
All included patients agreed to use their medical data for research purposes.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, H., Mao, J., Zhai, Z. et al. Analysis of related factors of long-term complications after vascularized fibular transplantation. Clin Oral Invest 26, 6961–6971 (2022). https://doi.org/10.1007/s00784-022-04650-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04650-3