Abstract
Objective
To assess and compare the immuno-expression of p53 and TP 53 gene amplification and correlate local recurrence and survival in histologically negative surgical margins of oral squamous cell carcinoma (OSCC) with normal oral mucosa.
Methods
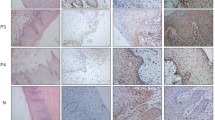
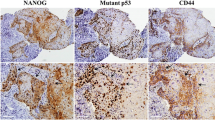
Forty formalin-fixed paraffin-embedded tissue blocks of HNMs of OSCC and 40 normal oral mucosa samples were analyzed for p53 immunostaining and TP 53 gene amplification by PCR.
Results
Significantly, higher positivity was noted with p53 immuno-expression, TP53 gene amplification, and combined p53 and TP53 expression in the study group compared to the control group (p < 0.05). Most cases that were positive for p53 immuno-expression, TP 53 gene amplification, and combined p53 and TP53 expression showed local recurrence and poor survival. Kaplan–Meier survival analysis showed that subjects with TP53 and combined p53 and TP53 positivity had decreased survival rate than their negative counterparts.
Conclusion
Detection of p53 in HNMs of OSCC can be used as a biomarker to identify patients at a higher risk of developing local recurrence and to predict survival.
Clinical relevance
Combined p53 and TP 53 assessment may be more reliable for predicting LR to help clinicians and surgeons in treatment planning.



Similar content being viewed by others
Change history
23 December 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00784-022-04834-x
References
Angadi PV, Patil PV, Hallikeri K, Mallapur MD, Hallikerimath S, Kale AD (2015) Tumor budding is an independent prognostic factor for prediction of lymph node metastasis in oral squamous cell carcinoma. Int J Surg Pathol 23(2):102–110. https://doi.org/10.1177/1066896914565022
More Y, D’Cruz AK (2013) Oral cancer: review of current management strategies. Natl Med J India 26(3):152–158
Oliveira LR, Ribeiro-Silva A, Costa JPO, Simões AL, Di MMAS, Zucoloto S (2008) Prognostic factors and survival analysis in a sample of oral squamous cell carcinoma patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106(5):685–695. https://doi.org/10.1016/j.tripleo.2008.07.002
Jelovac DB, Tepavčević Z, Nikolić N et al (2016) The amplification of c-erb-B2 in cancer-free surgical margins is a predictor of poor outcome in oral squamous cell carcinoma. Int J Oral Maxillofac Surg 45(6):700–705. https://doi.org/10.1016/j.ijom.2015.11.014
van Houten VMM, Leemans CR, Kummer JA et al (2004) Molecular diagnosis of surgical margins and local recurrence in head and neck cancer patients: a prospective study. Clin Cancer Res 10(11):3614–3620. https://doi.org/10.1158/1078-0432.CCR-03-0631
Mognetti B, Trione E, Corvetti G et al (2005) ΔNp63α as early indicator of malignancy in surgical margins of an oral squamous cell carcinoma. Oral Oncol Extra 41(7):129–131. https://doi.org/10.1016/j.ooe.2005.02.010
Bilde A, von Buchwald C, Dabelsteen E, Therkildsen MH, Dabelsteen S (2009) Molecular markers in the surgical margin of oral carcinomas. J Oral Pathol Med 38(1):72–78. https://doi.org/10.1111/j.1600-0714.2008.00715.x
Singh J, Jayaraj R, Baxi S et al (2016) Immunohistochemical expression levels of p53 and eIF4E markers in histologically negative surgical margins, and their association with the clinical outcome of patients with head and neck squamous cell carcinoma. Mol Clin Oncol 4(2):166–172. https://doi.org/10.3892/mco.2015.689
Yang X-H, Ding L, Fu Y et al (2019) p53-positive expression in dysplastic surgical margins is a predictor of tumor recurrence in patients with early oral squamous cell carcinoma. Cancer Manag Res 11:1465–1472. https://doi.org/10.2147/CMAR.S192500
de Carvalho AC, Kowalski LP, Campos AHJFM, Soares FA, Carvalho AL, Vettore AL (2012) Clinical significance of molecular alterations in histologically negative surgical margins of head and neck cancer patients. Oral Oncol 48(3):240–248. https://doi.org/10.1016/j.oraloncology.2011.10.018
Li MM, Puram SV, Silverman DA, Old MO, Rocco JW, Kang SY (2019) Margin analysis in head and neck cancer: state of the art and future directions. Ann Surg Oncol 26(12):4070–4080. https://doi.org/10.1245/s10434-019-07645-9
Shah AK (2018) Postoperative pathologic assessment of surgical margins in oral cancer: a contemporary review. J Oral Maxillofac Pathol 22(1):78–85. https://doi.org/10.4103/jomfp.JOMFP_185_16
Payne K (2017) Factors influencing the status of the surgical margin in the resection of oral squamous cell carcinoma. Biomed J Sci Tech Res 1(7):1835–1838. https://doi.org/10.26717/bjstr.2017.01.000562
Clark DJ, Mao L (2017) Understanding the surgical margin: a molecular assessment. Oral Maxillofac Surg Clin North Am 29(3):245–258. https://doi.org/10.1016/j.coms.2017.03.002
Adams EJ, Green JA, Clark AH, Youngson JH (1999) Comparison of different scoring systems for immunohistochemical staining. J Clin Pathol 52(1):75–77. https://doi.org/10.1136/jcp.52.1.75
Stoicănescu D, Andreescu N, Belengeanu A, Meszaros N, Cornianu M (2013) Assessment of p53 and HER-2/neu genes status and protein products in oral squamous cell carcinomas. Rom J Morphol Embryol 54(4):1107–1113
Elizabeth van Pelt-Verkuil Alex van Belkum John P. Hays (2008) Principles and technical aspects of PCR amplification. https://doi.org/10.1007/978-1-40206241-4
Heah KG, Hassan MIA, Huat SC (2011) p53 Expression as a marker of microinvasion in oral squamous cell carcinoma. Asian Pac J Cancer Prev 12(4):1017–1022
Gasco M, Crook T (2003) The p53 network in head and neck cancer. Oral Oncol 39(3):222–231. https://doi.org/10.1016/s1368-8375(02)00163-x
Nylander K, Dabelsteen E, Hall PA (2000) The p53 molecule and its prognostic role in squamous cell carcinomas of the head and neck. J Oral Pathol Med 29(9):413–425. https://doi.org/10.1034/j.1600-0714.2000.290901.x
Brennan JA, Mao L, Hruban RH et al (1995) Molecular assessment of histopathological staging in squamous-cell carcinoma of the head and neck. N Engl J Med 332(7):429–435. https://doi.org/10.1056/NEJM199502163320704
Wang X, Chen S, Chen X, Zhang C, Liang X (2016) Tumor-related markers in histologically normal margins correlate with locally recurrent oral squamous cell carcinoma: a retrospective study. J Oral Pathol Med 45(2):83–88. https://doi.org/10.1111/jop.12334
Warnakulasuriya S (2009) Global epidemiology of oral and oropharyngeal cancer. Oral Oncol 45(4–5):309–316. https://doi.org/10.1016/j.oraloncology.2008.06.002
Slootweg PJE (2005) Tumors of oral cavity and oropharynx: introduction. In: John LB, W. Eveson Peter Reichart David Sidransky, (eds) Pathology and genetics of head and neck tumours, 2005th edn. IARCPress International Agency for Research on Cancer (IARC) 69008 Lyon, France, pp 166–175
Prabhu SR (1992) Oral diseases in the tropics. Oxford University Press.
Chandra A, Singh A, Sebastian BT, Agnihotri A, Bali R, Verma PK (2013) Oral squamous cell carcinomas in age distinct population: a comparison of p53 immunoexpression. J Cancer Res Ther 9(4):587–591. https://doi.org/10.4103/0973-1482.126452
Sá C, Silva L, Cardoso S, Aguiar M, Carmo M (2006) p53 Immunoexpression in oral squamous cell carcinomas from different anatomical sites: a comparative study. Int J Morphol. 24. https://doi.org/10.4067/S0717-95022006000300018
Cruz IB, Meijer CJ, Snijders PJ, Snow GB, Walboomers JM, van Der Waal I (2000) p53 immunoexpression in non-malignant oral mucosa adjacent to oral squamous cell carcinoma: potential consequences for clinical management. J Pathol 191(2):132–137. https://doi.org/10.1002/(SICI)1096-9896(200006)191:2%3c132::AID-PATH605%3e3.0.CO;2-E
Cruz I, Napier SS, van der Waal I et al (2002) Suprabasal p53 immunoexpression is strongly associated with high grade dysplasia and risk for malignant transformation in potentially malignant oral lesions from Northern Ireland. J Clin Pathol 55(2):98–104. https://doi.org/10.1136/jcp.55.2.98
Acknowledgements
The authors would like to thank; a) the management of PAHER University, Udaipur for the support to complete the research, b) Dr. Umesh Hallikeri, Consultant pathologist and the entire management of Karnataka Cancer Therapy and Research Institute, Navanagar, Hubli for providing the specimens for the study, c) Dr. Sanjay Navani, Lab Surg Path, Mumbai, for immunohistochemical analysis, d) Dr. Kishore Bhat, Prof & Head, Research department, Maratha Mandal Nathajirao G. Halgekar Institute of Dental Sciences and Research Centre, Belagavi for PCR analysis and e) the management of Bharati Vidyapeeth, Bharati Vidyapeeth (Deemed to be University), Pune for their constant support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were following the ethical standards of the institutional and/or national research committee and with the Helsinki declaration.and its later amendments or comparable ethical standards. The research protocol was approved by the Department of Histopathology, Karnataka Cancer Therapy and Research Institute Ref- KCTRI- EC-01/2017, KCTRI Hubli, Karnataka, India.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
P53 protein expression by IHC was seen in Thirty-four (85%) HNMs. TP 53 gene analysis by PCR was seen in 27(67.5%) of HNMs. 38 (95%) HNMs & 18 (45%) of controls showed either p53 (IHC) or TP 53 (PCR) or both. Higher rate of localrecurrence was noted in p53, TP53, and p53 + TP53positive cases than p53, TP53,and p53 + TP53 negative cases respectively as assessed by logistic regression. TP 53 and p53 + TP 53 positivity were good predictors of survival in OSCC with HNMs.
The original version of this article was revised: This article was originally published with needed corrections in the body text.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kamat, M.S., Puranik, R.S., Das Rai, A.B. et al. Assessing immuno-expression of p53 protein and TP 53 gene amplification in histologically negative surgical margins of oral squamous cell carcinoma patients and normal oral mucosa. Clin Oral Invest 26, 6235–6243 (2022). https://doi.org/10.1007/s00784-022-04574-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04574-y