Abstract
Objectives
This experimental study was carried out to investigate the effects of locally delivered nanoparticles (AMG-487 NP) containing a CXCR3 antagonist in inhibiting the progression of LPS-induced inflammation, osteoclastic activity, and bone resorption on a murine model.
Materials and methods
Thirty, 7-week-old C57BL/6 J male mice were used. Inflammatory bone loss was induced by Porphyromonas gingivalis–lipopolysaccharide (P.g.-LPS) injections between the first and second maxillary molars, bilaterally, twice a week for 6 weeks (n = 20). AMG-487 NP were incorporated into a liposome carrier and locally delivered on sites where P.g.-LPS was injected. Control mice (n = 10) were injected with vehicle only. Experimental groups included (1) control, (2) LPS, and (3) LPS + NP. At the end of 1 and 6 weeks, mice were euthanized, maxillae harvested, fixed, and stored for further analysis.
Results
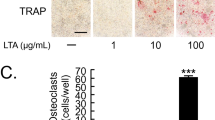
Volumetric bone loss analysis revealed, at 1 week, an increase in bone loss in the LPS group (47.9%) compared to control (27.4%) and LPS + NP (27.8%) groups. H&E staining demonstrated reduced inflammatory infiltrate in the LPS + NP group compared to LPS group. At 6 weeks, volumetric bone loss increased in all groups; however, treatment with the CXCR3 antagonist (LPS + NP) significantly reduced bone loss compared to the LPS group. CXCR3 antagonist treatment significantly reduced osteoclast numbers when compared to LPS group at 1 and 6 weeks.
Conclusions
This study showed that local delivery of a CXCR antagonist, via nanoparticles, in a bone resorption model, induced by LPS injection, was effective in reducing inflammation, osteoclast numbers, and bone loss.
Clinical relevance
CXCR3 blockade can be regarded as a novel target for therapeutic intervention of bone loss. It can be a safe and convenient method for periodontitis treatment or prevention applicable in clinical practice.




Similar content being viewed by others
References
Papapanou PN, Sanz M, Buduneli N et al (2018) Periodontitis: consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89(Suppl 1):S173–S182
Hajishengallis G, Chavakis T, Lambris JD (2000) Current understanding of periodontal disease pathogenesis and targets for host-modulation therapy. Periodontol 2000 84(1):14–34
Eke PI, Thornton-Evans GO, Wei L, Borgnakke WS, Dye BA, Genco RJ (2018) Periodontitis in US adults: National Health and Nutrition Examination Survey 2009–2014. J Am Dent Assoc 149(7):576–588 e576
Petersen PE (2003) The World Oral Health Report 2003: continuous improvement of oral health in the 21st century–the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 31(Suppl 1):3–23
Hajishengallis G, Darveau RP, Curtis MA (2012) The keystone-pathogen hypothesis. Nat Rev Microbiol 10(10):717–725
Sedghi L, DiMassa V, Harrington A, Lynch SV, Kapila YL (2021) The oral microbiome role of key organisms and complex networks in oral health and disease. Periodontol 2000 87(1):107–131
Joseph S, Curtis MA (2021) Microbial transitions from health to disease. Periodontol 2000 86(1):201–209
Abusleme L, Hoare A, Hong BY, Diaz PI (2021) Microbial signatures of health, gingivitis, and periodontitis. Periodontol 2000 86(1):57–78
Jepsen S, Caton JG, Albandar JM et al (2018) Periodontal manifestations of systemic diseases and developmental and acquired conditions: consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89(Suppl 1):S237–S248
Wade WG (2021) Resilience of the oral microbiome. Periodontol 2000 86(1):113–122
Darveau RP, Curtis MA (2021) Oral biofilms revisited: a novel host tissue of bacteriological origin. Periodontol 2000 86(1):8–13
Hajishengallis G, Lamont RJ (2021) Polymicrobial communities in periodontal disease Their quasi-organismal nature and dialogue with the host. Periodontol 2000 86(1):210–230
Pihlstrom BL, Michalowicz BS, Johnson NW (2005) Periodontal diseases. Lancet 366(9499):1809–1820
Hiyari S, Green E, Pan C et al (2018) Genomewide association study identifies Cxcl family members as partial mediators of LPS-induced periodontitis. J Bone Miner Res 33(8):1450–1463
Loetscher M, Gerber B, Loetscher P et al (1996) Chemokine receptor specific for IP10 and mig: structure, function, and expression in activated T-lymphocytes. J Exp Med 184(3):963–969
Loetscher M, Loetscher P, Brass N, Meese E, Moser B (1998) Lymphocyte-specific chemokine receptor CXCR3: regulation, chemokine binding and gene localization. Eur J Immunol 28(11):3696–3705
Luster AD, Unkeless JC, Ravetch JV (1985) Gamma-interferon transcriptionally regulates an early-response gene containing homology to platelet proteins. Nature 315(6021):672–676
Groom JR, Luster AD (2011) CXCR3 ligands: redundant, collaborative and antagonistic functions. Immunol Cell Biol 89(2):207–215
Groom JR, Luster AD (2011) CXCR3 in T cell function. Exp Cell Res 317(5):620–631
Groom JR, Richmond J, Murooka TT et al (2012) CXCR3 chemokine receptor-ligand interactions in the lymph node optimize CD4+ T helper 1 cell differentiation. Immunity 37(6):1091–1103
Dufour JH, Dziejman M, Liu MT, Leung JH, Lane TE, Luster AD (2002) IFN-gamma-inducible protein 10 (IP-10; CXCL10)-deficient mice reveal a role for IP-10 in effector T cell generation and trafficking. J Immunol 168(7):3195–3204
Ichikawa A, Kuba K, Morita M et al (2013) CXCL10-CXCR3 enhances the development of neutrophil-mediated fulminant lung injury of viral and nonviral origin. Am J Respir Crit Care Med 187(1):65–77
Igic M, Kostic M, Basic J et al (2020) Bleeding index and monocyte chemoattractant protein 1 as gingival inflammation parameters after chemical-mechanical retraction procedure. Med Princ Pract 29(5):492–498
Garlet GP, Martins W Jr, Ferreira BR, Milanezi CM, Silva JS (2003) Patterns of chemokines and chemokine receptors expression in different forms of human periodontal disease. J Periodontal Res 38(2):210–217
Gemmell E, Carter CL, Seymour GJ (2001) Chemokines in human periodontal disease tissues. Clin Exp Immunol 125(1):134–141
Sakai A, Ohshima M, Sugano N, Otsuka K, Ito K (2006) Profiling the cytokines in gingival crevicular fluid using a cytokine antibody array. J Periodontol 77(5):856–864
Aldahlawi S, Youssef AR, Shahabuddin S (2018) Evaluation of chemokine CXCL10 in human gingival crevicular fluid, saliva, and serum as periodontitis biomarker. J Inflamm Res 11:389–396
Guo X, Wang Y, Wang C, Chen J (2015) Identification of several hub-genes associated with periodontitis using integrated microarray analysis. Mol Med Rep 11(4):2541–2547
Guo YC, Chiu YH, Chen CP, Wang HS (2018) Interleukin-1beta induces CXCR3-mediated chemotaxis to promote umbilical cord mesenchymal stem cell transendothelial migration. Stem Cell Res Ther 9(1):281
Walser TC, Rifat S, Ma X et al (2006) Antagonism of CXCR3 inhibits lung metastasis in a murine model of metastatic breast cancer. Cancer Res 66(15):7701–7707
Bakheet SA, Alrwashied BS, Ansari MA et al (2020) CXC chemokine receptor 3 antagonist AMG487 shows potent anti-arthritic effects on collagen-induced arthritis by modifying B cell inflammatory profile. Immunol Lett 225:74–81
Bakheet SA, Ansari MA, Nadeem A et al (2019) CXCR3 antagonist AMG487 suppresses rheumatoid arthritis pathogenesis and progression by shifting the Th17/Treg cell balance. Cell Signal 64:109395
Mudshinge SR, Deore AB, Patil S, Bhalgat CM (2011) Nanoparticles: emerging carriers for drug delivery. Saudi Pharm J 19(3):129–141
Kumar AJ, Anumala N, Avula H (2012) Novel and often bizarre strategies in the treatment of periodontal disease. J Indian Soc Periodontol 16(1):4–10
Cui ZK, Sun JA, Baljon JJ et al (2017) Simultaneous delivery of hydrophobic small molecules and siRNA using Sterosomes to direct mesenchymal stem cell differentiation for bone repair. Acta Biomater 58:214–224
Kim S, Cui ZK, Koo B, Zheng J, Aghaloo T, Lee M (2018) Chitosan-lysozyme conjugates for enzyme-triggered hydrogel degradation in tissue engineering applications. ACS Appl Mater Interfaces 10(48):41138–41145
Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG (2010) Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol 8(6):e1000412
Hiyari S, Atti E, Camargo PM et al (2015) Heritability of periodontal bone loss in mice. J Periodontal Res 50(6):730–736
Cui ZK, Bastiat G, Jin C, Keyvanloo A, Lafleur M (2010) Influence of the nature of the sterol on the behavior of palmitic acid/sterol mixtures and their derived liposomes. Biochim Biophys Acta 1798(6):1144–1152
Hiyari S, Wong RL, Yaghsezian A et al (2018) Ligature-induced peri-implantitis and periodontitis in mice. J Clin Periodontol 45(1):89–99
Pirih FQ, Michalski MN, Cho SW et al (2010) Parathyroid hormone mediates hematopoietic cell expansion through interleukin-6. PLoS One. 5(10):e13657
Chaichanasakul T, Kang B, Bezouglaia O, Aghaloo TL, Tetradis S (2014) Diverse osteoclastogenesis of bone marrow from mandible versus long bone. J Periodontol 85(6):829–836
Bakheet SA, Alrwashied BS, Ansari MA et al (2020) CXCR3 antagonist AMG487 inhibits glucocorticoid-induced tumor necrosis factor-receptor-related protein and inflammatory mediators in CD45 expressing cells in collagen-induced arthritis mouse model. Int Immunopharmacol 84:106494
Li Q, Yang G, Li J et al (2020) Stem cell therapies for periodontal tissue regeneration: a network meta-analysis of preclinical studies. Stem Cell Res Ther 11(1):427
Vane J (1994) Towards a better aspirin. Nature 367(6460):215–216
McDonald JS, Cavanaugh PF, Pavelic LJ, Limardi RJ, Gluckman JL, Pavelic ZP (1997) Prostaglandin H synthase isoenzyme distribution in the gingival tissue of patients with periodontitis: pronounced expression adjacent to gram-positive bacteria. Inflammopharmacology 5(2):109–118
Funding
This work was supported by NIH/NIDCR DE023901-01 and the UCLA Faculty Development grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Informed consent
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lari, S., Hiyari, S., de Araújo Silva, D.N. et al. Local delivery of a CXCR3 antagonist decreases the progression of bone resorption induced by LPS injection in a murine model. Clin Oral Invest 26, 5163–5169 (2022). https://doi.org/10.1007/s00784-022-04484-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04484-z