Abstract
Objective
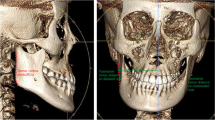
Posterior teeth intrusion is one of the best treatment options for treatment of skeletal open bite in adults; the surrounding anatomical landmarks are one of the restraining factors. This study aimed to assess the vertical relationship between the maxillary posterior teeth (MPT) and the maxillary sinus floor (MSF) in different facial growth patterns in the Chinese adult population.
Materials and methods
Cone beam computed tomography images of 298 patients, 145 males and 153 females aged between 20 and 45 years, were analyzed. Based on Jarabak ratio and the mandibular plane inclination, the sample was categorized into 94 hyperdivergent, 102 hypodivergent, and 102 normodivergent facial patterns subjects. The vertical relationship between the root-apex distances were classified as favorable, indicating no contact (type 1), or unfavorable, indicating roots in contact (type 2) for the posterior teeth intrusion. The relationship in the unfavorable group was subdivided into three subgroups (T2C, T2LC, and T2P). Comparative statistical tests were done related to age, gender, tooth side, and type of multiplanar view (sagittal and coronal). The significant level was set to be P < 0.05.
Results
There was a statistically significant difference in the mean distance between both genders in the hyperdivergent group (P < 0.001). The measured distance increased with age in all tooth roots (P < 0.001). In both sagittal and coronal views, the most frequent root scores were type 1 and type 2p (54.2%, 27.5%) and (55.1%, 21.4%), respectively. The hyperdivergent group demonstrated a higher prevalence of type 2P (31.6% and 25.5%), whereas the hypodivergent group showed a lower prevalence (25.1% and 19.2%); furthermore, the second molar’s mesiobuccal root in hyperdivergent patients showed the closest distance to the maxillary sinus in sagittal and coronal views, 0.3 ± 3.7 and 0.4 ± 3.1 mm, respectively.
Conclusions
Maxillary molars of hyperdivergent patients have the highest possible risk of root resorption due to the possible risk of cortical bone encroachment, while hypodivergent patients have the least possible risk.
Clinical relevance
Analysis of apex-sinus distances can be of great help for safe posterior teeth intrusion and providing correct and adequate treatment.



Similar content being viewed by others
References
Nurbakhsh B, Friedman S, Kulkarni GV et al (2011) Resolution of maxillary sinus mucositis after endodontic treatment of maxillary teeth with apical periodontitis: a cone-beam computed tomography pilot study. J Endod 37:1504–1511. https://doi.org/10.1016/j.joen.2011.07.007
Dobele I, Kise L, Apse P et al (2013) Radiographic assessment of findings in the maxillary sinus using cone-beam computed tomography. Stomatologija 15:119–122
Okada T, Kanai T, Tachikawa N et al (2016) Long-term radiographic assessment of maxillary sinus floor augmentation using beta-tricalcium phosphate: analysis by cone-beam computed tomography. Int J Implant Dent 2:1–9. https://doi.org/10.1186/s40729-016-0042-6
Jun B-C, Song S-W, Park C-S et al (2005) The analysis of maxillary sinus aeration according to aging process; volume assessment by 3-dimensional reconstruction by high-resolutional ct scanning. Otolaryngol Head Neck Surg 132:429–434. https://doi.org/10.1016/j.otohns.2004.11.012
Wehrbein HDiedrich PJ, (1992) The initial morphological state in the basally pneumatized maxillary sinus–a radiological-histological study in man. Fortschr Kieferorthop 53:254–262
Almaqrami B-S, Alhammadi M-SCao BJ, (2018) Three dimensional reliability analyses of currently used methods for assessment of sagittal jaw discrepancy. J clin exp dent 10:e352–e360. https://doi.org/10.4317/jced.54578
Nielsen ILJTAO (1991) Vertical malocclusions: etiology, development, diagnosis and some aspects of treatment. Angle Orthod 61:247–260. https://doi.org/10.1043/0003-3219(1991)061%3c0247:VMEDDA%3e2.0.CO;2
Alhammadi M-SJJoc, (2019) Dentoalveolar compensation in different anterioposterior and vertical skeletal malocclusions. J clin exp dent 11:e745–e753. https://doi.org/10.4317/jced.56020
Celik S, Celikoglu M, Buyuk SK et al (2016) Mandibular vertical asymmetry in adult orthodontic patients with different vertical growth patterns: a cone beam computed tomography study. Angle Orthod 86:271–277. https://doi.org/10.2319/030515-135.1
Arun T, Isik FSayinsu KJTAO, (2003) Vertical growth changes after adenoidectomy. Angle Orthod 73:146–150. https://doi.org/10.1043/0003-3219(2003)73%3c146:VGCAA%3e2.0.CO;2
Gu Y, McNamara JA Jr, Sigler LM et al (2011) Comparison of craniofacial characteristics of typical chinese and caucasian young adults. Eur J Orthod 33:205–211. https://doi.org/10.1093/ejo/cjq054
Schegerer AA, Lechel U, Ritter M et al (2014) Dose and image quality of cone-beam computed tomography as compared with conventional multislice computed tomography in abdominal imaging. Invest Radiol 49:675–684. https://doi.org/10.1097/RLI.0000000000000069
Maeda Y, Kuroda S, Ganzorig K et al (2015) Histomorphometric analysis of overloading on palatal tooth movement into the maxillary sinus. Am J Orthod Dentofacial Orthop 148:423–430. https://doi.org/10.1016/j.ajodo.2015.04.032
Pei J, Liu J, Chen Y et al (2020) Relationship between maxillary posterior molar roots and the maxillary sinus floor: cone-beam computed tomography analysis of a western chinese population. Int J Med Res 48:0300060520926896. https://doi.org/10.1177/0300060520926896
Zhang X, Li Y, Zhang Y et al (2019) Investigating the anatomical relationship between the maxillary molars and the sinus floor in a chinese population using cone-beam computed tomography. BMC Oral Health 19:1–8. https://doi.org/10.1186/s12903-019-0969-0
Gu Y, Sun C, Wu D et al (2018) Evaluation of the relationship between maxillary posterior teeth and the maxillary sinus floor using cone-beam computed tomography. BMC Oral Health 18:1–7. https://doi.org/10.1186/s12903-018-0626-z
Oishi S, Ishida Y, Matsumura T et al (2020) A cone-beam computed tomographic assessment of the proximity of the maxillary canine and posterior teeth to the maxillary sinus floor: lessons from 4778 roots. Am J Orthod Dentofacial Orthop 157:792–802. https://doi.org/10.1016/j.ajodo.2019.06.018
Haghanifar S, Moudi E, Bijani A et al (2018) Relationship between the maxillary molars roots and sinus in a selected iranian population: a cbct study. J Res Med Dent Sci 6:544–549. https://doi.org/10.5455/jrmds.20186282
Estrela C, Nunes CA, Guedes OA et al (2016) Study of anatomical relationship between posterior teeth and maxillary sinus floor in a subpopulation of the brazilian central region using cone-beam computed tomography-part 2. Braz Dent J 27:9–15. https://doi.org/10.1590/0103-6440201600679
Georgiev T, Peev SArnautska HJ (2015) Relationship between root apices of maxillary posterior teeth and the maxillary sinus floor in patients from the varna region. Med Inform 4: 30009. https://doi.org/10.18044/MedInform.201524.300
Mattar E, Hammad L, Faden A et al (2016) Relation of maxillary teeth to the maxillary sinus in normal saudi individuals living in riyadh. Biosci Biotechnol Res Asia 7:695–700
Costea M-C, Bondor C-I, Muntean A et al (2018) Proximity of the roots of posterior teeth to the maxillary sinus in different facial biotypes. Am J Orthod Dentofacial Orthop 154:346–355. https://doi.org/10.1016/j.ajodo.2018.01.006
Ahn N-LPark H-SJ (2017) Differences in distances between maxillary posterior root apices and the sinus floor according to skeletal pattern. Am J Orthod Dentofacial Orthop 152:811–819. https://doi.org/10.1016/j.ajodo.2017.05.021
Lu Y, Liu Z, Zhang L et al (2012) Associations between maxillary sinus mucosal thickening and apical periodontitis using cone-beam computed tomography scanning: a retrospective study. J Endod 38:1069–1074. https://doi.org/10.1016/j.joen.2012.04.027
Güncü GN, Yildirim YD, Wang HL et al (2011) Location of posterior superior alveolar artery and evaluation of maxillary sinus anatomy with computerized tomography: a clinical study. Clin Oral Implants Res 22:1164–1167. https://doi.org/10.1111/j.1600-0501.2010.02071.x
Alhammadi MS, Almaqrami BSCao BJ, (2019) Reliability of beta-angle in different anteroposterior and vertical combinations of malocclusions. Orthod Waves 78:111–117. https://doi.org/10.1016/j.odw.2019.02.002
Ozdemir F, Tozlu M, Germec-Cakan DJAjoo, et al (2013) Cortical bone thickness of the alveolar process measured with cone-beam computed tomography in patients with different facial types. Am J Orthod Dentofacial Orthop 143:190–196. https://doi.org/10.1016/j.ajodo.2012.09.013
Son WS, Kim YI, Kim SS et al (2020) Anatomical relationship between the maxillary posterior teeth and the sinus floor according to an anterior overbite. Orthod Craniofac Res 23:160–165. https://doi.org/10.1111/ocr.12354
Jung Y-HCho B-HJ (2012) Assessment of the relationship between the maxillary molars and adjacent structures using cone beam computed tomography. Imaging Sci Dent 42:219–224. https://doi.org/10.5624/isd.2012.42.4.219
Hodges RJ, Atchison KAWhite SCJAjoo, (2013) Impact of cone-beam computed tomography on orthodontic diagnosis and treatment planning. Am J Orthod Dentofacial Orthop 143:665–674. https://doi.org/10.1016/j.ajodo.2012.12.011
Alhammadi MS, Almashraqi AA, Halboub E, et al (2019) Pharyngeal airway spaces in different skeletal malocclusions: a cbct 3d assessment. CRANIO® 39: 97–106. https://doi.org/10.1080/08869634.2019.1583301
Hassan BAJ (2010) Reliability of periapical radiographs and orthopantomograms in detection of tooth root protrusion in the maxillary sinus: correlation results with cone beam computed tomography. J Oral Maxillofac Res 1:e6. https://doi.org/10.5037/jomr.2010.1106
Patcas R, Markic G, Müller L et al (2012) Accuracy of linear intraoral measurements using cone beam ct and multidetector ct: a tale of two cts. Dentomaxillofac Radiol 41:637–644. https://doi.org/10.1259/dmfr/21152480
Jang J, Kwak S, Ha J et al (2017) Anatomical relationship of maxillary posterior teeth with the sinus floor and buccal cortex. J Oral Rehabil 44:617–625. https://doi.org/10.1111/joor.12525
Ok E, Güngör E, Çolak M et al (2014) Evaluation of the relationship between the maxillary posterior teeth and the sinus floor using cone-beam computed tomography. Surg Radiol Anat 36:907–914. https://doi.org/10.1007/s00276-014-1317-3
Kilic C, Kamburoglu K, Yuksel SP et al (2010) An assessment of the relationship between the maxillary sinus floor and the maxillary posterior teeth root tips using dental cone-beam computerized tomography. Eur J Dent 4:462–467. https://doi.org/10.1055/s-0039-1697866
Kwak H, Park H, Yoon H et al (2004) Topographic anatomy of the inferior wall of the maxillary sinus in koreans. Int J Oral Maxillofac Surg 33:382–388. https://doi.org/10.1016/j.ijom.2003.10.012
Kim H-J, Yoon H-R, Kim K-D et al (2002) Personal-computer-based three-dimensional reconstruction and simulation of maxillary sinus. Surg Radiol Anat 24:392–398. https://doi.org/10.1007/s00276-002-0058-x
Gosau M, Rink D, Driemel O et al (2009) Maxillary sinus anatomy: a cadaveric study with clinical implications. Anat Rec Adv Integr Anat Evol Biol 292:352–354. https://doi.org/10.1002/ar.20859
Kaushik M, Kaushik P, Mehra N et al (2020) Anatomical relationship between roots of maxillary posterior teeth and maxillary sinus using cone-beam computed tomography. Endodontology 32:124–129. https://doi.org/10.4103/endo.endo_25_20
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study is supported by The Natural Foundation of Gansu Province, China (1208RJZA236), the Key Technology Plane Program of Gansu Province, China (20YF8FA071), and the Key Technology Support Program of Gansu Province, China (1604FKCA089).
Author information
Authors and Affiliations
Contributions
Conceptualization, Ehab A. Abdulghani, Abeer A. Al-Sosowa, and Maged Alhammadi and BaoCheng Cao. Data curation, Abeer A. Al-Sosowa, Abeer A. Almashreqi, Hasan M. Sharhan, and Hanan Al_fakeh.Formal analysis, Ehab A. Abdulghani. Investigation, Ehab A. Abdulghani. Methodology, Ehab A. Abdulghani and Abeer A. Almashreqi. Project administration, Ehab A. Abdulghani and BaoCheng Cao.; Resources, Ehab A. Abdulghani, and Abeer A. Al-Sosowa. Software, Ehab A. Abdulghani. Supervision, BaoCheng Cao. Validation, Ehab A. Abdulghani and Maged Alhammadi. Visualization, Ehab A. Abdulghani. Writing—original draft, Abeer A. Al-Sosowa, Abeer A. Almashreqi, Hasan M. Sharhan, and Hanan Al_fakeh. Writing—review and editing, Ehab A. Abdulghani, Maged Alhammadi, and BaoCheng Cao. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This is a retrospective cross-sectional study approved by the Institutional Ethical Committee (LZUKQ-2021–020) at the Hospital of Stomatology in Lanzhou University, China.
Informed consent
The requirement for informed consent was waived due to the retrospective nature of the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abdulghani, E.A., Alhammadi, M.S., Al-Sosowa, A.A. et al. Three-dimensional assessment of the favorability of maxillary posterior teeth intrusion in different facial patterns limited by the vertical relationship with the maxillary sinus floor. Clin Oral Invest 26, 4905–4915 (2022). https://doi.org/10.1007/s00784-022-04458-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04458-1