Abstract
Objectives
This study aims to evaluate the influence of toothache in early adolescence on oral health-related quality of life (OHRQoL) on later adolescence.
Materials and methods
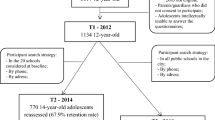
A longitudinal study was conducted, starting in 2012 within a random sample of 1,134 adolescents of 12-year-olds, in Santa Maria, Brazil. Clinical, socioeconomic, demographic, and subjective variables were obtained. Toothache was collected through the question “In the last 6 months, did you have toothache?” Six years later, the same adolescents answered the short form of the Child Perceptions Questionnaire (CPQ11–14). Multilevel Poisson regression was used to evaluate the association between toothache at baseline (2012) with overall and domain-specific CPQ11–14 scores at follow-up (2018).
Results
A total of 769 adolescents were revaluated in 2018 (68% rate retention), with a mean age of 17.5 years (SD, 0.64). Adolescents who reported toothache at the baseline presented a had a higher mean score in the overall CPQ questionnaire during follow-up (Incidence rate ratio (IRR) = 1.25; 95% CI 1.20–1.31). Toothache was also associated with all domain-specific CPQ11–14 even after adjusting the other variables.
Conclusions
Brazilian adolescents who had toothache in early adolescence, even if only a single episode, have a negative impact on OHRQoL throughout adolescence.
Clinical relevance
These findings serve as a warning for dental professionals to dedicate their preventive approaches and to promote healthy standards in this age group, in order to avoid episodes of toothache and negative impact on OHRQoL.
Similar content being viewed by others
References
World Health Organization (2015). Adolescent health research priorities: report of a technical consultation, 13th and 14th October 2015, Geneva, Switzerland (No. WHO/FWC/MCA/15/07). World Health Organization. Available from https://www.who.int/publications/i/item/WHO-FWC-MCA-15
Bundy DAP, de Silva N, Horton S, Patton GC, Schultz L, Jamison DT et al (2018) Investment in child and adolescent health and development: key messages from Disease Control Priorities, 3rd Edition. Lancet 391(10121):687–699. https://doi.org/10.1016/S0140-6736(17)32417-0
da Cunha IP, Pereira AC, Frias AC, Vieira V, de Castro MM, Batista MJ et al (2017) Social vulnerability and factors associated with oral impact on daily performance among adolescents. Health Qual Life Outcomes 15(1):1–10. https://doi.org/10.1186/s12955-017-0746-1
Slade GD (2001) Epidemiology of dental pain and dental caries among children and adolescents. Community Dent Health 18(4):219–227
Freire MCM, Nery NG, Jordão LMR, Abreu MHNG (2019) Individual and contextual determinants of dental pain in adolescents: evidence from a national survey. Oral Dis 25(5):1384–1393. https://doi.org/10.1111/odi.13100
Freire MCM, Jordão LMR, Peres MA, Abreu MHNG (2019) Six-year trends in dental pain and maternal education inequalities among Brazilian adolescents. Community Dent Oral Epidemiol 47(6):454–460. https://doi.org/10.1111/cdoe.12483
Hobdell M, Petersen PE, Clarkson J, Johnson N (2003) Global goals for oral health 2020. Int Dent J 53(5):285–288. https://doi.org/10.1111/j.1875-595x.2003.tb00761.x
Sischo L, Broder HL (2011) Oral health-related quality of life: what, why, how, and future implications. J Dent Res 90:1264. https://doi.org/10.1177/0022034511399918
Schuch HS, dos Santos CF, Torriani DD, Demarco FF, Goettems ML (2015) Oral health-related quality of life of schoolchildren: impact of clinical and psychosocial variables. Int J Paediatr Dent 25(5):358–365. https://doi.org/10.1111/ipd.12118
Bendo CB, Martins CC, Pordeus IA, Paiva SM (2014) Impact of oral conditions on individual’s quality of life. Rev Assoc Paul Cir Dent 68(3):189–193
Barasuol JC, Santos PS, Moccelini BS, Magno MB, Bolan M, Martins-Júnior PA, et al (2020) Association between dental pain and oral health-related quality of life in children and adolescents: a systematic review and meta-analysis. Community Dent Oral Epidemiol 1–7. https://doi.org/10.1111/cdoe.12535
Nicolau B, Thomson WM, Steele JG, Allison PJ (2007) Life-course epidemiology: concepts and theoretical models and its relevance to chronic oral conditions. Community Dent Oral Epidemiol 35:241–249. https://doi.org/10.1111/j.1600-0528.2007.00332.x
Kuh D, Power C, Blane D, Bartley M (1997) Social pathways between childhood and adult health. In: Kuh D, Ben-Shlomo Y (eds) A life course approach to chronic disease epidemiology. Oxford University Press, Oxford, pp 169–198
World Health Organization (1997). Oral health surveys, basic methods (4th ed). World Health Organization
Tomazoni F, Zanatta FB, Tuchtenhagen S, da Rosa GN, Del Fabro JP, Ardenghi TM (2014) Association of gingivitis with child oral health–related quality of life. J Periodontol 85(11):1557–1565. https://doi.org/10.1902/jop.2014.140026
Peres KG, Peres MA, Araujo CLP, Menezes AMB, Hallal PC (2009) Social and dental status along the life course and oral health impacts in adolescents: a population-based birth cohort. Health Qual Life Outcomes 7:1–10. https://doi.org/10.1186/1477-7525-7-95
Ministério da Saúde (2010) Pesquisa Nacional de Saúde Bucal. Ouvidoria do SUS 136 Biblioteca Virtual em Saúde do Ministério da Saúde Resultados Principais. https://bvsms.saude.gov.br/bvs/publicacoes/pesquisa_nacional_saude_bucal.pdf Accessed 08 June 2021
Torres CS, Paiva SM, Vale MP, Pordeus IA, Ramos-Jorge ML, Oliveira AC et al (2009) Psychometric properties of the Brazilian version of the Child Perceptions Questionnaire (CPQ11-14) - short forms. Health Qual Life Outcomes 7:1–7. https://doi.org/10.1186/1477-7525-7-43
Foster Page LA, Boyd D, Thomson WM (2013) Do we need more than one Child Perceptions Questionnaire for children and adolescents? BMC Oral Health 13(1):1–7. https://doi.org/10.1186/1472-6831-13-2
Kanegane K, Penha SS, Munhoz CD, Rocha RG (2009) Dental anxiety and salivary cortisol levels before dental care. J Oral Sci 51(4):515–520. https://doi.org/10.2334/josnusd.51.515
da Fonseca RCL, Antunes JLF, Cascaes AM, Bomfim RA (2020) Analysis of the combined risk of oral problems in the oral health–related quality of life of Brazilian adolescents: multilevel approach. Clin Oral Investig 24(2):857–866. https://doi.org/10.1007/s00784-019-02976-z
Ortiz FR, Tomazoni F, Dutra MMO, Piovesan C, Mendes F, Ardenghi TM (2014) Toothache, associated factors, and its impact on oral health-related quality of life (OHRQoL) in preschool children. Braz Dent J 25:546–553. https://doi.org/10.1590/0103-6440201302439
Rauber ED, Menegazzo GR, Knorst JK, Bolsson GB, Ardenghi TM (2021) Pathways between toothache and children’ oral health-related quality of life. Int J Paediatr Dent 31(5):558–564. https://doi.org/10.1111/ipd.12692
Bastos JLD, Gigante DP, Peres KG, Nedel FB (2007) Social determinants of odontalgia in epidemiological studies: theoretical review and proposed conceptual model. Cienc Saúde Coletiva 12(6):1611–1621. https://doi.org/10.1590/S1413-81232007000600022
Pakpour AH, Lin CY, Kumar S, Fridlund B, Jansson H (2018) Predictors of oral health-related quality of life in Iranian adolescents: a prospective study. J Investig Clin Dent 9(1):1–9. https://doi.org/10.1111/jicd.12264
Ortiz FR, Sfreddo CS, Coradini AGM, Fagundes MLB, Ardenghi TM (2020) Gingivitis influences oral health-related quality of life in adolescents: findings from a cohort study. Rev Bras Epidemiol 23:200051. https://doi.org/10.1590/1980-549720200051
Goettems ML, Shqair AQ, Bergmann VF, Cadermatori MG, Correa MB, Demarco FL (2018) Oral health self-perception, dental caries, and pain: the role of dental fear underlying this association. Int J Paediatr Dent 28(3):319–325. https://doi.org/10.1111/ipd.12359
Maroneze MC, Ardenghi DM, Brondani M, Unfer B, Ardenghi TM (2019) Dental treatment improves the oral health-related quality of life of adolescents: a mixed-methods approach. Int J Paediatr Dent 29(6):765–774. https://doi.org/10.1111/ipd.12548
Crocombe LA, Brennan DS, Slade GD (2012) The influence of dental attendance on change in oral health–related quality of life. Community Dent Oral Epidemiol 40(1):53–61. https://doi.org/10.1111/j.1600-0528.2011.00634.x
Huguet A, Stinson JN, Mcgrath PJ (2010) Measurement of self-reported pain intensity in children and adolescents. J Psychosom Res 68(4):329–336. https://doi.org/10.1016/j.jpsychores.2009.06.003
Moghaddam LF, Vettore MV, Bayani A, Bayat AH, Ahounbar E, Hemmat M, Fakhri Y (2020) The association of oral health status, demographic characteristics and socioeconomic determinants with oral health-related quality of life among children: a systematic review and meta-analysis. BMC Pediatr 20(1):1–15. https://doi.org/10.1186/s12887-020-02371-8
Acknowledgements
The authors thank all the schools and adolescents who participated in this study, the members of the Epidemiology Group who contributed to the data collection, and the Municipal Education Authorities of Santa Maria for their collaboration in this study.
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) (Finance Code 001) and the Fundação de Amparo à Pesquisa do Rio Grande do Sul (FAPERGS: 2381–2551/14–0).
Author information
Authors and Affiliations
Contributions
AWV led the article writing and participated in the data collection, MCM and FRO participated in the data collection and performed the data analysis of the article, and DMA participated on the writing and analysis of the article. TMA conceived the idea of the project and the article and coordinated and supervised the data collection. All authors critically reviewed the article, were important for its preparation, and agreed with its final version.
Corresponding author
Ethics declarations
Ethics approval
The study protocol was approved by the Committee of Ethics in Research of University (CAAE 2012, 0127.0.243.000–11, and CAAE 2018, 66553117.4.0000.5346).
Consent to participate
All the adolescents consented to participate, and their parents (either the mother or father) signed a term of consent before the data collection.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vargas, A.W., Maroneze, M.C., Ortiz, F.R. et al. Influence of toothache on oral health-related quality of life during adolescence: a cohort study. Clin Oral Invest 26, 4615–4622 (2022). https://doi.org/10.1007/s00784-022-04430-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04430-z