Abstract
Objectives
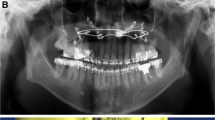
This study aimed to investigate the mandibular canal of ramus and design a suitable osteotomy line for intraoral vertical ramus osteotomy (IVRO) using cone-beam computed tomography (CBCT).
Materials and methods
Ninety patients were classified into class I, II, and III skeletal pattern groups. When extended from the horizontal base plane (0 mm, mandibular foramen [MF]), with a 2-mm section interval, to 10 mm above and 10 mm below the MF, the following landmarks were identified: external oblique ridge (EOR), posterior border of the ramus (PBR), and posterior lateral cortex of ramus (PLC): IVRO osteotomy point.
Results
In the base plane (0-mm plane), the EOR-PBR distance of class III (34.78 mm) and the IOR-PBR distance of class II (32.72 mm) were significantly higher than those of class I (32.95 mm and 30.03 mm). Compared to the EOR-PLC distance, the designed osteotomy point (two-thirds EOR-PBR length) has a 3.49-mm safe zone at the base plane and ranging from 0.89 mm (+ 10-mm plane) to 8.37 mm (− 10-mm plane).
Conclusions
The position at two-thirds EOR-PBR length (anteroposterior diameter of the ramus) can serve as a reference distance for the IVRO osteotomy position.
Clinical relevance
Mandibular setback operations for treating mandibular prognathism mainly include sagittal split ramus osteotomy (SSRO) and IVRO. IVRO has a markedly lower incidence of postoperative lower lip paraesthesia than SSRO. Our design presented a reference point for identification during IVRO, to prevent damage to the inferior alveolar neurovascular bundle.







Similar content being viewed by others
References
Rude K, Svensson P, Starch-Jensen T (2019) Neurosensory disturbances after bilateral sagittal split osteotomy using piezoelectric surgery: a systematic review. J Oral Maxillofac Surg 77:380–390
McLeod NM, Bowe DC (2016) Nerve injury associated with orthognathic surgery. Br J Oral Maxillofac Surg 54:366–371
Gennaro P, Giovannoni ME, Pini N et al (2017) Relationship between the quantity of nerve exposure during bilateral sagittal split osteotomy surgery and sensitive recovery. J Craniofac Surg 28:1375–1379
Politis C, Sun Y, Lambrichts I, Agbaje JO (2013) Self-reported hypoesthesia of the lower lip after sagittal split osteotomy. Int J Oral Maxillofac Surg 42:823–829
Karas ND, Boyd SB, Sinn DP (1990) Recovery of neurosensory function following orthognathic surgery. J Oral Maxillofac Surg 48:124–134
Westermark A, Bystedt H, von Konow L (1998) Inferior alveolar nerve function after mandibular osteotomies. Br J Oral Maxillofac Surg 36:425–428
Chen CM, Lai S, Chen KK, Lee HE (2015) Intraoperative hemorrhage and postoperative sequelae after intraoral vertical ramus osteotomy to treat mandibular prognathism. Biomed Res Int 2015:318270
Hogan G, Ellis E 3rd (2006) The “Antilingula”—Fact or Fiction? J Oral Maxillofac Surg 64:1248–1254
Aziz SR, Dorfman BJ, Ziccardi VB, Janal M (2007) Accuracy of using the antilingula as a sole determinant of vertical ramus osteotomy position. J Oral Maxillofac Surg 65:859–862
Park JH, Jung HD, Kim HJ, Jung YS (2018) Anatomical study of the location of the antilingula, lingula, and mandibular foramen for vertical ramus osteotomy. Maxillofac Plast Reconstr Surg 40:15
Farrell BB, Franco PB, Tucker MR (2014) Virtual surgical planning in orthognathic surgery. Oral Maxillofac Surg Clin North Am 26:459–473
Lai SS, Tseng YC, Huang IY, Yang YH, Shen YS, Chen CM (2007) Skeletal changes after modified intraoral vertical ramus osteotomy for correction of mandibular prognathism. J Plast Reconstr Aesthet Surg 60:139–145
Pogrel MA, Schmidt BL, Ammar A (1995) The presence of the antilingula and its relationship to the true lingula. Br J Oral Maxillofac Surg 33:235–328
Caldwell JB, Letterman GS (1954) Vertical osteotomy in the mandibular rami for correction of prognathism. J Oral Surg 12:185–202
Gabriel AC (1958) Some anatomical features of the mandible. J Anat 92:580
Hall HD, McKenna SJ (1987) Further refinement and evaluation of intraoral vertical ramus osteotomy. J Oral Maxillofac Surg 45:684–688
Monnazzi MS, Passeri LA, Gabrielli MF, Bolini PD, de Carvalho WR, da Costa MH (2012) Anatomic study of the mandibular foramen, lingula and antilingula in dry mandibles, and its statistical relationship between the true lingula and the antilingula. Int J Oral Maxillofac Surg 41:74–78
Ueki K, Okabe K, Miyazaki M et al (2010) Position of mandibular canal and ramus morphology before and after sagittal split ramus osteotomy. J Oral Maxillofac Surg 68:1795–1801
McKenna SJ, King EE (2016) Intraoral vertical ramus osteotomy procedure and technique. Atlas Oral Maxillofac Surg Clin N Am 24:37–43
Sekerci AE, Sisman Y (2014) Cone-beam computed tomography analysis of the shape, height, and location of the mandibular lingula. Surg Radiol Anat 36:155–162
Hsu KJ, Tseng YC, Liang SW, Hsiao SY, Chen CM (2020) Dimension and location of the mandibular lingula: comparisons of gender and skeletal patterns using cone-beam computed tomography. Biomed Res Int 2020:2571534
Chrcanovic BR, de Carvalho MV, Gjelvold B (2016) A morphometric analysis of the mandibular canal by cone beam computed tomography and its relevance to the sagittal split ramus osteotomy. Oral Maxillofac Surg 20:183–190
Hibi H, Ueda M (1995) A technique for ensuring accurate bone cuts in the intraoral vertical ramus osteotomy. J Oral Maxillofac Surg 53:1480–1481
Tominaga K, Yoshioka I, Nakahara T, Fukuda J (2002) A simple technique to avoid the mandibular nerve in intraoral vertical ramus osteotomy. J Oral Maxillofac Surg 60:1089–1091
Eggensperger N, Smolka W, Rahal A, Iizuka T (2004) Skeletal relapse after mandibular advancement and setback in single-jaw surgery. J Oral Maxillofac Surg 62:1486–1496
Lee YS, Kim YK, Yun PY, Larson BE, Lee NK (2016) Comparison of the stability after mandibular setback with minimal orthodontics of class III patients with different facial types. J Oral Maxillofac Surg 74:1464.e1-1464.e10
Tseng YC, Cheng JH, Chen MY, Chen KJ, Chen CM (2018) The changes of cheek line (lateral) and face line (frontal) after correction of mandibular prognathism. Biomed Res Int 2018:4926528
Acknowledgements
The authors would like to thank Ying-Chun Lin, assistant research fellow, of the Department of Dentistry, Kaohsiung Medical University Hospital for editing assistance.
Funding
The present study was funded by the authors’ own institution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The retrospective study was approved by the Institutional Review Board of Kaohsiung Medical University Hospital, Taiwan (KMUH-IRB 20160066).
Informed consent
Informed consent signed by the patients was waived because of the observational nature of the study and the anonymity and deidentification of personal information before data analysis.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, CM., Hsu, HJ., Liang, SW. et al. Two-thirds anteroposterior ramus length is the preferred osteotomy point for intraoral vertical ramus osteotomy. Clin Oral Invest 26, 1229–1239 (2022). https://doi.org/10.1007/s00784-021-04094-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04094-1