Abstract
Objectives
Microsurgical principles, techniques, and armamentarium have made significant contributions to the periodontal plastic surgery. The present meta-analysis aimed to investigate the overall efficacy of microsurgery on root coverage, and its clinical outcomes when compared to traditional macrosurgery.
Material and methods
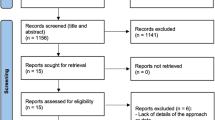
Electronic searches on PubMed, Embase, and CINAHL were used to retrieve prospective clinical trials. Primary outcomes were the mean root coverage (mRC) and probability of achieving complete root coverage (cRC), with secondary outcomes as other periodontal parameters and patient-reported outcome measures (PROMs).
Results
Nineteen studies were included in the quantitative analysis. Microsurgery was estimated to achieve 83.3% mRC and 69.3% cRC. From a subgroup of 9 comparative studies, it was estimated microsurgery increased mRC by 6.6% (p<0.001) and cRC by 27.9% (p<0.01) compared to macrosurgical control treatments. Operating microscope (OM) yielded a significantly 6.7% higher mRC than the control group (p=0.002), while using loupes showed 6.16% increase in mRC with a borderline significance (p=0.09). OM and loupes-only had a 31.05% (p=0.001) and 25.54% (p=0.001) increases in achieving cRC compared to control, respectively. As for PROMs, microsurgery reduced postoperative pain (p<0.001) and enhanced esthetics (p= 0.05).
Conclusions
Microsurgery significantly improved mean root coverage, probability of achieving complete root coverage, esthetics, and post-surgical recovery. Microsurgery enhances not only subclinical healing but also clinical outcomes, possibly owing to its minimally invasive approach and surgical precision.
Clinical relevance
Periodontal plastic microsurgery is minimally invasive, inducing less surgical trauma and ultimately resulting in improved clinical outcomes, patient’s satisfaction, and quality of life.






Similar content being viewed by others
References
Cortellini P, Bissada NF (2018) Mucogingival conditions in the natural dentition: narrative review, case definitions, and diagnostic considerations. J Periodontol 89(Suppl 1):S204–S213. https://doi.org/10.1002/JPER.16-0671
Pini Prato G, Di Gianfilippo R (2020) On the value of the 2017 classification of phenotype and gingival recessions. J Periodontol. https://doi.org/10.1002/JPER.20-0487
Nieri M, Pini Prato GP, Giani M, Magnani N, Pagliaro U, Rotundo R (2013) Patient perceptions of buccal gingival recessions and requests for treatment. J Clin Periodontol 40(7):707–712. https://doi.org/10.1111/jcpe.12114
Rios FS, Costa RS, Moura MS, Jardim JJ, Maltz M, Haas AN (2014) Estimates and multivariable risk assessment of gingival recession in the population of adults from Porto Alegre, Brazil. J Clin Periodontol 41(11):1098–1107. https://doi.org/10.1111/jcpe.12303
Chambrone L, Salinas Ortega MA, Sukekava F, Rotundo R, Kalemaj Z, Buti J, Pini Prato GP (2018) Root coverage procedures for treating localised and multiple recession-type defects. Cochrane Database Syst Rev 10:CD007161. https://doi.org/10.1002/14651858.CD007161.pub3
Tavelli L, Barootchi S, Di Gianfilippo R, Modarressi M, Cairo F, Rasperini G, Wang HL (2019) Acellular dermal matrix and coronally advanced flap or tunnel technique in the treatment of multiple adjacent gingival recessions. A 12-year follow-up from a randomized clinical trial. J Clin Periodontol 46(9):937–948. https://doi.org/10.1111/jcpe.13163
Barootchi S, Tavelli L, Di Gianfilippo R, Byun HY, Oh TJ, Barbato L, Cairo F, Wang HL (2019) Long term assessment of root coverage stability using connective tissue graft with or without an epithelial collar for gingival recession treatment. A 12-year follow-up from a randomized clinical trial. J Clin Periodontol 46(11):1124–1133. https://doi.org/10.1111/jcpe.13187
Pini Prato G, Franceschi D, Cortellini P, Chambrone L (2018) Long-term evaluation (20 years) of the outcomes of subepithelial connective tissue graft plus coronally advanced flap in the treatment of maxillary single recession-type defects. J Periodontol 89(11):1290–1299. https://doi.org/10.1002/JPER.17-0619
Tavelli L, Barootchi S, Cairo F, Rasperini G, Shedden K, Wang HL (2019) The effect of time on root coverage outcomes: a network meta-analysis. J Dent Res 98(11):1195–1203. https://doi.org/10.1177/0022034519867071
Chambrone L, Pini Prato GP (2019) Clinical insights about the evolution of root coverage procedures: the flap, the graft, and the surgery. J Periodontol 90(1):9–15. https://doi.org/10.1002/JPER.18-0281
Daniel RK (1979) Microsurgery: through the looking glass. N Engl J Med 300(22):1251–1257. https://doi.org/10.1056/NEJM197905313002205
Sitbon Y, Attathom T, St-Georges AJ (2014) Minimal intervention dentistry II: part 1. Contribution of the operating microscope to dentistry. Br Dent J 216(3):125–130. https://doi.org/10.1038/sj.bdj.2014.48
Carr GB (1992) Microscopes in endodontics. J Calif Dent Assoc 20(11):55–61
Shanelec DA (2000) Tibbetts LS (1996) A perspective on the future of periodontal microsurgery. Periodontol 11:58–64. https://doi.org/10.1111/j.1600-0757.1996.tb00183.x
Burkhardt R, Lang NP (2005) Coverage of localized gingival recessions: comparison of micro- and macrosurgical techniques. J Clin Periodontol 32(3):287–293. https://doi.org/10.1111/j.1600-051X.2005.00660.x
Cairo F, Pini-Prato GP (2010) A technique to identify and reconstruct the cementoenamel junction level using combined periodontal and restorative treatment of gingival recession. A prospective clinical study. Int J Periodontics Restorative Dent 30(6):573–581
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Higgins J, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods G, Cochrane Statistical Methods G (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Munn Z, Barker TH, Moola S, Tufanaru C, Stern C, McArthur A, Stephenson M, Aromataris E (2019) Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Database System Rev Implement Rep. https://doi.org/10.11124/JBISRIR-D-19-00099
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, Welch V (2019) Cochrane handbook for systematic reviews of interventions version 6.0
Higgins J, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Follmann D, Elliott P, Suh I, Cutler J (1992) Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol 45(7):769–773. https://doi.org/10.1016/0895-4356(92)90054-q
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629
Cairo F, Mervelt J, Cincinelli S, Franceschi D, Rotundo R, Pini Prato G (2010) The use of operative microscope in periodontal plastic surgery. Journal de Parodontologie & d’Implantologie Orale 9(4)
Thankkappan P, Roy S, Mandlik VB (2016) Comparative evaluation of management of gingival recession using subepithelial connective tissue graft and collagen membrane by periodontal microsurgical technique: a clinical study of 40 cases. J Indian Soc Periodontol 20(2):189–194. https://doi.org/10.4103/0972-124X.176394
Cortellini P, Tonetti M, Prato GP (2012) The partly epithelialized free gingival graft (pe-fgg) at lower incisors. A pilot study with implications for alignment of the mucogingival junction. J Clin Periodontol 39(7):674–680. https://doi.org/10.1111/j.1600-051X.2012.01896.x
Francetti L, Del Fabbro M, Testori T, Weinstein RL (2004) Periodontal microsurgery: report of 16 cases consecutively treated by the free rotated papilla autograft technique combined with the coronally advanced flap. Int J Periodontics Restorative Dent 24(3):272–279
Latha TA, Sudarsan S, Arun KV, Talwar A (2009) Root coverage in class I gingival recession defects, combining rotated papillary pedicle graft and coronally repositioned flap, using a micro surgical approach: a clinical evaluation. J Indian Soc Periodontol 13(1):21–26. https://doi.org/10.4103/0972-124X.51890
Agarwal SK, Jhingran R, Bains VK, Srivastava R, Madan R, Rizvi I (2016) Patient-centered evaluation of microsurgical management of gingival recession using coronally advanced flap with platelet-rich fibrin or amnion membrane: a comparative analysis. Eur J Dent 10(1):121–133. https://doi.org/10.4103/1305-7456.175686
Azaripour A, Kissinger M, Farina VS, Van Noorden CJ, Gerhold-Ay A, Willershausen B, Cortellini P (2016) Root coverage with connective tissue graft associated with coronally advanced flap or tunnel technique: a randomized, double-blind, mono-centre clinical trial. J Clin Periodontol 43(12):1142–1150. https://doi.org/10.1111/jcpe.12627
Kaval B, Renaud DE, Scott DA, Buduneli N (2014) The role of smoking and gingival crevicular fluid markers on coronally advanced flap outcomes. J Periodontol 85(3):395–405. https://doi.org/10.1902/jop.2013.120685
Kumar A, Bains VK, Jhingran R, Srivastava R, Madan R, Rizvi I (2017) Patient-centered microsurgical management of gingival recession using coronally advanced flap with either platelet-rich fibrin or connective tissue graft: a comparative analysis. Contemp Clin Dent 8(2):293–304. https://doi.org/10.4103/ccd.ccd_70_17
Andrade PF, Grisi MF, Marcaccini AM, Fernandes PG, Reino DM, Souza SL, Taba M, Palioto DB, Novaes AB (2010) Comparison between micro- and macrosurgical techniques for the treatment of localized gingival recessions using coronally positioned flaps and enamel matrix derivative. J Periodontol 81(11):1572–1579. https://doi.org/10.1902/jop.2010.100155
Bittencourt S, Del Peloso RE, Sallum EA, Nociti FH Jr, Casati MZ (2012) Surgical microscope may enhance root coverage with subepithelial connective tissue graft: a randomized-controlled clinical trial. J Periodontol 83(6):721–730. https://doi.org/10.1902/jop.2011.110202
Francetti L, Del Fabbro M, Calace S, Testori T, Weinstein RL (2005) Microsurgical treatment of gingival recession: a controlled clinical study. Int J Periodontics Restorative Dent 25(2):181–188
Nizam N, Bengisu O, Sonmez S (2015) Micro- and macrosurgical techniques in the coverage of gingival recession using connective tissue graft: 2 years follow-up. J Esthet Restor Dent 27(2):71–83. https://doi.org/10.1111/jerd.12124
Ucak O, Ozcan M, Seydaoglu G, Haytac MC (2017) Microsurgical instruments in laterally moved, coronally advanced flap for Miller Class III isolated recession defects: a randomized controlled clinical trial. Int J Periodontics Restorative Dent 37(1):109–115. https://doi.org/10.11607/prd.2547
Gumus P, Buduneli E (2014) Graft stabilization with cyanoacrylate decreases shrinkage of free gingival grafts. Aust Dent J 59(1):57–64. https://doi.org/10.1111/adj.12149
Patel C, Mehta R, Joshi S, Hirani T, Joshi C (2018) Comparative evaluation of treatment of localized gingival recessions with coronally advanced flap using microsurgical and conventional techniques. Contemp Clin Dent 9(4):613–618. https://doi.org/10.4103/ccd.ccd_571_18
Pandey S, Mehta DS (2013) Treatment of localized gingival recession using the free rotated papilla autograft combined with coronally advanced flap by conventional (macrosurgery) and surgery under magnification (microsurgical) technique: a comparative clinical study. J Indian Soc Periodontol 17(6):765–770. https://doi.org/10.4103/0972-124x.124500
Askar H, Di Gianfilippo R, Ravida A, Tattan M, Majzoub J, Wang HL (2019) Incidence and severity of postoperative complications following oral, periodontal, and implant surgeries: a retrospective study. J Periodontol 90(11):1270–1278. https://doi.org/10.1002/JPER.18-0658
Aslan S, Buduneli N, Cortellini P (2017) Entire papilla preservation technique in the regenerative treatment of deep intrabony defects: 1-year results. J Clin Periodontol 44(9):926–932. https://doi.org/10.1111/jcpe.12780
Cortellini P, Tonetti MS (2009) Improved wound stability with a modified minimally invasive surgical technique in the regenerative treatment of isolated interdental intrabony defects. J Clin Periodontol 36(2):157–163. https://doi.org/10.1111/j.1600-051X.2008.01352.x
Pini Prato G, Di Gianfilippo R, Wang H-L (2019) Success in periodontology: an evolutive concept. J Clin Periodontol 46(8):840–845. https://doi.org/10.1111/jcpe.13150
Tibbetts LS, Shanelec DA (2007) A review of the principles and practice of periodontal microsurgery. Texas dental journal 124(2):188–204
Acknowledgements
The authors would like to thank Mark MacEachern (markmac@umich.edu; Research & Informatics, Taubman Health Sciences Library, University of Michigan. Ann Arbor, MI, USA) for his supervision on the selection of the controlled vocabularies of the search strategy.
Funding
Drs. H-L Chan and D. Velasquez have received educational funds from Zeiss. No funding was actively pursued for conducting of this study.
Author information
Authors and Affiliations
Contributions
All the authors provided significant contribution to the study. RDG: study design, screening, data extraction, data interpretation, writing. IW: study design, data extraction, statistical analysis, writing. LS: screening, data extraction, writing. DV: study design, data interpretation, writing. HLW: study design, data interpretation, writing. HLC: study design, data interpretation, writing. All the authors approved the last version of the study before submission and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Figure 1:
MeSH terms, key words and Boolean operators were used to conduct electronic searches on Pubmed, Embase and CINAHL databases. MeSH terms were selected based on the controlled vocabularies of the specific databases. Last update was May 10th, 2020. (PDF 62 kb)
Supplementary Figure 2:
Sensitivity test for the mean root coverage of trials comparing micro- and macrosurgery. (PNG 454 kb)
Supplementary Figure 3:
Sensitivity test for complete root coverage reported in trials comparing micro- and macrosurgery. (PNG 329 kb)
Supplementary Figure 4:
Meta-analysis results on keratinized tissue width increase for studies comparing micro- and macrosurgery. (PNG 387 kb)
Supplementary Figure 5:
Meta-analysis results on surgical time in minutes for a subgroup of the four studies comparing micro- and macrosurgery. (PNG 259 kb)
Supplementary Figure 6:
Meta-analysis results on the visual analogue scale for pain perception at 3 and 7 postoperative days, comparing micro- and macrosurgery. (PNG 325 kb)
Supplementary Figure 7:
Meta-analysis results on visual analogue scale for the esthetic outcomes, comparing micro- and macrosurgery. (PNG 205 kb)
Supplementary Table 1:
Assessment of quality and risk of bias for the studies comparing microsurgical vs. macrosurgical approach. Each domain was ranked based on high, low, or not assessable (N/A) risk of bias according to the Cochrane Collaboration's tool for assessing risk of bias. (DOCX 16 kb)
Supplementary Table 2:
Assessment of quality and risk of bias for the studies reporting on magnified/microsurgical procedures without non-magnified control patients. Each domain was satisfied (yes), not satisfied (no), or not assessable (N/A) according to the Joanna Briggs Institute Critical Appraisal tool. (DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Di Gianfilippo, R., Wang, IC., Steigmann, L. et al. Efficacy of microsurgery and comparison to macrosurgery for gingival recession treatment: a systematic review with meta-analysis. Clin Oral Invest 25, 4269–4280 (2021). https://doi.org/10.1007/s00784-021-03954-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03954-0