Abstract
Objectives
To evaluate and compare the efficacy of prepared propolis mouth rinse with Chlorhexidine mouthwash on oral pathogens and also the plaque and gingival index scores.
Material and methods
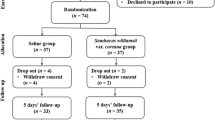
A triple-blind, concurrent parallel randomized controlled trial was conducted on 120 participants randomized to 4 mouth rinse study groups: (1) Hot Ethanolic Propolis extract; (2) Cold Ethanolic Propolis extract; (3) Chlorhexidine and (4) Distilled water. After a washout period of two weeks, oral prophylaxis and polishing was performed. Participants rinsed twice a day for 3 months. Saliva was collected at baseline, 5 min and 1 h for microbiological analysis. Plaque and Gingival index were recorded at baseline, 15 days, 1 month and 3 months. Repeated measures ANOVA with Bonferroni post hoc tests were used for statistical analysis.
Results
A decline in the concentration of S. mutans was observed in samples collected after the use of mouth rinse (p < 0.05). In comparison with baseline, L. acidophilus and S. mutans count decreased simultaneously when exposed to Hot Ethanolic mouthwash group (5.5 × 102) and Chlorhexidine mouthwash (5.8 × 102) respectively. At the end of 3 months, similar reduction in plaque scores was found in Chlorhexidine (0.45), Cold Ethanolic (0.46), Hot Ethanolic (0.47) mouthwash groups.
Conclusion
Propolis was found to be as efficient as Chlorhexidine in reducing plaque, gingivitis and dental caries pathogens.
Clinical relevance
Common microorganisms implicated in oral disease are S. mutans and L. acidophilus. There is great paucity of information on antimicrobial activity of propolis, against these microorganisms. Hence, the present study has been taken up to assess the effects of propolis on these oral pathogens.The effects of propolis on oral health have been proved which is obviously a new finding of significance.
Similar content being viewed by others
References
George J, Hegde S, Rajesh KS, Kumar A (2009) The efficacy of a herbal-based toothpaste in the control of plaque and gingivitis: a clinico-biochemical study. Indian J Dent Res 20(4):480–482
Pannuti CM, Mattos JP, Ranoya PN, Jesus AM, Lotufo RF, Romito GA (2003) Clinical effect of a herbal dentifrice on the control of plaque and gingivitis: a double-blind study. Pesqui Odontol Bras 17(4):314–318
Park YK, Alencar SM, Aguiar (2002) Botanical origin and chemical composition of Brazilian propolis. J Agric Food Chem 50(9):2502–2506
Paroliya A, Thomas MS, Kundabala M, Mohan M (2010) Propolis and its potential uses in oral health. Int J Med Med Sci 2(7):210–215
Koo H, Rosalen PL, Cury JA, Park YK, Bowen WH (2002) Effects of compounds found in propolis on Streptococcus mutans growth and on glucosyltransferase activity. Antimicrob Agents Chemother 46(5):1302–1309
Ophori EA, Eriagbonye BN, Ugbodaga P (2010) Antimicrobial activity of propolis against Streptococcus mutans. Afr J Bio 9(31):4966–4969
Bascones A, Morante S, Mateos L, Mata M, Poblet J (2005) Influence of additional active ingredients on the effectiveness of non-alcoholic chlorhexidine mouthwashes: a randomized controlled trial. J Periodontol 76(9):1469–1475
Nazeri R, Ghaiour M, Abbasi S (2019) Evaluation of antibacterial effect of propolis and its application in mouthwash production. Front Dent 16(1):1–12
Daugsch A, Moraes CS, Fort P, Park YK (2008) Brazilian red propolis—chemical composition and botanical origin. Evid Based Complement Alternat Med 5(4):435–441
Ozan F, Sümer Z, Polat ZA, Er K, Ozan U, Deger O (2007) Effect of mouthrinse containing propolis on oral microorganisms and human gingival fibroblasts. Eur J Dent 1(4):195–201
Löe H, Silness P (1963) Periodontal disease in pregnancy I. Acta Odontol Scand 21:533–551
Silness P, Löe H (1964) Periodontal disease in pregnancy II. Acta Odontol Scand 22:121–126
Bowen WH, Burne RA, Wu H, Koo H (2018) Oral biofilms: pathogens, matrix, and polymicrobial interactions in microenvironments. Trends Microbiol 26(3):229–242
Drago L, Mombelli B, De Vecchi E, Fassina MC, Tocalli L, Gismondo MR (2000) In vitro antimicrobial activity of propolis dry extract. J Chemother 12(5):390–395
Sforcin JM (2016) Biological properties and therapeutic applications of propolis. Phytother Res 30(6):894–905
Wagh VD, Borkar RD (2012) Indian propolis: a potential natural antimicrobial and antifungal agent. Int J Pharm Pharm Sci 4(4):12–17
Sforcin JM, Fernandes A Jr, Lopes CA, Bankova V, Funari SR (2000) Seasonal effect on Brazilian propolis antibacterial activity. J Ethnopharmacol 73(1-2):243–249
Bankova VS, de Castro SL, Marcucci MC (2000) Propolis: recent advances in chemistry and plant origin. Apidologie 31(1):3–15
Ncube NS, Afolayan AJ, Okoh AI (2008) Assessment techniques of antimicrobial properties of natural compounds of plant origin: current methods and future trends. Afr J Biotechnol 7(12):1797–1806
Hidaka S, Okamoto Y, Ishiyama K, Hashimoto K (2008) Inhibition of the formation of oral calcium phosphate precipitates: the possible effects of certain honeybee products. J Periodontal Res 43(4):450–458
Ansorge S, Reinhold D, Lendeckel U (2003) Propolis and some of its constituents down-regulate DNA synthesis and inflammatory cytokine production but induce TGF-beta1 production of human immune cells. Z Naturforsch C J Biosci 58(7-8):580–589
Silva BB, Rosalen PL, Cury JA, Ikegaki M, Souza VC, Esteves A, Alencar SM (2008) Chemical composition and botanical origin of red propolis, a new type of Brazilian propolis. Evid Based Complement Alternat Med 5(3):313–316
Trusheva B, Trunkova D, Bankova V (2007) Different extraction methods of biologically active components from propolis: a preliminary study. Chem Cent J 1:13
Anauate-Netto C, Anido-Anido A, Leegoy HR, Matsumoto R, Alonso RC, Marcucci MC, Paulino N, Bretz WA (2014) Randomized, double-blind, placebocontrolled clinical trial on the effects of propolis and chlorhexidine mouthrinses on gingivitis. Braz Dent Sci 17(1):11–15
Ozan F, Polat ZA, Er K, Ozan U, Deger O (2007) Effect of propolis on survival of periodontal ligament cells: new storage media for avulsed teeth. J Endod 33(5):570–573
Ozaki F, Pannuti CM, Imbronito AV, Pessotti W, Saraiva L, de Freitas NM, Ferrari G, Cabral VN (2006) Efficacy of a herbal toothpaste on patients with established gingivitis — a randomized controlled trial. Braz Oral Res 20(2):172–177
Hayacibara MF, Koo H, Rosalen PL, Duarte S, Franco EM, Bowen WH, Ikegaki M, Cury JA (2005) In vitro and in vivo effects of isolated fractions of Brazilian propolis on caries development. J Ethnopharmacol 101(1-3):110–111
Acknowledgements
The authors would like to thank the study participants and their parents for their participation and kind cooperation throughout the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author SB declares that he has no conflict of interest. Author RN declares that he has no conflict of interest. Author GR declares that she has no conflict of interest. Author KB declares that she has no conflict of interest.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bapat, S., Nagarajappa, R., Ramesh, G. et al. Effect of propolis mouth rinse on oral microorganisms — a randomized controlled trial. Clin Oral Invest 25, 6139–6146 (2021). https://doi.org/10.1007/s00784-021-03913-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03913-9