Abstract
Objective
Subgingival dental restorations and periodontal health have been studied for many years; however, there is a low histological evidence on the behavior of new materials in the supracrestal tissue attachment. The aim of this study is to analyze the periodontal response when a tricalcium silicate material (TSM) or composite margin restorations is placed to 0.5 mm and 1.5 mm from the bone crest with a histomorphometric analysis in dogs.
Methods
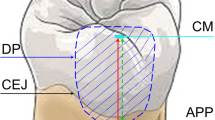
Nine mongrel dogs were used in this study: four dogs (8 canine teeth) for TSM group, 4 dogs (8 canine teeth) for composite group, and 1 dog (2 canine teeth) with cavities without restorations. Cavity preparation of 2×2×1 mm was created on the buccal aspect of the canines at 0.5 and 1.5 mm of the crestal bone. Cavities were restored with composite and TSM or were left unrestored as control. After 12 weeks of healing, the dogs were euthanized and blocks containing the tooth and soft tissues were processed.
Results
In all the specimens, the junction epithelium was stablished apical to the tooth preparations. A shorter distance to the bone (0.5 cavity) implies greater apical periodontal migration regardless of the material used. In the TSM groups, the connective tissue height and the distance between bone level and apical margin preparation were greater than those in the composite groups, while the epithelium height was less. However, there were no statistically significant differences comparing TSM and composite groups at either 0.5 mm or 1.5 mm (p > 0.05).
Conclusion
Histologic analysis did not show periodontal reattachment to TSM or composite. In both cases, bone crest migrates apically. For that reason, it is recommended to perform composite restorations at the subgingival level whenever the distance to the bone crest is at least 2 mm.
Clinical relevance
Both composite and TSM do not achieve reinsertion of the connective tissue in the biological width.









Similar content being viewed by others
References
Padbury A Jr, Eber R, Wang HL (2003) Interactions between the gingiva and the margin of restorations. J Clin Periodontol 30(5):379–385. https://doi.org/10.1034/j.1600-051x.2003.01277.x
Santamaria MP, Suaid FF, Carvalho MD, Nociti FH, Casati MZ, Sallum AW, Sallum EA (2013) Healing patterns after subgingival placement of a resin-modified glass-ionomer restoration: a histometric study in dogs. Int J Periodontics Restor Dent 33:679–687. https://doi.org/10.11607/prd.0396
Gargiulo AW, Wentz FM, Orban B (1961) Dimensions and relations of the dentogingival junction in humans. J Periodontol 32:261–267. https://doi.org/10.1902/jop.1961.32.3.261
Jepsen S, Caton JG, Albandar JM, Bissada NF, Bouchard P, Cortellini P, Demirel K, de Sanctis M, Ercoli C, Fan J, Geurs NC, Hughes FJ, Jin L, Kantarci A, Lalla E, Madianos PN, Matthews D, McGuire MK, Mills MP, Preshaw PM, Reynolds MA, Sculean A, Susin C, West NX, Yamazaki K (2018) Periodontal manifestations of systemic diseases and developmental and acquired conditions: Consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol 45(Suppl 20):S219–S229. https://doi.org/10.1111/jcpe.12951
Schmidt JC, Sahrmann P, Weiger R, Schmidlin PR, Walter C (2013) Biologic width dimensions--a systematic review. J Clin Periodontol 40(5):493–504. https://doi.org/10.1111/jcpe.12078
Ercoli C, Caton JG (2018) Dental prostheses and tooth-related factors. J Periodontol 89(Suppl 1):S223–S236. https://doi.org/10.1002/JPER.16-0569
Newcomb GM (1974) The relationship between the location of subgingival crown margins and gingival inflammation. J Periodontol 45(3):151–154. https://doi.org/10.1902/jop.1974.45.3.151
Carnevale G, Sterrantino SF, Di Febo G (1983) Soft and hard tissue wound healing following tooth preparation to the alveolar crest. Int J Periodontics Restorative Dent 3:36–53
Schatzle M, Land NP, Anerud A, Boysen H, Burgin W, Loe H (2001) The influence of margins of restorations of the periodontal tissues over 26 years. J Clin Periodontol 28(1):57–64. https://doi.org/10.1034/j.1600-051x.2001.280109.x
Sarfati A, Tirlet G (2018) Deep margin elevation versus crown lengthening: biologic width revisited. Int J Esthet Dent 13(3):334–356
Dragoo MR (1997) Resin-ionomer and hybrid-ionomer cements: part II, human clinical and histologic wound healing responses in specific periodontal lesions. Int J Periodontics Restorative Dent 17(1):75–87
Santamaria MP, Mathias IF, Dias SB, Jardini MA, Junior MS, Sallum EA (2014) Esthetic evaluation of different approaches to treat gingival recession associated with non-carious cervical lesion treatment: a 2-year follow-up. Am J Dent 27(4):220–224
Martins TM, Bosco AF, Nobrega FJ, Nagata MJ, Garcia VG, Fucini SE (2007) Periodontal tissue response to coverage of root cavities restored with resin materials: a histomorphometric study in dogs. J Periodontol 78(6):1075–1082. https://doi.org/10.1902/jop.2007.060457
Bertoldi C, Monari E, Cortellini P, Generali L, Lucchi A, Spinato S, Zaffe D (2020) Clinical and histological reaction of periodontal tissues to subgingival resin composite restorations. Clin Oral Investig 24:1001–1011. https://doi.org/10.1007/s00784-019-02998-7
Carvalho BAS, Duarte CAB, Silva JF, Batista WWDS, Douglas-De-Oliveira DW, De Oliveira ES, Soares LDG, Galvão EL, Rocha-Gomes G, Glória JCR, Gonçalves PF, Flecha OD (2020) Clinical and radiographic evaluation of the Periodontium with biologic width invasion. BMC Oral Health 20:1–6. https://doi.org/10.1186/s12903-020-01101-x
Stetler KJ, Bissada NF (1987) Significance of the width of keratinized gingiva on the periodontal status of teeth with submarginal restorations. J Periodontol 58:696–700. https://doi.org/10.1902/jop.1987.58.10.696
Cook DR, Mealey BL, Verrett RG, Mills MP, Noujeim ME, Lasho DJ, Cronin RJ (2011) Relationship between clinical periodontal biotype and labial plate thickness: an in vivo study. Int J Periodontics Restorative Dent 31:345–354. https://doi.org/10.11607/prd.00.0985
Dietschi D, Spreafico R (1998) Current clinical concepts for adhesive cementation of tooth-colored posterior restorations. Pract Periodontics Aesthet Dent 10:47–54
Paolantonio M, D’Ercole S, Perinetti G, Tripodi D, Catamo G, Serra E, Bruè C, Piccolomini R (2004) Clinical and microbiological effects of different restorative materials on the periodontal tissues adjacent to subgingival class V restorations. 1-Year results. J Clin Periodontol 31:200–207. https://doi.org/10.1111/j.0303-6979.2004.00472.x
Santos VR, Lucchesi JA, Cortelli SC, Amaral CM, Feres M, Duarte PM (2007) Effects of glass ionomer and microfilled composite subgingival restorations on periodontal tissue and subgingival biofilm: a 6-month evaluation. J Periodontol 78:1522–1528. https://doi.org/10.1902/jop.2007.070032
Parirokh M, Torabinejad M, Dummer PMH (2018) Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part I: vital pulp therapy. Int Endod J 51(2):177–205. https://doi.org/10.1111/iej.12841
Torabinejad M, Parirokh M, Dummer PMH (2018) Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part II: other clinical applications and complications. Int Endod J 51(3):284–317. https://doi.org/10.1111/iej.12843
Jafari F, Jafari S, Etesamnia P (2017) Genotoxicity, bioactivity and clinical properties of calcium silicate based sealers: a literature review. Iran Endod J 12(4):407–413. https://doi.org/10.22037/iej.v12i4.17623
Fuss Z, Trope M (1996) Root perforations: classification and treatment choices based on prognostic factors. Endod Dent Traumatol 12:255–264
Moinzadeh AT, Aznar Portoles C, Schembri Wismayer P, Camilleri J (2016) Bioactivity potential of EndoSequence BC RRM Putty. J Endod 42(4):615–621. https://doi.org/10.1016/j.joen.2015.12.004
Walsh RM, He J, Schweitzer J, Opperman LA, Woodmansey KF (2018) Bioactive endodontic materials for everyday use: a review. Gen Dent 66(3):48–51
Malkondu O, Karapinar Kazandag M, Kazazoglu E (2014) A review on Biodentine, a contemporary dentine replacement and repair material. Biomed Res Int 2014:160951–160910. https://doi.org/10.1155/2014/160951
Guven EP, Tasli PN, Yalvac ME, Sofiev N, Kayahan MB, Sahin F (2013) In vitro comparison of induction capacity and biomineralization ability of mineral trioxide aggregate and a bioceramic root canal sealer. Int Endod J 46(12):1173–1182. https://doi.org/10.1111/iej.12115
Leiendecker AP, Qi YP, Sawyer AN, Niu LN, Agee KA, Loushine RJ, Weller RN, Pashley DH, Tay FR (2012) Effects of calcium silicate-based materials on collagen matrix integrity of mineralized dentin. J Endod 38(6):829–833. https://doi.org/10.1016/j.joen.2012.01.004
Camilleri J (2013) Investigation of Biodentine as dentine replacement material. J Dent 41(7):600–610. https://doi.org/10.1016/j.jdent.2013.05.003
Zhou HM, Shen Y, Wang ZJ, Li L, Zheng YF, Hakkinen L, Haapasalo M (2013) In vitro cytotoxicity evaluation of a novel root repair material. J Endod 39(4):478–483. https://doi.org/10.1016/j.joen.2012.11.026
Marconyak LJ Jr, Kirkpatrick TC, Roberts HW, Roberts MD, Aparicio A, Himel VT, Sabey KA (2016) A comparison of coronal tooth discoloration elicited by various endodontic reparative materials. J Endod 42(3):470–473. https://doi.org/10.1016/j.joen.2015.10.013
Karypidou A, Chatzinikolaou ID, Kouros P, Koulaouzidou E (2016) Management of bilateral invasive cervical resorption lesions in maxillary incisors using a novel calcium silicate-based cement: a case report. Quintessence Int 47:637–642
Eftekhar L, Ashraf H, Jabbari S (2017) Mandibular canine using Biodentine as a restorative material. Iran Endod J 12:386–389. https://doi.org/10.22037/iej.v12i3
Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG (2010) Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol 8(6):e1000412. https://doi.org/10.1371/journal.pbio.1000412
Donath K, Breuner G (1982) A method for the study of undecalcified bones and teeth with attached soft tissues. The Sage-Schliff (sawing and grinding) technique. J Oral Pathol 11(4):318–326. https://doi.org/10.1111/j.1600-0714.1982.tb00172.x
Levai G, Varga S, Gyarmati J, Laczko J (1975) Effect of triiodothyronine treatment, thyroparathyroidectomy and mercaptoiminazole treatment on enchondral bone growth. Changes in the histological structure of the growth organ. Acta Morphol Acad Sci Hung 23(1):9–19
Parma-Benfenali S, Fugazzoto PA, Ruben MP (1985) The effect of restorative margins on the postsurgical development and nature of the periodontium. Part I Int J Periodontics Restorative Dent 5(6):30–51
Pama-Benfenati S, Fugazzotto PA, Ferreira PM, Ruben MP, Kramer GM (1986) The effect of restorative margins on the postsurgical development and nature of the periodontium. Part II Anat considerations Int J Periodontics Restorative Dent 6(1):64–75
Nassar U, Meyer AE, Ogle RE, Baier RE (1995) The effect of restorative and prosthetic materials on dental plaque. Periodontol 2000 8:114–124. https://doi.org/10.1111/j.1600-0757.1995.tb00049.x
Waerhaug J (1956) Effect of rough surfaces upon gingival tissue. J Dent Res 35(2):323–325. https://doi.org/10.1177/00220345560350022601
Svanberg M, Mjor IA, Orstavik D (1990) Mutans streptococci in plaque from margins of amalgam, composite, and glass-ionomer restorations. J Dent Res 69(3):861–864. https://doi.org/10.1177/00220345900690030601
Zucchelli G, Gori G, Mele M, Stefanini M, Mazzotti C, Marzadori M, Montebugnoli L, De Sanctis M (2011) Non-carious cervical lesions associated with gingival recessions: a decision-making process. J Periodontol 82(12):1713–1724. https://doi.org/10.1902/jop.2011.110080
Veneziani M (2010) Adhesive restorations in the posterior area with subgingival cervical margins: new classification and differentiated treatment approach. Eur J Esthet Dent 5(1):50–76
Juloski J, Köken S, Ferrari M (2018) Cervical margin relocation in indirect adhesive restorations: a literature review. J Prosthodont Res 62:273–280
Oppermann R, Gomes S, Cavagni J, Cayana E, Conceição E (2016) Response to proximal restorations placed either subgingivally or following crown lengthening in patients with no history of periodontal disease. Int J Periodontics Restorative Dent 36:117–124. https://doi.org/10.11607/prd.2015
Tirone F, Salzano S, Piattelli A, Perrotti V, Iezzi G (2018) Response of periodontium to mineral trioxide aggregate and Biodentine: a pilot histological study on humans. Aust Dent J 63(2):231–241. https://doi.org/10.1111/adj.12605
Estrela C, Decurcio DA, Rossi-Fedele G, Silva JA, Guedes OA, Borges AH (2018) Root perforations: a review of diagnosis, prognosis and materials. Braz Oral Res 32(suppl 1):e73. https://doi.org/10.1590/1807-3107bor-2018.vol32.0073
Silva RAB, Borges ATN, Hernandez-Gaton P, de Queiroz AM, Arzate H, Romualdo PC, Nelson-Filho P, Silva LAB (2019) Histopathological, histoenzymological, immunohistochemical and immunofluorescence analysis of tissue response to sealing materials after furcation perforation. Int Endod J 52:1489–1500. https://doi.org/10.1111/iej.13145
Blank LW, Caffesse RG, Charbeneau GT (1979) The gingival response to well-finished composite resin restorations. J Prosthet Dent 42(6):626–632. https://doi.org/10.1016/0022-3913(79)90192-6
Gomes SC, Miranda LA, Soares I, Oppermann RV (2005) Clinical and histologic evaluation of the periodontal response to restorative procedures in the dog. Int J Periodontics Restorative Dent 25(1):39–47
Ghezzi C, Brambilla G, Conti A, Dosoli R, Ceroni F, Ferrantino L (2019) Cervical margin relocation: case series and new classification system. Int J Esthet Dent 14(3):272–284
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Castelo-Baz, P., Argibay-Lorenzo, O., Muñoz, F. et al. Periodontal response to a tricalcium silicate material or resin composite placed in close contact to the supracrestal tissue attachment: a histomorphometric comparative study. Clin Oral Invest 25, 5743–5753 (2021). https://doi.org/10.1007/s00784-021-03876-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03876-x