Abstract
Objectives
Although panoramic radiographs are extensively studied for diagnosis and preoperative planning in third molar surgery, research on the predictive value of this radiographic information regarding the postoperative recovery of patients remains underexploited. This prospective cohort study aimed to assess the potential relationship between radiologic risk indicators and persistent postoperative morbidity, in 1009 patients undergoing 2825 third molar extractions in context of the M3BE study.
Methods
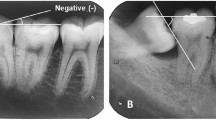
Two observers evaluated ten radiographic parameters: vertical and horizontal eruption status, third molar orientation, surgical difficulty, nerve relation, maxillary sinus relation, presence of periapical and pericoronal radiolucencies, caries, and third or second molar resorption. Patients’ postoperative recovery was recorded 3 and 10 days after surgery. Univariate logistic regression was performed to assess potential associations between radiographic risk indicators and persistent postoperative morbidity.
Results
Deep impactions were significantly associated with the persistence of postoperative pain, trismus and swelling until 10 days after surgery, prolonged need for pain medication, and the inability to resume daily activities and work/studies. Pericoronal radiolucencies and resorption were significantly associated with persistent morbidity and a longer recovery time, whereas caries and periapical lesions were linked to a shorter recovery time.
Conclusion
Based on the results of this study, clinicians may better inform patients at risk for persistent postoperative discomfort according to what was preoperatively diagnosed on the panoramic radiograph.
Clinical relevance
Preoperative panoramic radiographs contain information about patients at risk of prolonged recovery after third molar removal. Several risk indicators for persistent postoperative morbidity were identified.


Similar content being viewed by others
References
Shepherd J, Brickley M (1994) Surgical removal of third molars. Br Med J 309:620–621
Bello SA, Adeyemo WL, Bamgbose BO, Obi EV, Adeyinka AA (2011) Effect of age, impaction types and operative time on inflammatory tissue reactions following lower third molar surgery. Head Face Med 7:8
Deliverska EG, Petkova M (2016) Complications after extraction of impacted third molars: literature review. J IMAB Ann Proc 22:1202–1211
Pérez-Gonzàlez J, Esparza-Villalpando V, Martinez-Rider R, Noyola-Frías M, Pozos-Guillén A (2018) Clinical and radiographic characteristics as predictive factors of swelling and trismus after mandibular third molar surgery: a longitudinal approach. Pain Res Manag 7938492
de Santana-Santos T, de Souza-Santos JA, Martins-Filho PR, da Silva LC, de Oliveira e Silva ED, Gomes AC (2013) Prediction of postoperative facial swelling, pain and trismus following third molar surgery based on preoperative variables. Med Oral Patol Oral Cir Bucal 18:65–70
Slade GD, Foy SP, Shugars DA, Phillips C, White RP Jr (2004) The impact of third molar symptoms, pain, and swelling on oral health-related quality of life. J Oral Maxillofac Surg 62:1118–1124
Malkawi Z, Al-Omiri MK, Khraisat A (2011) Risk indicators of postoperative complications following surgical extraction of lower third molars. Med Princ Pract 20:321–325
Bui CH, Seldin EB, Dodson TB (2003) Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg 61:1379–1389
Meara DJ (2012) Evaluation of third molars: clinical examination and imaging techniques. Atlas Oral Maxillofac Surg Clin North Am 20:163–168
Brasil DM, Nascimento EHL, Gaeta-Araujo H, Oliveira-Santos C, Maria de Almeida S (2019) Is panoramic imaging equivalent to cone-beam computed tomography for classifying impacted lower third molars? J Oral Maxillofac Surg 77:1968–1974
Su N, van Wijk A, Berkhout E, Sanderink G, De Lange J, Wang H et al (2017) Predictive value of panoramic radiography for injury of inferior alveolar nerve after mandibular third molar surgery. J Oral Maxillofac Surg 75:663–679
Pell GJ, Gregory GT (1933) Impacted mandibular third molars: classification and modified technique for removal. Dent Dig 39
Winter G (1926) Principles of exodontia as applied to the impacted third molars. American Medical Books, St. Louis
Pederson GW (1988) Surgical removal of tooth. Oral surgery. WB Saunders, Philadelphia
Rood JP, Nooraldeen Shehab BAA (1990) The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg 28:20–25
Jung YH, Cho BH (2012) Assessment of maxillary third molars with panoramic radiography and cone-beam computed tomography. Imaging Sci Dent 45:233–240
Freudlsperger C, Deiss T, Bodem J, Engel M, Hoffmann J (2012) Influence of lower third molar anatomic position on postoperative inflammatory complications. J Oral Maxillofac Surg 70:1280–1285
Yuasa H, Sugiura M (2004) Clinical postoperative findings after removal of impacted mandibular third molars: prediction of postoperative facial swelling and pain based on preoperative variables. Br J Oral Maxillofac Surg 42:209–214
Garcia AG, Grana PM, Sampedro FG, Diago MP, Rey JM (2003) Does oral contraceptive use affect the incidence of complications after extraction of a mandibular third molar? Br Dent J 194:453–455
Brooks AS (2011) Delayed complications of tooth extraction in patients taking warfarin, antibiotics, and other medications. J Oral Maxillofac Surg 69:977–979
Kunkel M, Kleis W, Morbach T, Wagner W (2007) Severe third molar complications including death-lessons from 100 cases requiring hospitalization. J Oral Maxillofac Surg 65:1700–1706
Chuang SK, Perrott DH, Susarla SM, Dodson TB (2008) Risk factors for inflammatory complications following third molar surgery in adults. J Oral Maxillofac Surg 66:2213–2218
Matzen LH, Petersen LB, Schropp L, Wenzel A (2019) Mandibular canal-related parameters interpreted in panoramic images and CBCT of mandibular third molars as risk factors to predict sensory disturbances of the inferior alveolar nerve. Int J Oral Maxillofac Surg 48:1094–1101
Sisk AL, Hammer WB, Shelton DW, Joy ED Jr (1986) Complications following removal of impacted third molars: the role of the experience of the surgeon. J Oral Maxillofac Surg 44:855–859
Lanzer M, Pejicic R, Kruse AL, Schneider T, Gratz KW, Lubbers HT (2015) Anatomic (positional) variation of maxillary wisdom teeth with special regard to the maxillary sinus. Swiss Dent J 125:555–571
Santamaria MR, Valmesade Castellon E, Berini Aytes L, Gay Escoda C (2006) Incidence of oral sinus communications in 389 upper third molar extraction. Med Oral Patol Oral Cir Bucal 11:E334–E338
Chiapasco M, De Cicco L, Marrone G (1993) Side effects and complications associated with third molar surgery. Oral Surg Oral Med Oral Pathol 76:412–420
Bali A, Bali D, Sharma A, Verma G (2013) Is Pederson index a true predictive difficulty index for impacted mandibular third molar surgery? A meta-analysis. J Maxillofac Oral Surg 12:359–364
Ren YF, Malmstrom HS (2007) Effectiveness of antibiotic prophylaxis in third molar surgery: a meta-analysis of randomized controlled clinical trials. J Oral Maxillofac Surg 65:1909–1921
Adde CA, Soares MS, Romano MM, Carnaval TG, Sampaio RM, Aldarvis FP, Federico LRTA (2012) Clinical and surgical evaluation of the indication of postoperative antibiotic prescription in third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol 114:S26–S31
McCoy JM (2012) Complications of retention: pathology associated with retained third molars. Atlas Oral Maxillofac Surg Clin North Am 20:177–195
Offenbacher S, Beck JD, Moss KL, Barros S, Mendoza L, White RP Jr (2012) What are the local and systemic implications of third molar retention? J Oral Maxillofac Surg 70:S58–S65
Vandeplas C, Vranckx M, Hekner D, Politis C, Jacobs R (2020) Does retaining third molars result in the development of pathology over time? A systematic review. J Oral Maxillofac Surg S0278-2391:30588–7
Ventä I, Vehkalahti MM, Suominen AL (2019) What kind of third molars are disease-free in a population aged 30 to 93 years? Clin Oral Investig 23:1015–1022
Radiation Protection (2004) European guidelines on radiation protection in dental radiology: the safe use radiographs dental practice. European Commission Vol 136
Acknowledgments
All authors listed above have made a significant contribution to this manuscript and have agreed to its submission. We would like to acknowledge Wim Coucke for his help in the statistical analysis.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The study was approved by the Medical Ethical Committee of the University Hospitals of Leuven (Belgium) (B322201525552). All procedures performed in this study, involving human participants, were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vranckx, M., Lauwens, L., Moreno Rabie, C. et al. Radiological risk indicators for persistent postoperative morbidity after third molar removal. Clin Oral Invest 25, 4471–4480 (2021). https://doi.org/10.1007/s00784-020-03759-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03759-7