Abstract
Objectives
The aim of this study was categorizing the microbial flora and susceptibility to antibiotics and to clarify to which degree the empiric administered antibiotics are suitable for therapy.
Materials and methods
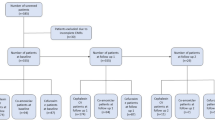
A 3.5-year retrospective study evaluated hospital records of 206 patients who suffered from head and neck infections of odontogenic origin. All patients underwent surgical incision and drainage and received intravenous antibiotics and inpatient treatment. The specimens were obtained by performing a swab.
Results
Two hundred six patients were included with 251 strains isolated (1.22 per patient). One hundred eight strains showed antibiotic resistance. Eighty-seven patients showed at least one bacterial strain that showed antibiotic resistance (42.2%). The most frequent isolated bacteria were Streptococcus spp. (n = 116), with a high rate of antibiotic resistance (50.8%). We investigated 205 cases of antibiotic resistance in 87 subjects. Nine bacterial strains showed no susceptibility to unacid (4.3%) and 36 strains to clindamycin (17.5%).
Conclusion
Antibiotic resistance against clindamycin was rather high. The distribution of the afflicted spaces and isolated bacteria was alike recent findings. It is mandatory to understand that immediate surgical treatment in terms of incision and drainage is the basis in abscess treatment. Antibiotic treatment is adjunct therapy.
Clinical relevance
Streptococcus species were the most frequently identified bacteria presenting antibiotic resistance in more than 50%. Increased resistant rates for clindamycin require reconsiderations regarding an empiric antibiotic treatment.

Similar content being viewed by others
References
Huang TT, Liu TC, Chen PR, Tseng FY, Yeh TH, Chen YS (2004) Deep neck infection: analysis of 185 cases. Head Neck 26(19):854–860
Boscolo-Rizzo P, Da Mosto MC (2009) Submandibular space infection. A potential lethal infection. Int J Infect Dis 13(3):327–333
Azenha MR, Homsi G, Garcia IR Jr (2012) Multiple brain absces from dental origin: case report and literature review. Oral Maxillofac Surg 16(4):393–397
Tavakoli M, Bagheri A, Faraz M, Salehirad S, Roghaee S (2013) Orbital cellulitis as a complication of mandibular odontogenic infection. Opthal Plast Reconstr Surg 29(1):e5–e7
Pappa H, Jones DC (2005) Mediastinitis from odontogenic infection: a case report. Br Dent J 198:548
Dhariwal DK, Patton DW, Gregory MC (2003) Epidural spinal abscess following dental extraction - a rare and potentially fatal complication. Br J Maxillofac Surg 41:58
DeAngelis AF, Barrowmann RA, Harrod R, Nastri AL (2014) Review article: Maxillofacial emergencies: oral pain and odontogenic infections. Emerg Med Australas 26(4):336–342
Seppanen L, Lauhio A, Lindqvist C, Suuronen R, Rautemaa R (2008) Analysis of systemic and local odontogenic infection complications requiring hospital care. J Inf Secur 57(2):116.e122
Sandner A, Börgermann J (2011) Update on necrotizing mediastinitis: causes, approaches to management, and outcomes. Curr Infect Dis Rep 13(3):278.e286
Walia IS, Borle RM, Mehendiratta D, Yadav AO (2014) Microbiology and antibiotic sensitivity of head and neck space infections of odontogenic origin. J Maxillofac Oral Surg 13(1):16–21
Kuriyama T, Williams DW, Yanagisawa M, Iwahara K, Shimizu C, Nakagawa K, Yamamoto E, Karasawa T (2007) Antimicrobial susceptibility of 800 anaerobic isolates from patients with dentoalveolar infection to 13 oral antibiotics. Oral Microbiol Immunol 22(4):285–288
Lopez-Piriz R, Aguilar L, Gimenez MJ (2007) Management of odontogenic infection of pulpal and periodontal origin. Med Oral Patol Oral Cir Bucal 12(2):E154–E159
Sobottka I, Wegschneider K, Balzer L, Böger RH, Hallier O, Giersdorf I, Streichert T, Haddad M, Platzer U, Cachovan G (2012) Microbial analysis of a prospective, randomized, double-blind trial comparing maxifloxacin and clindamycin in the treatment of odontogenic infiltrates and abscesses. Antimicrob Agents Chemother 56(5):2565–2569
Robertson D, Smith AJ (2009) The microbiology of the acute dental abscess. J Med Microbiol 58(Pt2):155–162
Salomon D, Heidel RE, Kolokythas A, Miloro M, Schlieve T (2017) Does restriction of public health care dental benefits affect the volume, severity, or cost of dental-related hospital visits? J Oral Maxillofac Surg 75:467–474
Burnham R, Bhandari R, Bridle C (2011) Changes in admission rates for spreading odontogenic infection resulting from changes in government policy about the dental schedule and remunerations. Br J Oral Maxillofac Surg 49:26–28
Sanchez R, Mirada E, Arias J, Pano JR, Burgueno M (2011) Severe odontogenic infections: epidemiological, microbiological and therapeutic factors. Med Oral Patol Oral Cir 16(5):e670–e676
Zirk M, Buller J, Goeddertz P, Rothamel D, Dreiseidler T, Zoller JE, Kreppel M (2016) Empiric systemic antibiotics for hospitalized patients with severe odontogenic infections. J Craniomaxillofac Surg 44(8):1081–1088
Heim N, Warwas FB, Wiedemeyer V, Wilms CT, Reich RH, Martini M (2019) The role of immediate versus secondary removal of the odontogenic focus in treatment of deep head and neck space infections. A retrospective analysis of 248 patients. Clin Oral Investig 23(7):2921–2927
Epstein S, Scoop IW (1977) Antibiotics and the intraoral abscess. J Periodontol 48:236
Hunt DE, Meyer RA (1983) Continued evolution of the microbiology of oral infections. J Am Dent Assoc 107:52
Levi ME, Eustermann VD (2011) Oral infections and antibiotic therapy. Otolaryngol Clin North Am 44(1):57–78
Rega AJ, Aziz SR, Ziccardi VB (2006) Microbiology and antibiotic sensitivities of head and neck space infections of odontogenic origin. J Oral Maxillofac Surg 64(9):1377–1380
Al-Nawas B, Maeurer M (2008) Severe versus local odontogenic bacterial infections: comparison of microbial isolates. Eur Surg Res 40(2):220–224
Eick S, Pfister W, Straube E (1999) Antimicrobial susceptibility of anaerobic and capnophilic bacteria isolated from odontogenic abscesses and rapidly progressive periodontitis. Int J Antimicrob Agents 12(1):41–46
Plum AW, Mortelliti AJ, Walsh RE (2018) Microbial flora and antibiotic resistance in odontogenicabscesses in Upstate New York. Ear Nose Throat J 97(1-2):E27–E31
Martinez JL (2009) The role of natural environments in the evolution of resistance traits in pathogenic bacteria. Proc R Soc B Biol Sci 276:2521–2530
Baumgartner JC, Xia T (2003) Antibiotic susceptibility of bacteria associated with endodontic abscess. J Endond 29(1):44–47
Yarlagadda K, Shrimanker I, Nookala VK (2019) Catheter-associated Hafnia alvei-induced urosepsis. Cureus 11(12):e6471
Jolivet-Gougeon A, Sixou JL, Tamanai-Shacoori Z, Bonnaure-Mallet M (2007) Antimicrobial treatment of Capnocytophaga infections. Int. J. Antimicrob. Agents 29(4):367–373
Shafquat Y, Jabeen K, Farooqi J, Mehmood K, Irfan S, Hasan R, Zafar A (2019) Antimicrobial susceptibility against metronidazole and carbapenem in clinical anaerobic isolates from Pakistan. Antimicrob Resist. Infect Control 8:99
Lodise TP, Patel N, Lomaestro BM, Rodvold KA, Drusano GL (2009) Relationship between initial vancomycin concentration-time profile and nephrotoxicity (toxic to the kidneys) among hospitalized patients. Clin Infect Dis 49(4):507–514
Kang SH, Kim MK (2019) Antibiotic sensitivity and resistance of bacteria from odontogenic maxillofacial abscesses. J Korean Assoc Oral Maxillofac Surg 45(6):324–331
Singh M, Kambalimath DH, Gupta KC (2014) Management of odontogenic space infection with microbiology study. J Maxillofac Oral Surg 13(2):133–139
Shah A, Ramola V, Nautiyal V (2016) Aerobic microbiology and culture sensitivity of head and neck space infection of odontogenic origin. Natl J Maxillofac Surg 7(1):56–61
Weise H, Naros A, Weise C, Reinert S, Hoefert S (2019) Severe odontogenic infections with septic progress - a constant and increasing challenge: a retrospective analysis. BMC Oral Health 19(1):173
Thomas SJ, Atkinson C, Hughes C, Revington P, Ness AR (2008) Is there an epidemic of admissions for surgical treatment of dental abscess in the UK? BMJ 336:1219–1220
Fu B, McGowan K, Sun JH, Batstone M (2020) Increasing frequency and severity of odontogenic infection requiring hospital admission and surgical management. Br J Oral Maxillofac Surg 58:409–415. https://doi.org/10.1016/j.boms.2020.01.011
Carter LM, Layton S (2009) Cervicofacial infection of dental origin presenting to maxillofacial surgery units in the United Kingdom: a national audit. Br Dent J 206:73–78
Gilmour AS, Welply A, Cowpe JG, Bullock AD, Jones RJ (2016) The undergraduate preparation of dentists: confidence levels of final year dental students at the School of Dentistry in Cardiff. Br Dent J 221:349–354
Jundt JS, Gutta R (2012) Characteristics and cost impact of severe odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol 114:558–566
Eisler L, Wearda K, Romatoski K, Odland RM (2013) Morbidity and cost of odontogenic infections. Otolaryngol Head Neck Surg 149:84–88
Nalliah RP, Allareddy V, Elangovan S, Karimbux N, Allareddy V (2011) Hospital emergency department visits attributed to pulpal and periapical disease in the United States in 2006. J Endod 37:6–9
Heim N, Faron A, Wiedemeyer V, Reich R, Martini M (2017) Microbiology and antibiotic sensitivity of head and neck space infections of odontogenic origin. Differences in inpatient and outpatient management. J Craniomaxillofac Surg 45(10):1731–1735
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
This article is a retrospective analysis and does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Heim, N., Jürgensen, B., Kramer, FJ. et al. Mapping the microbiological diversity of odontogenic abscess: are we using the right drugs?. Clin Oral Invest 25, 187–193 (2021). https://doi.org/10.1007/s00784-020-03350-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03350-0