Abstract
Objectives
To determine if patient outcome variables differ between conventional and virtual surgical planning of orthognathic surgery for class III asymmetry.
Material and methods
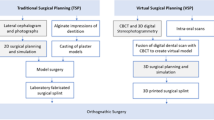
This retrospective case-control study examined 95 patients with class III asymmetry who had been consecutively treated with at least a Le Fort I osteotomy and a bilateral sagittal split osteotomy with a surgery-first approach. Two groups were examined: 51 patients treated with conventional surgical planning and 44 with virtual surgical planning. After treatment, quantitative assessment was determined with measurements of midline symmetry, contour symmetry, and overall facial symmetry using standardized frontal photographs. Subject assessments were analyzed with questionnaires regarding self-perception of overall appearance, satisfaction with appearance, and quality of life.
Results
Conventional and virtual surgical planning resulted in significant improvements in outcomes for all patients. However, facial midline and overall facial symmetry were significantly greater for the virtual compared with the conventional group. There were no significant differences in subjective measures of appearance, satisfaction with appearance, and quality of life for patients treated with conventional or virtual surgical planning; measures were high for both groups.
Conclusions
Conventional and virtual surgical planning of surgery-first bimaxillary orthognathic surgery resulted in quantitative and qualitative improvements in facial symmetry. Although patient satisfaction was similar for both approaches, virtual surgical planning was superior to conventional surgical planning for the improvement of midline and overall asymmetry.
Clinical relevance
Improvements with virtual surgical planning in facial midline, facial contour, and overall facial symmetry are as good as or better than conventional surgical planning.




Similar content being viewed by others
References
Xia JJ, Phillips CV, Gateno J, Teichgraeber JF, Christensen AM, Gliddon MJ, Lemoine JJ, Liebschner MA (2006) Cost-effectiveness analysis for computer-aided surgical simulation in complex cranio-maxillofacial surgery. J Oral Maxillofac Surg 64:1780–1784
Iorio ML, Masden D, Blake CA, Baker SB (2011) Presurgical planning and time efficiency in orthognathic surgery: the use of computer-assisted surgical simulation. Plast Reconstr Surg 128:179e–181e
Steinhuber T, Brunold S, Gärtner C, Offermanns V, Ulmer H, Ploder O (2018) Is virtual surgical planning in orthognathic surgery faster than conventional planning? A time and workflow analysis of an office-based workflow for single- and double-jaw surgery. J Oral Maxillofac Surg 76:397–407
Xia JJ, Shevchenko L, Gateno J, Teichgraeber JF, Taylor TD, Lasky RE, English JD, Kau CH, McGrory KR (2011) Outcome study of computer-aided surgical simulation in treatment of patients with craniomaxillofacial deformities. J Oral Maxillofac Surg 69:2014–2024
Lonic D, Pai BC, Yamaguchi K, Chortrakarnkij P, Lin HH, Lo LJ (2016) Computer-assisted orthognathic surgery for patients with cleft lip/palate: from traditional planning to three-dimensional surgical simulation. PLoS One 11:e0152014
Ho CT, Lin HH, Liou EJ, Lo LJ (2017) Three-dimensional surgical simulation improves the planning for correction of facial prognathism and asymmetry: A qualitative and quantitative study. Sci Rep 7:40423
De Riu G, Meloni SM, Baj A, Corda A, Soma D, Tullio A (2014) Computer-assisted orthognathic surgery for correction of facial asymmetry: results of a randomized controlled clinical trial. Br J Oral Maxillofac Surg 52:251–257
Bengtsson M, Wall G, Greiff L, Rasmusson L (2017) Treatment outcome in orthognathic surgery-A prospective randomized blinded case-controlled comparison of planning accuracy in computer-assisted two- and three-dimensional planning techniques (part II). J Craniomaxillofac Surg 45:1419–1424
Udomlarptham N, Lin CH, Wang YC, Ko EW (2018) Does two-dimensional vs. three-dimensional surgical simulation produce better surgical outcomes among patients with class III facial asymmetry? Int J Oral Maxillofac Surg 47:1022–1031
Tucker S, Cevidanes LH, Styner M, Kim H, Reyes M, Proffit W, Turvey T (2010) Comparison of actual surgical outcomes and 3-dimensional surgical simulations. J Oral Maxillofac Surg 68:2412–2421
Wu TY, Lin HH, Lo LJ, Ho CT (2017) Postoperative outcomes of two- and three-dimensional planning in orthognathic surgery: A comparative study. J Plast Reconstr Aesthet Surg 70:1101–1111
Ko EW, Lin CH, Chen YA, Chen YR (2018) Enhanced surgical outcomes in patients with skeletal class III facial asymmetry by 3-dimensional surgical simulation. J Oral Maxillofac Surg 76:1073–1083
Zhang N, Liu S, Hu Z, Hu J, Zhu S, Li Y (2016) Accuracy of virtual surgical planning in two-jaw orthognathic surgery: Comparison of planned and actual results. Oral Surg Oral Med Oral Pathol Oral Radiol 122:143–151
Liao YF, Chen YF, Yao CF, Chen YA, Chen YR (2019) Long-term outcomes of bimaxillary surgery for treatment of asymmetric skeletal class III deformity using surgery-first approach. Clin Oral Investig 23:1685–1693
Liao YF, Chiu YT, Huang CS, Ko EW, Chen YR (2010) Presurgical orthodontics versus no presurgical orthodontics: treatment outcome of surgical-orthodontic correction for skeletal class III open bite. Plast Reconstr Surg 126:2074–2083
Hunsuck EE (1968) A modified intra-oral sagittal splitting technique for correction of mandibular prognathism. J Oral Surg 26:250–253
Honda T, Lin CH, Yu CC, Heller F, Chen YR (2005) The medial surface of the mandible as an alternative source of bone grafts in 404 orthognathic surgery. J Craniofac Surg 16:123–128
Bell WH (1992) Modern practice in orthognathic and reconstructive surgery. Saunders, Philadelphia
Chu YM, Po-Hsun Chen R, Morris DE, Wen-Ching Ko E, Chen YR (2007) Surgical approach to the patient with bimaxillary protrusion. Clin Plast Surg 34:535–346
Yu CC, Bergeron L, Lin CH, Chu YM, Chen YR (2009) Single-splint technique in orthognathic surgery: intraoperative checkpoints to control facial symmetry. Plast Reconstr Surg 24:879–886
Ettorre G, Weber M, Schaaf H, Lowry JC, Mommaerts MY, Howaldt HP (2006) Standards for digital photography in craniomaxillofacial surgery—part I: basic views and guidelines. J Craniomaxillofac Surg 34:65–73
Schaaf H, Streckbein P, Ettorre G, Lowry JC, Mommaerts MY, Howaldt HP (2006) Standards for digital photography in craniomaxillofacial surgery—part II: additional picture sets and avoiding common mistakes. J Craniomaxillofac Surg 34:366–377
Lee LW, Chen SH, Yu CC, Lo LJ, Lee SR, Chen YR (2007) Stigma, body image, and quality of life in women seeking orthognathic surgery. Plast Reconstr Surg 120:225–231
Pruzinsky T, Cash TF (2002) Assessing body image and quality of life in medical settings. In: Cash TF, Pruzinsky T (eds) Body image: a handbook of theory, research, and clinical practice. Guilford Press, New York, pp 171–179
Hajeer MY, Ayoub AF, Millett DT (2004) Three-dimensional assessment of facial soft-tissue asymmetry before and after orthognathic surgery. Br J Oral Maxillofac Surg 42:396–404
Chen YF, Liao YF, Chen YA, Chen YR (2019) Treatment outcome of bimaxillary surgery for asymmetric skeletal class II deformity. Clin Oral Investig 23:623–632
Chung C, Lee Y, Park KH, Park SH, Park YC, Kim KH (2008) Nasal changes after surgical correction of skeletal class III malocclusion in Koreans. Angle Orthod 78:427–432
Baik HS, Kim SY (2010) Facial soft-tissue changes in skeletal class III orthognathic surgery patients analyzed with 3-dimensional laser scanning. Am J Orthod Dentofacial Orthop 138:167–178
Park SB, Yoon JK, Kim YI, Hwang DS, Cho BH, Son WS (2012) The evaluation of the nasal morphologic changes after bimaxillary surgery in skeletal class III maloccusion by using the superimposition of cone beam computed tomography (CBCT) volumes. J Craniomaxillofac Surg 40:e87–e92
Kim BR, Oh KM, Cevidanes LHS, Park JE, Sim HS, Seo SK, Reyes M, Kim YJ, Park YH (2013) Analysis of 3D soft tissue changes after 1- and 2-jaw orthognathic surgery in mandibular prognathism patients. J Oral Maxillofac Surg 71:151–161
Ko EWC, Huang CS, Chen YR (2009) Characteristics and corrective outcome of face asymmetry by orthognathic surgery. J Oral Maxillofac Surg 67:2201–2209
You KH, Lee KJ, Lee SH, Baik HS (2010) Three-dimensional computed tomography analysis of mandibular morphology in patients with facial asymmetry and mandibular prognathism. Am J Orthod Dentofac Orthop 138:540.e1–540.e8
Lee H, Bayome M, Kim SH, Kim KB, Behrents RG, Kook YA (2012) Mandibular dimensions of subjects with asymmetric skeletal class III malocclusion and normal occlusion compared with conebeam computed tomography. Am J Orthod Dentofac Orthop 142:179–185
Funding
The work was supported by the Chang Gung Memorial Hospital, Taiwan (CMRPG5F0051, CMRPG5F0061, CMRPG5G0021).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was not needed due to the retrospective design of the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liao, YF., Chen, YA., Chen, YC. et al. Outcomes of conventional versus virtual surgical planning of orthognathic surgery using surgery-first approach for class III asymmetry. Clin Oral Invest 24, 1509–1516 (2020). https://doi.org/10.1007/s00784-020-03241-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03241-4