Abstract
Objective
To assess longitudinal peri-implant tissue evaluation in a plaque compromised ligature free dog model, clinically, radiographically, microbiologically and histologically.
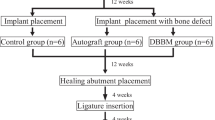
Materials and methods
Six beagle mandibular premolars and first molars were extracted. Plaque accumulated for 16 weeks. Two implants were placed per hemi-mandible. For 17 weeks, control implants (CI) in one hemi-mandible were brushed daily; test implants (TI) in the other were not. These parameters were then assessed: clinically, probing depth (PD), bleeding-on-probing (BOP), presence of plaque (PP) and clinical attachment level (CAL); radiographically, marginal bone level; microbiologically, counts for Streptococcus spp., Fusobacterium spp., Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans, Prevotella intermedia and total bacterial load. At week 17, histomorphometric analysis was performed (MM-ISH (mucosal margin–implant shoulder); ISH-fBIC (implant shoulder–first bone-to-implant contact); MM-aJE (mucosal margin–apical area junctional epithelium); MM-aINF (mucosal margin–apical limit of the inflammatory infiltrate); %INF (percentage of inflammatory infiltrate)).
Results
At week 17, TI had significant increased PD, BOP, PP and CAL versus baseline. All clinical variables presented intergroup differences. There was no intergroup difference for radiographic bone loss (p > 0.05). Total bacteria, Fusobacterium spp., A. actinomycetemcomitans and P. gingivalis had intergroup differences. There was no statistically significant intergroup difference for ISH-fBIC.
Conclusions
Longitudinal microbiology evaluation detected a shift period. Final intergroup microbiological differences were the basis of W17 clinical intergroup differences, with higher values in TI. Microbiological and clinical changes detected in peri-implant tissues were compatible with onset of peri-implant disease. Despite histological inflammatory intergroup difference, no histological or radiographic intergroup bone loss was detected.
Clinical relevance
This study set-up describes a valuable method for generating “true” early peri-implant defects without mechanical trauma.








Similar content being viewed by others
References
Albrektsson T, Dahlin C, Jemt T, Sennerby L, Turri A, Wennerberg A (2014) Is marginal bone loss around oral implants the result of a provoked foreign body reaction? Clin Implant Dent Relat Res 16(2):155–165. https://doi.org/10.1111/cid.12142
de Waal YC, van Winkelhoff AJ, Meijer HJ, Raghoebar GM, Winkel EG (2013) Differences in peri-implant conditions between fully and partially edentulous subjects: a systematic review. J Clin Periodontol 40(3):266–286. https://doi.org/10.1111/jcpe.12013
Jepsen S, Berglundh T, Genco R, Aass AM, Demirel K, Derks J, Figuero E, Giovannoli JL, Goldstein M, Lambert F, Ortiz-Vigon A, Polyzois I, Salvi GE, Schwarz F, Serino G, Tomasi C, Zitzmann NU (2015) Primary prevention of peri-implantitis: managing peri-implant mucositis. J Clin Periodontol 42(Suppl 16):S152–S157. https://doi.org/10.1111/jcpe.12369
Ericsson I, Berglundh T, Marinello C, Liljenberg B, Lindhe J (1992) Long-standing plaque and gingivitis at implants and teeth in the dog. Clin Oral Implants Res 3(3):99–103
Abrahamsson I, Berglundh T, Lindhe J (1998) Soft tissue response to plaque formation at different implant systems. A comparative study in the dog. Clin Oral Implants Res 9(2):73–79
Martins O, Ramos JC, Baptista IP, Dard MM (2014) The dog as a model for peri-implantitis: a review. J Investig Surg 27(1):50–56. https://doi.org/10.3109/08941939.2013.828805
Albouy JP, Abrahamsson I, Persson LG, Berglundh T (2009) Spontaneous progression of ligatured induced peri-implantitis at implants with different surface characteristics. An experimental study in dogs II: histological observations. Clin Oral Implants Res 20(4):366–371
Faggion CM Jr, Chambrone L, Gondim V, Schmitter M, Tu YK (2010) Comparison of the effects of treatment of peri-implant infection in animal and human studies: systematic review and meta-analysis. Clin Oral Implants Res 21(2):137–147. https://doi.org/10.1111/j.1600-0501.2009.01753.x
Zitzmann NU, Berglundh T, Ericsson I, Lindhe J (2004) Spontaneous progression of experimentally induced periimplantitis. J Clin Periodontol 31(10):845–849. https://doi.org/10.1111/j.1600-051X.2004.00567.x
Berglundh T, Gotfredsen K, Zitzmann NU, Lang NP, Lindhe J (2007) Spontaneous progression of ligature induced peri-implantitis at implants with different surface roughness: an experimental study in dogs. Clin Oral Implants Res 18(5):655–661. https://doi.org/10.1111/j.1600-0501.2007.01397.x
Albouy JP, Abrahamsson I, Berglundh T (2012) Spontaneous progression of experimental peri-implantitis at implants with different surface characteristics: an experimental study in dogs. J Clin Periodontol 39(2):182–187. https://doi.org/10.1111/j.1600-051X.2011.01820.x
Albouy JP, Abrahamsson I, Persson LG, Berglundh T (2008) Spontaneous progression of peri-implantitis at different types of implants. An experimental study in dogs. I: clinical and radiographic observations. Clin Oral Implants Res 19(10):997–1002. https://doi.org/10.1111/j.1600-0501.2008.01589.x
Marinello CP, Berglundh T, Ericsson I, Klinge B, Glantz PO, Lindhe J (1995) Resolution of ligature-induced peri-implantitis lesions in the dog. J Clin Periodontol 22(6):475–479
Berglundh T, Stavropoulos A, Working Group 1 of the VEWoP (2012) Preclinical in vivo research in implant dentistry. Consensus of the eighth European workshop on periodontology. J Clin Periodontol 39(Suppl 12):1–5. https://doi.org/10.1111/j.1600-051X.2011.01827.x
Klinge B (2012) Peri-implant marginal bone loss: an academic controversy or a clinical challenge? Eur J Oral Implantol 5(Suppl):S13–S19
Becker W (2012) Osseointegration: have we tinkered with the process too much? Clin Implant Dent Relat Res 14(6):779–780. https://doi.org/10.1111/cid.12009
Salvi GE, Aglietta M, Eick S, Sculean A, Lang NP, Ramseier CA (2012) Reversibility of experimental peri-implant mucositis compared with experimental gingivitis in humans. Clin Oral Implants Res 23(2):182–190. https://doi.org/10.1111/j.1600-0501.2011.02220.x
Lindhe J, Meyle J, Group DoEWoP (2008) Peri-implant diseases: consensus report of the Sixth European Workshop on Periodontology. J Clin Periodontol 35(8 Suppl):282–285. https://doi.org/10.1111/j.1600-051X.2008.01283.x
Augthun M, Conrads G (1997) Microbial findings of deep peri-implant bone defects. Int J Oral Maxillofac Implants 12(1):106–112
Heitz-Mayfield LJ, Lang, NP (2010) Comparative biology of chronic and aggressive periodontitis vs. peri-implantitis. Periodontol 53:167–181. doi:https://doi.org/10.1111/j.1600-0757.2010.00348.x
Kilkenny C, Browne W, Cuthill IC, Emerson M, Altman DG, National Centre for the Replacement R, Reduction of Amimals in R (2011) Animal research: reporting in vivo experiments—the ARRIVE guidelines. J Cereb Blood Flow Metab 31(4):991–993. https://doi.org/10.1038/jcbfm.2010.220
Cochran DL, Nummikoski PV, Schoolfield JD, Jones AA, Oates TW (2009) A prospective multicenter 5-year radiographic evaluation of crestal bone levels over time in 596 dental implants placed in 192 patients. J Periodontol 80(5):725–733. https://doi.org/10.1902/jop.2009.080401
Donath K, Breuner G (1982) A method for the study of undecalcified bones and teeth with attached soft tissues. The Sage-Schliff (sawing and grinding) technique. J Oral Pathol 11(4):318–326
Schwarz F, Jepsen S, Herten M, Sager M, Rothamel D, Becker J (2006) Influence of different treatment approaches on non-submerged and submerged healing of ligature induced peri-implantitis lesions: an experimental study in dogs. J Clin Periodontol 33(8):584–595. https://doi.org/10.1111/j.1600-051X.2006.00956.x
Ericsson I, Persson LG, Berglundh T, Marinello CP, Lindhe J, Klinge B (1995) Different types of inflammatory reactions in peri-implant soft tissues. J Clin Periodontol 22(3):255–261
Zitzmann NU, Abrahamsson I, Berglundh T, Lindhe J (2002) Soft tissue reactions to plaque formation at implant abutments with different surface topography. An experimental study in dogs. J Clin Periodontol 29(5):456–461
Struillou X, Boutigny H, Soueidan A, Layrolle P (2010) Experimental animal models in periodontology: a review. Open Dent J 4:37–47. https://doi.org/10.2174/1874210601004010037
Kortegaard HE, Eriksen T, Baelum V (2008) Periodontal disease in research beagle dogs—an epidemiological study. J Small Anim Pract 49(12):610–616. https://doi.org/10.1111/j.1748-5827.2008.00609.x
Quirynen M, Vogels R, Pauwels M, Haffajee AD, Socransky SS, Uzel NG, van Steenberghe D (2005) Initial subgingival colonization of ‘pristine’ pockets. J Dent Res 84(4):340–344
Wennerberg A, Albrektsson T (2010) On implant surfaces: a review of current knowledge and opinions. Int J Oral Maxillofac Implants 25(1):63–74
Pesce P, Menini M, Tealdo T, Bevilacqua M, Pera F, Pera P (2014) Peri-implantitis: a systematic review of recently published papers. Int J Prosthodont 27(1):15–25. https://doi.org/10.11607/ijp.3785
Pontoriero R, Tonelli MP, Carnevale G, Mombelli A, Nyman SR, Lang NP (1994) Experimentally induced peri-implant mucositis. A clinical study in humans. Clin Oral Implants Res 5(4):254–259
Mombelli A, Decaillet F (2011) The characteristics of biofilms in peri-implant disease. J Clin Periodontol 38(Suppl 11):203–213. https://doi.org/10.1111/j.1600-051X.2010.01666.x
Derks J, Schaller D, Hakansson J, Wennstrom JL, Tomasi C, Berglundh T (2016) Peri-implantitis—onset and pattern of progression. J Clin Periodontol 43(4):383–388. https://doi.org/10.1111/jcpe.12535
Heyman O, Koren N, Mizraji G, Capucha T, Wald S, Nassar M, Tabib Y, Shapira L, Hovav AH, Wilensky A (2018) Impaired differentiation of Langerhans cells in the murine oral epithelium adjacent to titanium dental implants. Front Immunol 9:1712. https://doi.org/10.3389/fimmu.2018.01712
Ferreira SD, Silva GL, Cortelli JR, Costa JE, Costa FO (2006) Prevalence and risk variables for peri-implant disease in Brazilian subjects. J Clin Periodontol 33(12):929–935. https://doi.org/10.1111/j.1600-051X.2006.01001.x
Lang NP, Wetzel AC, Stich H, Caffesse RG (1994) Histologic probe penetration in healthy and inflamed peri-implant tissues. Clin Oral Implants Res 5(4):191–201
Charalampakis G, Abrahamsson I, Carcuac O, Dahlen G, Berglundh T (2014) Microbiota in experimental periodontitis and peri-implantitis in dogs. Clin Oral Implants Res 25(9):1094–1098. https://doi.org/10.1111/clr.12235
Derks J, Tomasi C (2015) Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol 42(Suppl 16):S158–S171. https://doi.org/10.1111/jcpe.12334
Acknowledgements
The authors are very grateful to Dr. Philipp Sahrmann (Center of Dental Medicine, University of Zurich) for his contribution to this study.
Funding
The work was supported by Institut Straumann, Basel, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Orlando Martins declares that he has no conflict of interest. João Carlos Ramos declares that he has no conflict of interest. Marta Mota declares that she has no conflict of interest. Michel Dard is the Global Medical Director at Institut Straumann, Basel, Switzerland. Carlos Viegas declares that he has no conflict of interest. Francisco Caramelo declares that he has no conflict of interest. Célia Nogueira declares that she has no conflict of interest. Teresa Gonçalves declares that she has no conflict of interest. Isabel Poiares Baptista declares that she has no conflict of interest.
Ethical approval
All applicable international, national and/or institutional guidelines for the care and use of animals were followed.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martins, O., Ramos, J.C., Mota, M. et al. Evaluation of a novel dog animal model for peri-implant disease: clinical, radiographic, microbiological and histological assessment. Clin Oral Invest 24, 3121–3132 (2020). https://doi.org/10.1007/s00784-019-03186-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-03186-3