Abstract
Objective
This study aimed to longitudinally assess the risk of facial nerve injury (FNI) in the surgical repair of mandibular condylar neck and subcondylar fractures (CN/SCFs) and to explore its predictors.
Materials and methods
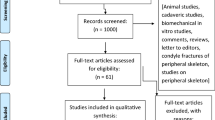
In a retrospective cohort study, the outcome was defined as FNI at 1 week and 1, 3, and 6 months postoperatively. Potential predictors included age, sex, etiology, fracture site and pattern (dislocation/non-dislocation), concomitant facial fractures, interval to surgery, surgeons’ experience, plate types, and the marginal mandibular branch-traversing approach (deep/superficial group). We employed generalized estimating equations (GEEs) for repeated measurements throughout the 6-month follow-up period.
Results
Among 102 patients with 114 fractures, 27 patients (26.5%) developed FNI within 1 week. Prolonged FNI (≥ 1 month) occurred in 19 (19.2%) of 99 patients. Multivariate GEE analyses revealed that deep surgical approaches (i.e., traditional submandibular and retroparotid approaches; odds ratio [OR], 18.90; p = 0.011), fractures with dislocation (OR, 3.60; p = 0.025), and female gender (OR, 2.71; p = 0.040) were independently associated with the overall FNI risk. Additionally, the deep approaches (OR, 15.91; p = 0.014) and female gender (OR, 3.41; p = 0.035) were correlated with a prolonged FNI risk. Sensitivity analyses for the outcomes identified the same predictors.
Conclusion
The predictors longitudinally associated with FNI in CN/SCF surgeries included a deep MMB-traversing approach, dislocated fracture, and female gender.
Clinical relevance
The superficial surgical approaches (i.e., transparotid, transmasseteric anteroparotid, and high perimandibular approaches) should be adopted for CN/SCF treatment to minimize postoperative morbidity, especially for female patients with dislocated condyles.

Similar content being viewed by others
References
Zachariades N, Mezitis M, Mourouzis C, Papadakis D, Spanou A (2006) Fractures of the mandibular condyle: a review of 466 cases. Literature review, reflections on treatment and proposals. J Craniomaxillofac Surg 34(7):421–432
Wang HD, Susarla SM, Mundinger GS, Schultz BD, Yang R, Bojovic B, Christy MR, Manson PN, Rodriguez ED, Dorafshar AH (2016) Which factors are associated with open reduction of adult mandibular condylar injuries? Plast Reconstr Surg 137(6):1813–1821
Schneider M, Erasmus F, Gerlach KL, Kuhlisch E, Loukota RA, Rasse M, Schubert J, Terheyden H, Eckelt U (2008) Open reduction and internal fixation versus closed treatment and mandibulomaxillary fixation of fractures of the mandibular condylar process: a randomized, prospective, multicenter study with special evaluation of fracture level. J Oral Maxillofac Surg 66(12):2537–2544
Singh V, Bhagol A, Goel M, Kumar I, Verma A (2010) Outcomes of open versus closed treatment of mandibular subcondylar fractures: a prospective randomized study. J Oral Maxillofac Surg 68(6):1304–1309
Ellis E, McFadden D, Simon P, Throckmorton G (2000) Surgical complications with open treatment of mandibular condylar process fractures. J Oral Maxillofac Surg 58(9):950–958
Al-Moraissi EA, Louvrier A, Colletti G, Wolford LM, Biglioli F, Ragaey M et al (2018) Does the surgical approach for treating mandibular condylar fractures affect the rate of seventh cranial nerve injuries? A systematic review and meta-analysis based on a new classification for surgical approaches. J Craniomaxillofac Surg 46(3):398–412
Rozeboom AVJ, Dubois L, Bos RRM, Spijker R, de Lange J (2018) Open treatment of condylar fractures via extraoral approaches: a review of complications. J Craniomaxillofac Surg 46(8):1232–1240
Imai T, Nakazawa M, Uzawa N (2019) Four-step chart of percutaneous approaches to the mandibular condyle: a proposal of a visualized system for intuitive comprehension. J Oral Maxillofac Surg 77(2):238–239
Imai T, Nakazawa M, Uzawa N (2019) Advanced model of a 4-step chart for percutaneous approaches to condylar fractures: a tool to comprehend trends in classification based on the dissection route. J Oral Maxillofac Surg 77(10):1962–1964
Ellis E, Dean J (1993) Rigid fixation of mandibular condyle fractures. Oral Surg Oral Med Oral Pathol 76(1):6–15
Chossegros C, Cheynet F, Blanc JL, Bourezak Z (1996) Short retromandibular approach of subcondylar fractures: clinical and radiologic long-term evaluation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 82(3):248–252
Spinzia A, Patrone R, Belli E, Dell'Aversana Orabona G, Ungari C, Filiaci F et al (2012) Open reduction and internal fixation of extracapsular mandibular condyle fractures: a long-term clinical and radiological follow-up of 25 patients. BMC Surg 14:68
Wilson AW, Ethunandan M, Brennan PA (2005) Transmasseteric antero-parotid approach for open reduction and internal fixation of condylar fractures. Br J Oral Maxillofac Surg 43(1):57–60
Narayanan V, Ramadorai A, Ravi P, Nirvikalpa N (2012) Transmasseteric anterior parotid approach for condylar fractures: experience of 129 cases. Br J Oral Maxillofac Surg 50(5):420–424
Wilk A, Biotchane I, Rosenstiel M, Charles X, Meyer C (1997) Osteosynthesis of subcondylar fractures using a rectangular 3-dimensional stabilization plate. Rev Stomatol Chir Maxillofac 98:40–44
Meyer C, Zink S, Chatelain B, Wilk A (2008) Clinical experience with osteosynthesis of subcondylar fractures of the mandible using TCP plates. J Craniomaxillofac Surg 36(5):260–268
Trost O, Abu El-Naaj I, Trouilloud P, Danino A, Malka G (2008) High cervical transmasseteric anteroparotid approach for open reduction and internal fixation of condylar fracture. J Oral Maxillofac Surg 66(1):201–204
Shi D, Patil PM, Gupta R (2015) Facial nerve injuries associated with the retromandibular transparotid approach for reduction and fixation of mandibular condyle fractures. J Craniomaxillofac Surg 43(3):402–407
Kanno T, Sukegawa S, Tatsumi H, Karino M, Nariai Y, Nakatani E, Furuki Y, Sekine J (2016) Does a retromandibular transparotid approach for the open treatment of condylar fractures result in facial nerve injury? J Oral Maxillofac Surg 74(10):2019–2032
Imai T, Fujita Y, Motoki A, Takaoka H, Kanesaki T, Ota Y, Iwai S, Chisoku H, Ohmae M, Sumi T, Nakazawa M, Uzawa N (2019) Surgical approaches for condylar fractures related to facial nerve injury: deep versus superficial dissection. Int J Oral Maxillofac Surg 48(9):1227–1234
Hwang M, Zebracki K, Chlan KM, Vogel LC (2014) Longitudinal changes in medical complications in adults with pediatric-onset spinal cord injury. J Spinal Cord Med 37(2):171–178
Gellrich NC, Schoen R (2012) Condyle, ascending ramus, and coronoid process fractures. In: Ehrenfeld M, Manson PN, Prein J (eds) Principles of internal fixation of the craniomaxillofacial skeleton. Thieme, New York, pp 158–167
MacLennan W (1952) Consideration of 180 cases of typical fractures of the mandibular condylar process. Br J Plast Surg 5(2):122–128
Trost O, Trouilloud P, Malka G (2009) Open reduction and internal fixation of low subcondylar fractures of mandible through high cervical transmasseteric anteroparotid approach. J Oral Maxillofac Surg 67(11):2446–2451
Hanley JA, Negassa A, Edwardes MD, Forrester JE (2003) Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol 157(4):364–375
Williamson DS, Bangdiwala SI, Marshall SW, Waller AE (1996) Repeated measures analysis of binary outcomes: applications to injury research. Accid Anal Prev 28(5):571–579
European Medicines Agency (2010) Guideline on Missing Data in Confirmatory Clinical Trials https://www.ema.europa.eu/en/missing-data-confirmatory-clinical-trials:1-12
Handschel J, Ruggeberg T, Depprich R, Schwarz F, Meyer U, Kubler NR et al (2012) Comparison of various approaches for the treatment of fractures of the mandibular condylar process. J Craniomaxillofac Surg 40(8):e397–e401
Tasanen A, Lamberg MA (1976) Transosseous wiring in the treatment of condylar fractures of the mandible. J Maxillofac Surg 4(4):200–206
Mendelson BC, Freeman ME, Wu W, Huggins RJ (2008) Surgical anatomy of the lower face: the premasseter space, the jowl, and the labiomandibular fold. Aesthet Plast Surg 32(2):185–195
Jones KJ (1993) Recovery from facial paralysis following crush injury of the facial nerve in hamsters: differential effects of gender and androgen exposure. Exp Neurol 121(1):133–138
Yoshioka I, Tanaka T, Khanal A, Habu M, Kito S, Kodama M, Oda M, Wakasugi-Sato N, Matsumoto-Takeda S, Seta Y, Tominaga K, Sakoda S, Morimoto Y (2011) Correlation of mandibular bone quality with neurosensory disturbance after sagittal split ramus osteotomy. Br J Oral Maxillofac Surg 49(7):552–556
Bruckmoser E, Bulla M, Alacamlioglu Y, Steiner I, Watzke IM (2013) Factors influencing neurosensory disturbance after bilateral sagittal split osteotomy: retrospective analysis after 6 and 12 months. Oral Surg Oral Med Oral Pathol Oral Radiol 115(4):473–482
Joss CU, Thuer UW (2007) Neurosensory and functional impairment in sagittal split osteotomies: a longitudinal and long-term follow-up study. Eur J Orthod 29(3):263–271
Monnazzi MS, Real-Gabrielli MF, Passeri LA, Gabrielli MA (2011) Cutaneous sensibility impairment after mandibular sagittal split osteotomy: a prospective clinical study of the spontaneous recovery. J Oral Maxillofac Surg 70(3):696–702
Little RJ, D'Agostino R, Cohen ML, Dickersin K, Emerson SS, Farrar JT, Frangakis C, Hogan JW, Molenberghs G, Murphy SA, Neaton JD, Rotnitzky A, Scharfstein D, Shih WJ, Siegel JP, Stern H (2012) The prevention and treatment of missing data in clinical trials. N Engl J Med 367(14):1355–1360
Coulson SE, Croxson GR, Adams RD, O'Dwyer NJ (2005) Reliability of the “Sydney,” “Sunnybrook,” and “House Brackmann” facial grading systems to assess voluntary movement and synkinesis after facial nerve paralysis. Otolaryngol Head Neck Surg 132(4):543–549
Acknowledgments
The authors thank Dr. Hiroyuki Kuragami in the Data Coordinating Center, Translational Research Center for Medical Innovation, Osaka University Hospital, for statistical consultation.
Author information
Authors and Affiliations
Contributions
Tomoaki Imai participated in all aspects of the development and completion of this research, including literature search, study design, data collection and analysis, and drafting of the manuscript. Yusei Fujita participated in literature search, data collection and analysis, and drafting of the manuscript. Hiroo Takaoka, Ayako Motoki, Tomohiko Kanesaki, Yoshiyuki Ota, and Masatoshi Ohmae collected data and critical revision of the manuscript. Hirohisa Chisoku, Tetsuro Sumi, Mitsuhiro Nakazawa, and Narikazu Uzawa contributed to data interpretation and critical revision of the manuscript. All the authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the internal review boards of Osaka University Graduate School of Dentistry and was conducted in accordance with the Declaration of Helsinki.
Informed consent
The requirement to obtain informed consent was waived by the internal review boards because of the retrospective design.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Imai, T., Fujita, Y., Takaoka, H. et al. Longitudinal study of risk for facial nerve injury in mandibular condyle fracture surgery: marginal mandibular branch-traversing classification of percutaneous approaches. Clin Oral Invest 24, 1445–1454 (2020). https://doi.org/10.1007/s00784-019-03163-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-03163-w