Abstract
Objectives
The objectives of the study are to analyze volumetric differences of condylar volumes in patients with unilateral and bilateral JIA and to compare results with control condylar volumes.
Materials and methods
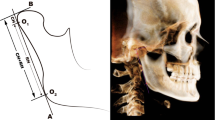
Forty-six CBCT images were analyzed for all patients affected by JIA, 37 females and 9 males (mean age 10.8 ± 4.2) with TMJ involvement (19 unilaterally, mean age 10.9 ± 4.5; 27 bilaterally, mean age 10.7 ± 4.5), and 25 CBCT of subjects without diagnosis of JIA were selected as controls (mean age 10.8 ± 4.2 years). In the case of unilateral JIA, condylar volumes and ramus lengths were compared with healthy condyle and with the compromised one. In the case of bilateral JIA, condyle volume and ramus lengths were compared with healthy one. The Shapiro-Wilk test was used to assess whether the data was normally distributed. Paired t test was applied to compare affected and non-affected condyle in the same patients (P < 0.05). Independent t test was used to evaluate whether the difference between the groups were comparable or significantly different (P < 0.05).
Results
For the unilateral JIA group, significant differences comparing affected and non-affected condyles were found. A statistically significant reduction of the volume of the head, neck, and ramus was found in the affected side (P < 0.01).
For the bilateral JIA group, statistically significant differences have been found considering the condylar head and neck, the whole condylar volume, and the ramus length compared with the control group (P < 0.05).
Conclusions
Subjects with unilateral JIA have condyles volumetrically smaller than those of the unaffected side and those found in healthy patients. A considerable decrease of the volume of all the anatomical structures considered in the patients with bilateral JIA was found compared with control group.
Clinical relevance
The study presents the effects of JIA on different anatomical structures highlighting their dimensional changes, whose sequelae are irreversible if not diagnosed and treated early.



Similar content being viewed by others
References
Giancane G, Consolaro A, Lanni S, Davì S, Schiappapietra B, Ravelli A (2016) Juvenile idiopathic arthritis: diagnosis and treatment. Rheumatol Ther 3(2):187–207
Kjellberg H, Fasth A, Kiliaridis S, Wenneberg B, Thilander B (1995) Craniofacial structure in children with juvenile chronic arthritis (JCA) compared with healthy children with ideal or postnormal occlusion. Am J Orthod Dentofac Orthop 107(1):67–78
Twilt M, Schulten AJM, Nicolaas P, Dülger A, van Suijlekom-Smit LWA (2006) Facioskeletal changes in children with juvenile idiopathic arthritis. Ann Rheum Dis 65(6):823–825
Hsieh Y-J, Darvann TA, Hermann N V, Larsen P, Liao Y-F, Kreiborg S (2019) Three-dimensional assessment of facial morphology in children and adolescents with juvenile idiopathic arthritis and moderate to severe TMJ involvement using 3D surface scans. Clin Oral Investig. https://doi.org/10.1007/s00784-019-02962-5
Farronato G, Carletti V, Maspero C, Farronato D, Giannini L, Bellintani C (2015) Craniofacial growth in children affected by juvenile idiopathic arthritis involving the temporomandibular joint: functional therapy management. J Clin Pediatr Dent 33:351–357
Billiau AD, Hu Y, Verdonck A, Carels C, Wouters C (2007) Temporomandibular joint arthritis in juvenile idiopathic arthritis: prevalence, clinical and radiological signs, and relation to dentofacial morphology. J Rheumatol 34(9):1925–1933
Ronchezel M V., Hilario MOE, Goldenberg J, Lederman HM, Faltin K, De Azevedo MF, et al (1995) Temporomandibular joint and mandibular growth alterations in patients with juvenile rheumatoid arthritis. J Rheumatol 22(10):1956–1961
Stabrun AE, Larheim TA, Höyeraal HM, Rösler M (1988) Reduced mandibular dimensions and asymmetry in juvenile rheumatoid arthritis. Pathogenetic factors. Arthritis Rheum 31(5):602–611
Hu YS, Schneiderman ED, Harper RP (1996) The temporomandibular joint in juvenile rheumatoid arthritis: part II. Relationship between computed tomographic and clinical findings. Pediatr Dent 18(4):312–319
Farronato G, Carletti V, Giannini L, Farronato D, Maspero C (2011) Juvenile idiopathic arthritis with temporomandibular joint involvement: functional treatment. Eur J Paediatr Dent 12(2):131–134
Karhulahti T, Rönning O, Jämsä T (1990) Mandibular condyle lesions, jaw movements, and occlusal status in 15-year-old children with juvenile rheumatoid arthritis. Scand J Dent Res 98(1):17–26
Garagiola U, Mercatali L, Bellintani C, Fodor A, Farronato G, Lőrincz A. (2013) Change in condylar and mandibular morphology in juvenile idiopathic arthritis: cone beam volumetric imaging 106(1):27–31.
Rönning O, Väliaho ML, Laaksonen AL (1974) The involvement of the temporomandibular joint in juvenile rheumatoid arthritis. Scand J Rheumatol 3(2):89–96
González MFO, Pedersen TK, Dalstra M, Herlin T, Verna C (2016) 3D evaluation of mandibular skeletal changes in juvenile arthritis patients treated with a distraction splint: a retrospective follow-up. Angle Orthod 86(5):846–853
Kjellberg H (1998) Craniofacial growth in juvenile chronic arthritis. Acta Odontol Scand 56(6):360–365
Huntjens E, Kiss G, Wouters C, Carels C (2008) Condylar asymmetry in children with juvenile idiopathic arthritis assessed by cone-beam computed tomography. Eur J Orthod 30(6):545–551
Koos B, Gassling V, Bott S, Tzaribachev N, Godt A (2014) Pathological changes in the TMJ and the length of the ramus in patients with confirmed juvenile idiopathic arthritis. J Craniomaxillofac Surg 42(8):1802–1807
Koos B, Twilt M, Kyank U, Fischer-Brandies H, Gassling V, Tzaribachev N (2014) Reliability of clinical symptoms in diagnosing temporomandibular joint arthritis in juvenile idiopathic arthritis. J Rheumatol 41(9):1871–1877
Keller H, Müller LM, Markic G, Schraner T, Kellenberger CJ, Saurenmann RK (2015) Is early TMJ involvement in children with juvenile idiopathic arthritis clinically detectable? Clinical examination of the TMJ in comparison with contrast enhanced MRI in patients with juvenile idiopathic arthritis. Pediatr Rheumatol Online J 13:56
Farronato G, Bellintani C, Garagiola U, Cressoni P, Sarzi Puttini P, Atzeni F et al (2014) Three-dimensional morphological condylar and mandibular changes in a patient with juvenile idiopathic arthritis: interdisciplinary treatment. Reumatismo 201466(3):254–257
De Vos W, Casselman J, Swennen GRJ (2009) Cone-beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: a systematic review of the literature. Int J Oral Maxillofac Surg 38(6):609–625
Ludlow JB, Laster WS, See M, Bailey L‘TJ, Hershey HG (2007) Accuracy of measurements of mandibular anatomy in cone beam computed tomography images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103(4):534–542
Barghan S, Merrill R, Tetradis S (2010) Cone beam computed tomography imaging in the evaluation of the temporomandibular joint. J Calif Dent Assoc 38(1):33–39
Petty RE, Southwood TR, Baum J, Bhettay E, Glass DN, Manners P, Maldonado-Cocco J, Suarez-Almazor M, Orozco-Alcala J, Prieur AM (1998) Revision of the proposed classification criteria for juvenile idiopathic arthritis: Durban, 1997. J Rheumatol 25(10):1991–1994
Tecco S, Saccucci M, Nucera R, Polimeni A, Pagnoni M, Cordasco G et al (2010) Condylar volume and surface in Caucasian young adult subjects. BMC Med Imaging 10(1):28
Schlueter B, Kim KB, Oliver D, Sortiropoulos G (2008) Cone beam computed tomography 3D reconstruction of the mandibular condyle. Angle Orthod 78(5):880–888
Kjellberg H, Ekestubbe A, Kiliaridis S, Thilander B (1994) Condylar height on panoramic radiographs. A methodologic study with a clinical application. Acta Odontol Scand 52(1):43–50
Laster WS, Ludlow JB, Bailey LJ, Hershey HG (2005) Accuracy of measurements of mandibular anatomy and prediction of asymmetry in panoramic radiographic images. Dentomaxillofac Radiol 34(6):343–349
Kambylafkas P, Murdock E, Gilda E, Tallents RH, Kyrkanides S (2006) Validity of panoramic radiographs for measuring mandibular asymmetry. Angle Orthod 76(3):388–393
Demant S, Hermann NV, Darvann TA, Zak M, Schatz H, Larsen P, Kreiborg S (2011) 3D analysis of facial asymmetry in subjects with juvenile idiopathic arthritis. Rheumatology (Oxford) 50(3):586–592
Walton AG, Welbury RR, Thomason JM, Foster HE (2000) Oral health and juvenile idiopathic arthritis: a review. Rheumatology 39(5):550–555
Kjellberg H, Kiliaridis S, Thilander B (1995) Dentofacial growth in orthodontically treated and untreated children with juvenile chronic arthritis (JCA). A comparison with Angle Class II division 1 subjects. Eur J Orthod 17(5):357–373
Larheim TA, Haanaes HR (1981) Micrognathia, temporomandibular joint changes and dental occlusion in juvenile rheumatoid arthritis of adolescents and adults. Scand J Dent Res 89(4):329–338
Stabrun AE (1991) Impaired mandibular growth and micrognathic development in children with juvenile rheumatoid arthritis. A longitudinal study of lateral cephalographs. Eur J Orthod 13(6):423–434
Pedersen TK, Küseler A, Gelineck J, Herlin T (2008) A prospective study of magnetic resonance and radiographic imaging in relation to symptoms and clinical findings of the temporomandibular joint in children with juvenile idiopathic arthritis. J Rheumatol 35(8):1668–1675
Kiliaridis S (1995) Masticatory muscle influence on craniofacial growth. Acta Odontol Scand 53(3):196–202
Stoustrup PB, Ahlefeldt-Laurvig-Lehn N, Kristensen KD, Arvidsson LZ, Twilt M, Cattaneo PM, Küseler A, Christensen AE, Herlin T, Pedersen TK (2018) No association between types of unilateral mandibular condylar abnormalities and facial asymmetry in orthopedic-treated patients with juvenile idiopathic arthritis. Am J Orthod Dentofac Orthop 153(2):214–223
Liukkonen M, Sillanmäki L, Peltomäki T (2005) Mandibular asymmetry in healthy children. Acta Odontol Scand 63(3):168–172
Türp JC, Alt KW, Vach W, Harbich K (1998) Mandibular condyles and rami are asymmetric structures. Cranio 16(1):51–56
Piancino MG, Cannavale R, Dalmasso P, Tonni I, Filipello F, Perillo L et al (2015) Condylar asymmetry in patients with juvenile idiopathic arthritis: Could it be a sign of a possible temporomandibular joints involvement? Semin Arthritis Rheum 45(2):208–213
Funding
The work was supported by the Department of Biomedical Surgical and Dental Sciences at University of Milan, Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico Milan, Italy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
A retrospective case-control study was performed analyzing CBCT of patients affected by JIA and comparing them with healthy controls. The study protocol was approved by the Ethical Committee of the Fondazione IRCCS Ca’ Granda, Ospedale Maggiore, Milan, Italy (protocol no. 573/15). This article does not contain any studies with animals performed by any of the authors. All procedures performed in this retrospective study involving human participants were in accordance with the ethical standards of the institutional and/or research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, informed consent was obtained from all individual participants or their parents, depending on their age included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Farronato, M., Cavagnetto, D., Abate, A. et al. Assessment of condylar volume and ramus height in JIA patients with unilateral and bilateral TMJ involvement: retrospective case-control study. Clin Oral Invest 24, 2635–2643 (2020). https://doi.org/10.1007/s00784-019-03122-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-03122-5