Abstract
Objectives
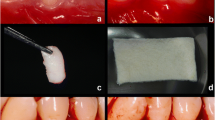
This study evaluated clinical outcomes of acellular dermal matrix (ADM) allograft compared with autogenous free gingival graft (FGG) for gingival augmentation after 15 years.
Material and methods
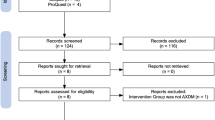
Twenty-two patients were originally included and evaluated by de Resende et al. (Clin Oral Investig 23:539–550, 2019), and 12 accepted to participate in this longitudinal evaluation. Clinical parameters evaluated were recession depth (RD), probing depth (PD), clinical attachment level (CAL), keratinized tissue width (KTW), and soft tissue thickness (TT). In addition, esthetic perception was evaluated by patients and by a calibrated periodontist. Data were evaluated by ANOVA complemented by Tukey tests (p < 0.05).
Results
After 15 years, both treatments provided a significant increase in KTW and TT but with superior results for the FGG group (p < 0.05). No differences were observed between groups for PD and CAL. In the ADM group, RD significantly increased in long term, as well as the rate of tissue contraction. The percentage of shrinkage for the ADM group was 59.6%. Conversely, the FGG group presented a creeping attachment of 17.6% and RD significantly decreased in long term. The ADM group presented superior results considering professional esthetic perception.
Conclusions
Both treatments longitudinally promoted significant gain of keratinized tissue width and thickness with superior outcomes for the FGG group. The ADM group demonstrated more tissue contraction and gingival recession whereas the FGG group presented creeping attachment. Professional esthetic perception was superior for the ADM group.
Clinical relevance
This study added important clinical data with long-term evaluation of ADM compared with FGG.

Similar content being viewed by others
References
Wei P, Laurell L, Geivelis M, Lingen MW, Maddalozzo D (2000) Acellular dermal matrix allografts to achieve increased attached gingiva. Part 1. A clinical study. J Periodontol 71:1297–1305
Nevins M, Nevins ML, Kim SW, Schupbach P, Kim DM (2011) The use of mucograft collagen matrix to augment the zone of keratinized tissue around teeth: a pilot study. Int J Periodontics Restorative Dent 31:367–373
Agarwal C, Tarun Kumar AB, Mehta DS (2015) Comparative evaluation of free gingival graft and AlloDerm(®) in enhancing the width of attached gingival: a clinical study. Contemp Clin Dent 6:483–488
Kuru B, Yildirim S (2013) Treatment of localized gingival recessions using gingival unit grafts: a randomized controlled clinical trial. J Periodontol 84(Suppl.1):S41–S50
Feitosa DS, Santamaria MP, Sallum EA, Nociti Junior FH, Casati MZ, Toledo S (2008) Indicações atuais dos enxertos gengivais libres. RGO 56(Suppl. 2):S1–S6
Björn H (1963) Free transplantation of gingiva propria. Odont Revy 14:323
Shah R, Thomas R, Mehta DS (2015) Recent modifications of free gingival graft: a case series. Contemp Clin Dent 6(Suppl.3):S425–S427
Zuhr O, Bäumer D, Hürzeler M (2014) The addition of soft tissue replacement grafts in plastic periodontal and implant surgery: critical elements in design and execution. J Clin Periodontol 41(Suppl. 15):S123–S142
Kassab M, Badawi H, Dentino A (2010) Treatment of gingival recession. Dent Clin N Am 54(Suppl.1):S129–S140
Callan DP, Silverstein LH (1998) Use of acellular dermal matrix for increasing keratinized tissue around teeth and implants. Pract Periodont Aesthet Dent 10:731–734
Hashemi H, Parhiz A, Ghafari S (2012) Vestibuloplasty: allograft versus mucosal graft. Int J Oral Maxillofac Surg 41:527–530
de Resende DRB, Greghi SLA, Siqueira AF, Benfatti CAM, Damante CA, Ragghianti Zangrando MS (2019) Acellular dermal matrix allograft versus free gingival graft: a histological evaluation and split-mouth randomized clinical trial. Clin Oral Investig 23(Suppl.2):S539–S550
Harris RJ (2001) Clinical evaluation of 3 techniques to augment keratinized tissue without root coverage. J Periodontol 72:932–938
De Resende DRB (2004) Avaliação comparativa clínica e histológica de enxertos gengivais livres autógenos e de matriz dérmica acelular alógena na criação e manutenção de uma faixa de mucosa ceratinizada em humanos. Teses Faculdade de Odontologia de Bauru, Universidade de São Paulo, Bauru (SP)
Löe H, Silness J (1963) Periodontal disease in pregnancy I. Prevalence and severity. Acta Odontol Scand 21:533–551
Silness J, Löe H (1964) Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 22:121–135
Agudio G, Chambrone L, Pini Prato G (2017) Biologic remodeling of periodontal dimensions of areas treated with gingival augmentation procedure (GAP). A 25-year follow-up observation. J Periodontol 88:634–642
Agudio G, Cortellini P, Buti J, Pini Prato G (2016) Periodontal conditions of sites treated with gingival augmentation surgery compared with untreated contralateral homologous sites: an 18-to 35-year long-term study. J Periodontol 87:1371–1378
Gapski R, Parks CA, Wang H (2005) Acellular dermal matrix for mucogingival surgery: a meta-analysis. J Periodontol 76:1814–1822
Dragan IF, Hotlzman LP, Karimbux NY, Morin RA, Bassir SH (2017) Clinical outcomes of comparing soft tissue alternatives to free gingival graft: a systematic review and meta-analysis. J Evidence Dent Pract 17(Suppl.4):S370–S380
Zucchelli G, Mele M, Stefanini M, Mazzotti C, Marzadori M, Montebugnoli L et al (2010) Patient morbidity and root coverage outcome after subepithelial connective tissue and deepithelialized grafts: a comparative randomized-controlled clinical trial. J Clin Periodontol 37(Suppl.8):S728–SS38
Zucchelli G, Marzadori M, Mele M, Stefanini M, Montebugnoli L (2012) Root coverage in molar teeth: a comparative controlled randomized clinical trial. J Clin Periodontol 39(Suppl.11):S1082–S1088
Zucchelli G, Mounssif I, Mazzotti C, Montebugnoli L, Sangiorgi M, Mele M et al (2014) Does the dimension of the graft influence patient morbidity and root coverage outcomes? A randomized controlled clinical trial. J Clin Periodontol 41(Suppl.7):S708–S716
Frost NA, Mealey BL, Jones AA, Huynh-Ba G (2010) Periodontal biotype: gingival thickness as it relates to probe visibility and buccal plate thickness. J Periodontol 86(Suppl.10):S1141–S1149
Egreja AM, Kahn S, Barceleiro M, Bittencourt S (2012) Relationship between the width of the zone of keratinized tissue and thickness of gingival tissue in the anterior maxilla. Int J Periodontics Restorative Dent 32(Suppl.5):573–579
Manjunath RGS, Rana A, Sarkar A (2015) Gingival biotype assessment in a healthy periodontium: transgingival probing method. J Clin Diagn Res 9(Suppl.5):S66–S69
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior Brasil (CAPES)-Finance code 001. Part of this study was supported by a grant (no. 99/09834-2) from FAPESP (São Paulo Research Foundation). The work was financially supported by the Department of Prosthodontics and Periodontics of Bauru School of Dentistry, University of São Paulo, Brazil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cevallos, C.A.R., de Resende, D.R.B., Damante, C.A. et al. Free gingival graft and acellular dermal matrix for gingival augmentation: a 15-year clinical study. Clin Oral Invest 24, 1197–1203 (2020). https://doi.org/10.1007/s00784-019-02983-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02983-0