Abstract
Objectives
The aim of this study was to investigate in vitro the effect of clodronate on interleukin-1ß (IL-1ß)–stimulated human periodontal ligament fibroblasts (HPdLFs) with the focus on inflammatory factors of orthodontic tooth movement with and without compressive force.
Materials and methods
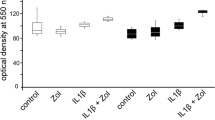
HPdLFs were incubated with 5 μM clodronate and 10 ng/mL IL-1ß. After 48 h, cells were exposed to 3 h of compressive force using a centrifuge. The gene expression of cyclooxygenase-2 (COX-2), interleukin-6 (IL-6), matrix metalloproteinase 8 (MMP-8), and the tissue inhibitor of MMP (TIMP-1) was analyzed using RT-PCR. Prostaglandin E2 (PGE-2), IL-6, and TIMP-1 protein syntheses were quantified via ELISA.
Results
Compressive force and IL-1ß induced an overexpression of COX-2 gene expression (61.8-fold; p < 0.05 compared with control), diminished by clodronate (41.1-fold; p < 0.05 compared with control). Clodronate slowed down the compression and IL-1ß induced IL-6 gene expression (161-fold vs. 85.6-fold; p < 0.05 compared with control). TNF-α was only slightly affected without statistical significance. Clodronate reduced IL-1ß-stimulated MMP-8 expression with and without compressive force. TIMP-1 on gene and protein level was downregulated in all groups. Analyzing the MMP-8/TIMP-1 ratio, the highest ratio was detected in IL-1ß-stimulated HPdLFs with compressive force (21.2-fold; p < 0.05 compared with control). Clodronate diminished IL-1ß-induced upregulation of MMP-8/TIMP-1 ratio with (11.5-fold; p < 0.05 compared with control) and without (12.5-fold; p < 0.05 compared with control) compressive force.
Conclusion
Our study demonstrates a slightly anti-inflammatory effect by clodronate under compressive force in vitro. Additionally, the periodontal remodeling presented by the MMP-8/TIMP-1 ratio seems to be diminished by clodronate.
Clinical relevance
Reduction of pro-inflammatory factors and reduction of periodontal remodeling might explain reduced orthodontic tooth movement under clodronate intake.



Similar content being viewed by others
References
Lekic PC, Rajshankar D, Chen H, Tenenbaum H, McCulloch CA (2001) Transplantation of labeled periodontal ligament cells promotes regeneration of alveolar bone. Anat Rec 262:193–202
Saito M, Saito S, Ngan PW, Shanfeld J, Davidovitch Z (1991) Interleukin 1 beta and prostaglandin E are involved in the response of periodontal cells to mechanical stress in vivo and in vitro. Am J Orthod Dentofac Orthop 99:226–240
Jager A, Zhang D, Kawarizadeh A, Tolba R, Braumann B, Lossdorfer S, Gotz W (2005) Soluble cytokine receptor treatment in experimental orthodontic tooth movement in the rat. Eur J Orthod 27:1–11
Nunes L, Quintanilha L, Perinetti G, Capelli JJ (2017) Effect of orthodontic force on expression levels of ten cytokines in gingival crevicular fluid. Arch Oral Biol 76:70–75
Surlin P, Rauten AM, Mogoanta L, Silosi I, Oprea B, Pirici D (2010) Correlations between the gingival crevicular fluid MMP8 levels and gingival overgrowth in patients with fixed orthodontic devices. Romanian J Morphol Embryol 51:515–519
Grieve WG 3rd, Johnson GK, Moore RN, Reinhardt RA, DuBois LM (1994) Prostaglandin E (PGE) and interleukin-1 beta (IL-1 beta) levels in gingival crevicular fluid during human orthodontic tooth movement. Am J Orthod Dentofac Orthop 105:369–374
Scott P, Fleming P, DiBiase A (2007) An update in adult orthodontics. Dent Update 34:427–428, 431-4, 436 passim
Rogers MJ (2003) New insights into the molecular mechanisms of action of bisphosphonates. Curr Pharm Des 9:2643–2658
Schenk R, Merz WA, Muhlbauer R, Russell RG, Fleisch H (1973) Effect of ethane-1-hydroxy-1,1-diphosphonate (EHDP) and dichloromethylene diphosphonate (Cl 2 MDP) on the calcification and resorption of cartilage and bone in the tibial epiphysis and metaphysis of rats. Calcif Tissue Res 11:196–214
Jacobs C, Walter C, Ziebart T, Dirks I, Schramm S, Grimm S, Krieger E, Wehrbein H (2014) Mechanical loading influences the effects of bisphosphonates on human periodontal ligament fibroblasts. Clin Oral Investig 19:699–708
Walter C, Klein MO, Pabst A, Al-Nawas B, Duschner H, Ziebart T (2010) Influence of bisphosphonates on endothelial cells, fibroblasts, and osteogenic cells. Clin Oral Investig 14:35–41
Saviola G, Abdi-Ali L, Campostrini L, Sacco S, Baiardi P, Manfredi M, Mannoni A, Benucci M (2012) Clodronate and hydroxychloroquine in erosive osteoarthritis: a 24-month open randomized pilot study. Mod Rheumatol 22:256–263
Zhang JX, Dang SC, Yin K, Jiang DL (2011) Protective effect of clodronate-containing liposomes on intestinal mucosal injury in rats with severe acute pancreatitis. Hepatobiliary Pancreat Dis Int 10:544–551
Llavaneras A, Ramamurthy NS, Heikkila P, Teronen O, Salo T, Rifkin BR, Ryan ME, Golub LM, Sorsa T (2001) A combination of a chemically modified doxycycline and a bisphosphonate synergistically inhibits endotoxin-induced periodontal breakdown in rats. J Periodontol 72:1069–1077
Dombrecht EJ, Schuerwegh AJ, Bridts CH, Ebo DG, Van Offel JF, Stevens WJ, De Clerck LS (2007) Effect of bisphosphonates on nitric oxide production by inflammatory activated chondrocytes. Clin Exp Rheumatol 25:817–822
Ozdemir SP, Kurtis B, Tuter G, Bozkurt S, Gultekin SE, Senguven B, Watanabe K, Aydin S (2012) Effects of low-dose doxycycline and bisphosphonate clodronate on alveolar bone loss and gingival levels of matrix metalloproteinase-9 and interleukin-1beta in rats with diabetes: a histomorphometric and immunohistochemical study. J Periodontol 83:1172–1182
Dehghani F, Conrad A, Kohl A, Korf HW, Hailer NP (2004) Clodronate inhibits the secretion of proinflammatory cytokines and NO by isolated microglial cells and reduces the number of proliferating glial cells in excitotoxically injured organotypic hippocampal slice cultures. Exp Neurol 189:241–251
Choi J, Baek SH, Lee JI, Chang YI (2010) Effects of clodronate on early alveolar bone remodeling and root resorption related to orthodontic forces: a histomorphometric analysis. Am J Orthod Dentofac Orthop 138:548 e1–548 e8 discussion 548-9
Liu L, Igarashi K, Haruyama N, Saeki S, Shinoda H, Mitani H (2004) Effects of local administration of clodronate on orthodontic tooth movement and root resorption in rats. Eur J Orthod 26:469–473
Lotwala RB, Greenlee GM, Ott SM, Hall SH, Huang GJ (2012) Bisphosphonates as a risk factor for adverse orthodontic outcomes: a retrospective cohort study. Am J Orthod Dentofac Orthop 142:625–634 e3
Liu L, Igarashi K, Kanzaki H, Chiba M, Shinoda H, Mitani H (2006) Clodronate inhibits PGE(2) production in compressed periodontal ligament cells. J Dent Res 85:757–760
Proff P, Reicheneder C, Faltermeier A, Kubein-Meesenburg D, Romer P (2014) Effects of mechanical and bacterial stressors on cytokine and growth-factor expression in periodontal ligament cells. J Orofac Orthop 75:191–202
Nokhbehsaim M, Winter J, Rath B, Jager A, Jepsen S, Deschner J (2011) Effects of enamel matrix derivative on periodontal wound healing in an inflammatory environment in vitro. J Clin Periodontol 38:479–490
Jacobs C, Schramm S, Dirks I, Walter C, Pabst A, Meila D, Jacobs C, Wehrbein H (2018) Mechanical loading increases pro-inflammatory effects of nitrogen-containing bisphosphonate in human periodontal fibroblasts. Clin Oral Investig 22:901–907
Long P, Liu F, Piesco NP, Kapur R, Agarwal S (2002) Signaling by mechanical strain involves transcriptional regulation of proinflammatory genes in human periodontal ligament cells in vitro. Bone 30:547–552
Walter C, Pabst A, Ziebart T, Klein M, Al-Nawas B (2011) Bisphosphonates affect migration ability and cell viability of HUVEC, fibroblasts and osteoblasts in vitro. Oral Dis 17:194–199
Pabst AM, Ziebart T, Koch FP, Taylor KY, Al-Nawas B, Walter C (2012) The influence of bisphosphonates on viability, migration, and apoptosis of human oral keratinocytes--in vitro study. Clin Oral Investig 16:87–93
Grimm S, Walter C, Pabst A, Goldschmitt J, Wehrbein H, Jacobs C (2015) Effect of compressive loading and incubation with clodronate on the RANKL/OPG system of human osteoblasts. J Orofac Orthop 76:531–542
Diercke K, Zingler S, Kohl A, Lux CJ, Erber R (2014) Gene expression profile of compressed primary human cementoblasts before and after IL-1beta stimulation. Clin Oral Investig 18:1925–1939
Redlich M, Roos H, Reichenberg E, Zaks B, Grosskop A, Bar Kana I, Pitaru S, Palmon A (2004) The effect of centrifugal force on mRNA levels of collagenase, collagen type-I, tissue inhibitors of metalloproteinases and beta-actin in cultured human periodontal ligament fibroblasts. J Periodontal Res 39:27–32
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25:402–408
Meeran NA (2013) Cellular response within the periodontal ligament on application of orthodontic forces. J Indian Soc Periodontol 17:16–20
Mitsui N, Suzuki N, Maeno M, Yanagisawa M, Koyama Y, Otsuka K, Shimizu N (2006) Optimal compressive force induces bone formation via increasing bone morphogenetic proteins production and decreasing their antagonists production by Saos-2 cells. Life Sci 78:2697–2706
Bartzela T, Turp JC, Motschall E, Maltha JC (2009) Medication effects on the rate of orthodontic tooth movement: a systematic literature review. Am J Orthod Dentofac Orthop 135:16–26
Shima K, Nemoto W, Tsuchiya M, Tan-No K, Takano-Yamamoto T, Sugawara S, Endo Y (2016) The bisphosphonates clodronate and etidronate exert analgesic effects by acting on glutamate- and/or ATP-related pain transmission pathways. Biol Pharm Bull 39:770–777
Jiang L, Tang Z (2018) Expression and regulation of the ERK1/2 and p38 MAPK signaling pathways in periodontal tissue remodeling of orthodontic tooth movement. Mol Med Rep 17:1499–1506
Ren Y, Hazemeijer H, de Haan B, Qu N, de Vos P (2007) Cytokine profiles in crevicular fluid during orthodontic tooth movement of short and long durations. J Periodontol 78:453–458
Garlet TP, Coelho U, Silva JS, Garlet GP (2007) Cytokine expression pattern in compression and tension sides of the periodontal ligament during orthodontic tooth movement in humans. Eur J Oral Sci 115:355–362
Alhashimi N, Frithiof L, Brudvik P, Bakhiet M (2001) Orthodontic tooth movement and de novo synthesis of proinflammatory cytokines. Am J Orthod Dentofac Orthop 119:307–312
Taddei SR, Moura AP, Andrade I Jr, Garlet GP, Garlet TP, Teixeira MM, da Silva TA (2012) Experimental model of tooth movement in mice: a standardized protocol for studying bone remodeling under compression and tensile strains. J Biomech 45:2729–2735
Apajalahti S, Sorsa T, Railavo S, Ingman T (2003) The in vivo levels of matrix metalloproteinase-1 and -8 in gingival crevicular fluid during initial orthodontic tooth movement. J Dent Res 82:1018–1022
Jacobs C, Walter C, Ziebart T, Grimm S, Meila D, Krieger E, Wehrbein H (2013) Induction of IL-6 and MMP-8 in human periodontal fibroblasts by static tensile strain. Clin Oral Investig 18:901–908
Funding
The work was supported by the Osteology Foundation (Lucerne, Switzerland).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Grimm, S., Wolff, E., Walter, C. et al. Influence of clodronate and compressive force on IL-1ß-stimulated human periodontal ligament fibroblasts. Clin Oral Invest 24, 343–350 (2020). https://doi.org/10.1007/s00784-019-02930-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02930-z