Abstract
Purpose
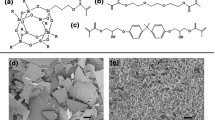
To determine the effect of aging methods on the fracture toughness of a conventional Bis-GMA-based resin composite (Filtek Supreme), an ormocer-based resin composite (Admira), and an experimental hydrophobic oxirane/acrylate interpenetrating network resin system (OASys)-based composite.
Methods
A 25 × 5 × 2.8-mm stainless-steel mold with 2.5 mm single-edge center notch, following ASTM standards [E399-90], was used to fabricate 135 specimens (n = 15) of the composite materials and randomly distributed into groups. For the baseline group, specimens were fabricated and then tested after 24-h storage in water. For the biofilm challenge, specimens were randomly placed in a six-well tissue culture plate and kept at 37 °C with bacterial growth media (Brain Heart Infusion (BHI); Streptococcus mutans) changed daily for 15 days. For the water storage challenge, specimens were kept in 5 ml of deionized distilled autoclaved water for 30 days at 37 °C. μCT evaluation by scanning the specimens was performed before and after the proposed challenge. Fracture toughness (KIc) testing was carried out following the challenges.
Results
μCT surface area and volume analyses showed no significant changes regardless of the materials tested or the challenge. Filtek and Admira fracture toughness was significantly lower after the biofilm and water storage challenges. OASys mean fracture toughness values after water aging were significantly higher than that of baseline. Toughness values for OASys composites after biofilm aging were not statistically different when compared to either water or baseline values.
Conclusion
The fracture toughness of Bis-GMA and ormocer-based dental resin composites significantly decreased under water and bacterial biofilm assault. However, such degradation in fracture toughness was not visible in OASys-based composites.
Clinical significance
Current commercial dental composites are affected by the oral environment, which might contribute to the long-term performance of these materials.

Similar content being viewed by others
References
Heintze SD, Ilie N, Hickel R, Reis A, Loguercio A, Rousson V (2017) Laboratory mechanical parameters of composite resins and their relation to fractures and wear in clinical trials-a systematic review. Dent Mater 33:e101–e114. https://doi.org/10.1016/j.dental.2016.11.013
Ferracane JL (2013) Resin-based composite performance: are there some things we can’t predict? Dent Mater 29:51–58. https://doi.org/10.1016/j.dental.2012.06.013
Martos J, Osinaga PWR, Oliveira E, Castro LAS (2003) Hydrolytic degradation of composite resins: effects on the microhardness. Mater Res 6:99–604
Arikawa H, Kuwahata H, Seki H, Kanie T, Fujii K, Inoue K (1995) Deterioration of mechanical properties of composite resins. Dent Mater J 14:78–83
Tjaderhane L, Nascimento FD, Breschi L, Mazzoni A, Tersariol IL, Geraldeli S, Tezvergil-Mutluay A, Carrilho M, Carvalho RM, Tay FR, Pashley DH (2013) Strategies to prevent hydrolytic degradation of the hybrid layer-a review. Dent Mater 29:999–1011. https://doi.org/10.1016/j.dental.2013.07.016
Ferracane JL, Condon JR (1999) In vitro evaluation of the marginal degradation of dental composites under simulated occlusal loading. Dent Mater 15:262–267
Suiter EA, Watson LE, Tantbirojn D, Lou JS, Versluis A (2016) Effective expansion: balance between shrinkage and hygroscopic expansion. J Dent Res 95:543–549. https://doi.org/10.1177/0022034516633450
Ferracane JL (1994) Elution of leachable components from composites. J Oral Rehabil 21:441–452
Ferracane JL, Condon JR (1990) Rate of elution of leachable components from composite. Dent Mater 6:282–287. https://doi.org/10.1016/s0109-5641(05)80012-0
Busscher HJ, Rinastiti M, Siswomihardjo W, van der Mei HC (2010) Biofilm formation on dental restorative and implant materials. J Dent Res 89:657–665. https://doi.org/10.1177/0022034510368644
Fucio SB, Carvalho FG, Sobrinho LC, Sinhoreti MA, Puppin-Rontani RM (2008) The influence of 30-day-old Streptococcus mutans biofilm on the surface of esthetic restorative materials--an in vitro study. J Dent 36:833–839. https://doi.org/10.1016/j.jdent.2008.06.002
Beyth N, Bahir R, Matalon S, Domb AJ, Weiss EI (2008) Streptococcus mutans biofilm changes surface-topography of resin composites. Dent Mater 24:732–736. https://doi.org/10.1016/j.dental.2007.08.003
Kalra S, Singh A, Gupta M, Chadha V (2012) Ormocer: an aesthetic direct restorative material; an in vitro study comparing the marginal sealing ability of organically modified ceramics and a hybrid composite using an ormocer-based bonding agent and a conventional fifth-generation bonding agent. Contemp Clin Dent 3:48–53. https://doi.org/10.4103/0976-237x.94546
Cavalcante LM, Schneider LF, Silikas N, Watts DC (2011) Surface integrity of solvent-challenged ormocer-matrix composite. Dent Mater 27:173–179. https://doi.org/10.1016/j.dental.2010.10.002
Monsarrat P, Garnier S, Vergnes JN, Nasr K, Grosgogeat B, Joniot S (2017) Survival of directly placed ormocer-based restorative materials: a systematic review and meta-analysis of clinical trials. Dent Mater 33:e212–e220. https://doi.org/10.1016/j.dental.2017.01.019
Rawls HR JAD, Norling BK, Whang K (2015) Restorative resin compositions and methods of use, WIPO patent WO20151557329A1
Danso RMA, Oldham M, Whang K, Wendt S, Johnston A, Ralph HR (2017) A hydrophobic composite based on an Oxirane/Acrylate Interpenetrating Network. J Dent Res 96(A):3014
Ilie N, Hickel R, Valceanu AS, Huth KC (2012) Fracture toughness of dental restorative materials. Clin Oral Investig 16:489–498. https://doi.org/10.1007/s00784-011-0525-z
Lin L, Drummond JL (2010) Cyclic loading of notched dental composite specimens. Dent Mater 26:207–214. https://doi.org/10.1016/j.dental.2009.10.002
ASTM Standard E399-90 A (1997) Standard test method for plane-strain fracture toughness of metallic materials. ASTM International, West Conshohocken, PA, 2003 www.astm.org
Jain A (2016) A biofilm-based aging model for testing degradation of dental adhesive microtensile bond strength. University of Iowa, Iowa Research Online
Drummond JL (2008) Degradation, fatigue, and failure of resin dental composite materials. J Dent Res 87:710–719. https://doi.org/10.1177/154405910808700802
Mese A, Ea Palamara J, Bagheri R, Fani M, Burrow MF (2016) Fracture toughness of seven resin composites evaluated by three methods of mode I fracture toughness (KIc). Dent Mater J 35:893–899. https://doi.org/10.4012/dmj.2016-140
Thomaidis S, Kakaboura A, Mueller WD, Zinelis S (2013) Mechanical properties of contemporary composite resins and their interrelations. Dent Mater 29:e132–e141. https://doi.org/10.1016/j.dental.2013.04.025
Sookhakiyan M, Tavana S, Azarnia Y, Bagheri R (2017) Fracture toughness of nanohybrid and hybrid composites stored wet and dry up to 60 days. J Dent Biomater 4:341–346
Elbishari H, Silikas N, Satterthwaite J (2012) Filler size of resin-composites, percentage of voids and fracture toughness: is there a correlation? Dent Mater J 31:523–527
Watanabe H, Khera SC, Vargas MA, Qian F (2008) Fracture toughness comparison of six resin composites. Dent Mater 24:418–425. https://doi.org/10.1016/j.dental.2007.06.018
Lohbauer U, Belli R, Ferracane JL (2013) Factors involved in mechanical fatigue degradation of dental resin composites. J Dent Res 92:584–591. https://doi.org/10.1177/0022034513490734
Apel E, Deubener J, Bernard A, Holand M, Muller R, Kappert H, Rheinberger V, Holand W (2008) Phenomena and mechanisms of crack propagation in glass-ceramics. J Mech Behav Biomed Mater 1:313–325. https://doi.org/10.1016/j.jmbbm.2007.11.005
Bijelic-Donova J, Garoushi S, Lassila LV, Keulemans F, Vallittu PK (2016) Mechanical and structural characterization of discontinuous fiber-reinforced dental resin composite. J Dent 52:70–78. https://doi.org/10.1016/j.jdent.2016.07.009
Ferracane JL, Marker VA (1992) Solvent degradation and reduced fracture toughness in aged composites. J Dent Res 71:13–19. https://doi.org/10.1177/00220345920710010101
Musanje L, Shu M, Darvell BW (2001) Water sorption and mechanical behaviour of cosmetic direct restorative materials in artificial saliva. Dent Mater 17:394–401
Al Sunbul H, Silikas N, Watts DC (2015) Resin-based composites show similar kinetic profiles for dimensional change and recovery with solvent storage. Dent Mater 31:e201–e217. https://doi.org/10.1016/j.dental.2015.06.003
Ilie N, Hickel R (2009) Macro-, micro- and nano-mechanical investigations on silorane and methacrylate-based composites. Dent Mater 25:810–819. https://doi.org/10.1016/j.dental.2009.02.005
Delaviz Y, Finer Y, Santerre JP (2014) Biodegradation of resin composites and adhesives by oral bacteria and saliva: a rationale for new material designs that consider the clinical environment and treatment challenges. Dent Mater 30:16–32. https://doi.org/10.1016/j.dental.2013.08.201
Nedeljkovic I, De Munck J, Ungureanu AA, Slomka V, Bartic C, Vananroye A, Clasen C, Teughels W, Van Meerbeek B, Van Landuyt KL (2017) Biofilm-induced changes to the composite surface. J Dent 63:36–43. https://doi.org/10.1016/j.jdent.2017.05.015
Hahnel S, Muhlbauer G, Hoffmann J, Ionescu A, Burgers R, Rosentritt M, Handel G, Haberlein I (2012) Streptococcus mutans and Streptococcus sobrinus biofilm formation and metabolic activity on dental materials. Acta Odontol Scand 70:114–121. https://doi.org/10.3109/00016357.2011.600703
Napimoga MH, Hofling JF, Klein MI, Kamiya RU, Goncalves RB (2005) Tansmission, diversity and virulence factors of Sreptococcus mutans genotypes. J Oral Sci 47:59–64
Zhou X, Wang S, Peng X, Hu Y, Ren B, Li M, Hao L, Feng M, Cheng L, Zhou X (2018) Effects of water and microbial-based aging on the performance of three dental restorative materials. J Mech Behav Biomed Mater 80:42–50. https://doi.org/10.1016/j.jmbbm.2018.01.023
Swain MV, Xue J (2009) State of the art of micro-CT applications in dental research. Int J Oral Sci 1:177–188. https://doi.org/10.4248/ijos09031
Yoshikawa T, Sadr A, Tagami J (2017) MicroCT-3D visualization analysis of resin composite polymerization and dye penetration test of composite adaptation. Dent Mater J 37:71–77. https://doi.org/10.4012/dmj.2016-323
Hirata R, Clozza E, Giannini M, Farrokhmanesh E, Janal M, Tovar N, Bonfante EA, Coelho PG (2015) Shrinkage assessment of low shrinkage composites using micro-computed tomography. J Biomed Mater Res B Appl Biomater 103:798–806. https://doi.org/10.1002/jbm.b.33258
Zeiger DN, Sun J, Schumacher GE, Lin-Gibson S (2009) Evaluation of dental composite shrinkage and leakage in extracted teeth using X-ray microcomputed tomography. Dent Mater 25:1213–1220. https://doi.org/10.1016/j.dental.2009.04.007
Prager M, Pierce M, Atria PJ, Sampaio C, Caceres E, Wolff M, Giannini M, Hirata R (2018) Assessment of cuspal deflection and volumetric shrinkage of different bulk fill composites using non-contact phase microscopy and micro-computed tomography. Dent Mater J 37:393–399. https://doi.org/10.4012/dmj.2017-136
Soderholm KJ (1984) Water sorption in a bis(GMA)/TEGDMA resin. J Biomed Mater Res 18:271–279. https://doi.org/10.1002/jbm.820180304
Boaro LC, Goncalves F, Guimaraes TC, Ferracane JL, Pfeifer CS, Braga RR (2013) Sorption, solubility, shrinkage and mechanical properties of “low-shrinkage” commercial resin composites. Dent Mater 29:398–404. https://doi.org/10.1016/j.dental.2013.01.006
Funding
This work was partially supported by the National Institutes of Health [NIH/NIDCR Grant U01 DE23778].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Algamaiah, H., Danso, R., Banas, J. et al. The effect of aging methods on the fracture toughness and physical stability of an oxirane/acrylate, ormocer, and Bis-GMA-based resin composites. Clin Oral Invest 24, 369–375 (2020). https://doi.org/10.1007/s00784-019-02912-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02912-1