Abstract
Objectives
Oromandibular dystonia, which is characterized by stereotypic, task-specific, or sustained contractions of masticatory and/or lingual muscles, is frequently misdiagnosed as temporomandibular disorders or psychogenic disease. Diagnostic delay in oromandibular dystonia is not acceptable; thus, a screening tool that can distinguish this condition from a temporomandibular disorder may be helpful for medical professionals unfamiliar with involuntary movements or temporomandibular disorders.
Materials and methods
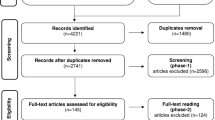
A questionnaire that included questions on the clinical features of oromandibular dystonia, such as stereotypy, task-specificity, sensory tricks, and morning benefit, and included questions to rule out temporomandibular disorders (total point range 0–40) was administered to 553 patients suspected to have involuntary movements.
Results
Based on a careful examination and the differential diagnosis, the patients were divided into four groups: oromandibular dystonia (n = 385), oral dyskinesia (n = 84), psychogenic (functional) movement disorder (n = 50), and temporomandibular disorders (n = 34). The questionnaire had a high level of internal consistency as measured by the Cronbach’s α (0.91), and item-total correlation was significant (p < 0.001). The test-retest reliability on two separate occasions showed a significant correlation (p < 0.001). Mean total scores of the questionnaire significantly differed among oromandibular dystonia (32.0), temporomandibular disorders (10.4; one-way analysis of variance, p < 0.001), oral dyskinesia (21.0; p < 0.001), and psychogenic (functional) movement disorder (13.7; p < 0.001).
Conclusions
Findings of this study suggest that the present questionnaire is a simple diagnostic tool that is useful for tentative differentiation of oromandibular dystonia from temporomandibular disorders.
Clinical relevance
This screening tool can be used to distinguish oromandibular dystonia from temporomandibular disorders.

Similar content being viewed by others
References
Albanese A, Bhatia K, Bressman SB, DeLong MR, Fahn S, Fung VSC, Hallett M, Jankovic J, Jinnah HA, Klein C, Lang AE, Mink JW, Teller JK (2013) Phenomenology and classification of dystonia: a consensus up date. Mov Disord 28:863–873. https://doi.org/10.1002/mds.25475
Yoshida K, Kaji R, Kubori T, Kohara N, Iizuka T, Kimura J (1998) Muscle afferent block for the treatment of oromandibular dystonia. Mov Disord 13:699–705. https://doi.org/10.1002/mds.870130416
Yoshida K, Kaji R, Shibasaki H, Iizuka T (2002) Factors influencing the therapeutic effect of muscle afferent block for oromandibular dystonia and dyskinesia: implications for their distinct pathophysiology. Int J Oral Maxillofac Surg 31:499–505. https://doi.org/10.1054/ijom.2002.0291
Sinclair CF, Gurey LE, Blitzer A (2013) Oromandibular dystonia: long-term management with botulinum toxin. Laryngoscope 123:3078–3083. https://doi.org/10.1002/lary.23265
Yoshida K (2017) Clinical and phenomelogical characteristics of patients with task-specific lingual dystonia: possible association with occupation. Front Neurol 8:649. https://doi.org/10.3389/fneur.2017.00649
Yoshida K, Kaji R, Kohara N, Murase N, Ikeda A, Shibasaki H, Iizuka T (2003) Movement-related cortical potentials before jaw excursions in patients with oromandibular dystonia. Mov Disord 18:94–100. https://doi.org/10.1002/mds.10296
Yoshida K, Iizuka T (2006) Botulinum toxin treatment for upper airway collapse resulting from temporomandibular joint dislocation due to jaw-opening dystonia. Cranio 24:217–222. https://doi.org/10.1179/crn.2006.035
Yoshida K (2017) How do I inject botulinum toxin into the lateral and medial pterygoid muscles? Mov Disord Clin Pract 4:285. https://doi.org/10.1002/mdc3.12460
Yoshida K (2018) Computer-aided design/computer-aided manufacturing-derived needle guide for injection of botulinum toxin into the lateral pterygoid muscle in patients with oromandibular dystonia. J Oral Facial Pain Headache (in press)
Yoshida K (2018) Sensory trick splint as a multimodal therapy for oromandibular dystonia. J Prosthodont Res 62:239–244. https://doi.org/10.1016/j.jpor.2017.09.004
Yoshida K (2006) Coronoidotomy as treatment for trismus due to jaw-closing oromandibular dystonia. Mov Disord 21:1028–1031. https://doi.org/10.1002/mds.20859
Yoshida K (2017) Surgical intervention for oromandibular dystonia-related limited mouth opening: long-term follow-up. J Craniomaxillofac Surg 45:56–62. https://doi.org/10.1016/j.jcms.2016.10.009
Macerollo A, Superbo M, Gigante AF, Livrea P, Defazio G (2015) Diagnostic delay in adult-onset dystonia: data from an Italian movement disorder center. J Clin Neurosci 22:608–610. https://doi.org/10.1016/j.jocn.2014.09.014
Powell AT, Bidewell JW, Walker AC (1995) Diagnosing idiopathic dystonia: must it take so long? Aust Health Rev 18:120–131
Jog M, Chouinard S, Hobson D, Grimes D, Chen R, Bhogal M, Simonyi S (2011) Causes for treatment delays in dystonia and hemifacial spasm: a Canadian survey. Can J Neurol Sci 38:704–711
Tiderington E, Goodman EM, Rosen AR, Hapner ER, Johns MM 3rd, Evatt ML, Freeman A, Factor S, Jinnah HA (2013) How long does it take to diagnose cervical dystonia? J Neurol Sci 335:72–74. https://doi.org/10.1016/j.jns.2013.08.028
Bertram KL, Williams DR (2016) Delays to the diagnosis of cervical dystonia. J Clin Neurosci 25:62–64. https://doi.org/10.1016/j.jocn.2015.05.054
Streiner DL, Norman GR, Cairney J (2015) Health measurement scales: a practical guide to their development and use, 5th edn. Oxford University Press, Oxford
Merz RI, Deakin J, Hawthorne MR (2010) Oromandibular dystonia questionnaire (OMDQ-25): a valid and reliable instrument for measuring health-related quality of life. Clin Otolaryngol 35:390–396. https://doi.org/10.1111/j.1749-4486.2010.02194.x
Albanese A, Sorbo FD, Comella C, Jinnah HA, Mink JW, Post B, Vidailhet M, Volkmann J, Warner TT, Leentjens AF, Martinez-Martin P, Stebbins GT, Goetz CG, Schrag A (2013) Dystoniaratingscales: critique and recommendations. Mov Disord 28:874–883. https://doi.org/10.1002/mds.25579
Defazio G, Hallett M, Jinnah HA, Stebbins GT, Gigante AF, Ferrazzano G, Conte A, Fabbrini G, Berardelli A (2015) Development and validation of a clinical scale for rating the severity of blepharospasm. Mov Disord 30:525–530. https://doi.org/10.1002/mds.26156
Comella CL, Fox SH, Bhatia KP, Perlmutter JS, Jinnah HA, Zurowski M, McDonald WM, Marsh L, Rosen AR, Waliczek T, Wright LJ, Galpern WR, Stebbins GT (2015) Development of the comprehensive cervical dystonia rating scale: methodology. Mov Disord Clin Pract 2:135–141. https://doi.org/10.1002/mdc3.12131
Thenganatt MA, Jankovic J (2015) Psychogenicmovement disorders. Neurol Clin 33:205–224. https://doi.org/10.1016/j.ncl.2014.09.013
Hallett M (2016) Functional (psychogenic) movement disorders—clinical presentations. Parkinsonism Relat Disord 22:S149–S152. https://doi.org/10.1016/j.parkreldis.2015.08.036
Schiffman R, Ohrbach E, Truelove E, Look J, Anderson G, Goulet JP, List T, Svensson P, Gonzalez Y, Lobbezoo F, Michelotti A, Brooks SL, Ceusters W, Drangsholt M, Ettlin D, Gaul C, Goldberg LJ, Haythornthwaite JA, Hollender L, Jensen R, John MT, De Laat A, de Leeuw R, Maixner W, van der Meulen M, Murray GM, Nixdorf DR, Palla S, Petersson A, Pionchon P, Smith B, Visscher CM, Zakrzewska J, Dworkin SF (2014) Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache 28:6–27. https://doi.org/10.11607/jop.1151
Müller J, Wissel J, Kemmler G, Voller B, Bodner T, Schneider A, Wenning GK, Poewe W (2004) Craniocervical dystonia questionnaire (CDQ-24): development and validation of a disease-specific quality of life instrument. J Neurol Neurosurg Psychiatry 75:749–753
Nutt JG, Muenter MD, Aronson A, Kurland LT, Melton LJ 3rd (1988) Epidemiology of focal and generalized dystonia in Rochester, Minnesota. Mov Disord 3:188–194. https://doi.org/10.1002/mds.870030302
Yoshida K (2018) Involuntary movements of the stomatognathic region. https://sites.google.com/site/oromandibulardystoniaenglish/ Accessed 14 March, 2018
Yoshida K (2018) Multilingual website and cyber consultations for oromandibular dystonia. Neurol Int 10:7536. https://doi.org/10.4081/ni.2018.7536
Funding
This study was supported by grants from the Japanese Ministry of Health, Labor, and Welfare (24592946 and 22111201).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflict of interest.
Ethical approval
This study was performed in accordance with the Declaration of Helsinki under the approval of the institutional review board and ethics committee of Kyoto Medical Center.
Rights and permissions
About this article
Cite this article
Yoshida, K. Oromandibular dystonia screening questionnaire for differential diagnosis. Clin Oral Invest 23, 405–411 (2019). https://doi.org/10.1007/s00784-018-2449-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2449-3