Abstract
Objectives
The objective of this study was to evaluate the accuracy of different impression techniques on multiple implants.
Material and methods
A master cast simulating a jaw with four implants was used.
Eight impression techniques were tested: open tray-polyether#1, open tray plus splint of impression copings with acrylic resin-polyether#1, closed tray-polyether#1, open tray-polyether#2, open tray-splint-polyether#2, closed tray-polyether#2, open tray-impression plaster, and digital impression (DI).
Five impressions of the master cast were taken with each traditional impression (TI) technique, pouring 35 sample casts. Three different clinicians took 5 DI each (n = 15).
A three-dimensional coordinate measurement machine (CMM) was used to measure implant angulation and inter-implant distances on TI casts. TI data and DI Standard Tessellation Language datasets were compared with the master cast.
The best and the worst impressions made with TI and DI were selected to fabricate four milled titanium frameworks. Passive fit was evaluated through Sheffield test, screwing each framework on the master cast. Gaps between framework-implant analogs were measured through a stereomicroscope (×40 magnification).
Results
Statistically significant differences in accuracy were found comparing the different impression techniques by CMM (p < 0.01). DI performed the best, while TI techniques revealed a greater variability in the results.
Sheffield test revealed a mean gap of 0.022 ± 0.023 mm (the best TI), 0.063 ± 0.059 mm (the worst TI), 0.015 ± 0.011 mm (the best DI), and 0.019 ± 0.015 mm (the worst DI).
Conclusions
Within the limits of this in vitro study, the digital impression showed better accuracy compared to conventional impressioning.
Clinical relevance
The digital impression might offer a viable alternative to traditional impressions for fabrication of full-arch implant-supported prostheses with satisfactory passive fit.
Similar content being viewed by others
Introduction
The passive fit of prosthodontic frameworks is critical to prevent mechanical and biological complications in multiple implant rehabilitation. Misfitting prostheses may negatively affect the long-term success rate of full-arch fixed implant rehabilitations, particularly in immediate-loading procedures [1,2,3,4,5,6,7].
Impression deformations and errors during dental laboratory procedures greatly contribute to generate misfits in implant prosthodontics [2, 6, 8].
Various factors involved in implant impression precision have been investigated in literature (e.g., impression material and technique adopted, splinting of impression copings, implant angulation, and depth). According to a systematic review [9], to date there are no guidelines that strictly recommend a certain technique or material to achieve the best accuracy in case of multi-unit implant impression, owing to conflicting evidences emerging from currently available studies.
Indeed, several authors report greater accuracy when a closed tray technique is performed [10, 11], while others support open tray techniques with splinting of the impression copings [12, 13] or without it [14].
Some studies show no differences between open tray versus closed tray technique [15, 16] as well as splinted versus unsplinted technique [17, 18].
Polyethers (PE) and polyvinylsiloxanes (PVS) are both acknowledged as excellent impression materials for implant rehabilitations [2, 9]. Many authors promote the use of PE for edentulous dental arches [9].
In the last decades, computer-aided design/computer-aided manufacturing (CAD/CAM) technology has been advocated as a reliable tool to produce precise prostheses both on natural teeth and on dental implants [19, 20].
The CAD phase consists of 3D data acquisition, performed by a digitizing unit and followed by software elaboration. Once the prosthodontic restoration has been designed and milling parameters have been set, the following CAM phase is assigned to mill it from blocks made of a definite restoration material [21].
Traditional impressions or casts can be digitized and sent to the dental laboratory by e-mail [6, 19,20,21,22,23,24]. Nowadays, intraoral digitizers have been introduced to directly perform digital impressions of dental arches.
There is a growing interest towards the potential benefits offered by these systems compared to traditional implant impressions.
The digital impression allows simplifying the workflow. Indeed, some operational steps can be skipped with remarkable decrease of time and material costs, such as tray selection and customization, mixing of impression materials, disinfection after impression setting, impression storage, shipping of the impression to the dental laboratory, definitive cast pouring, and articulation [19,20,21,22,23].
Digital data acquisition let clinicians obtain a 3D pre-visualization of the preparation and the implant prosthodontic space [20], improving communication both with the dental team and with patients [25, 26].
Other claimed advantages are higher accuracy [20, 22,23,24,25,26] by minimizing operator-dependent variability and removing material-dependent factors (e.g., dimensional changes of impression and cast materials) and increased patient compliance [20, 27], particularly in those affected by incoercible gag reflex or with difficulty in opening the mouth.
Downsides related to the use of an intraoral digitizer are mainly the high initial economic investment and the need of a learning curve for clinicians, as well as for dental technicians [19].
Intraoral digital impression performance is well-established for single crowns and short bridges both on natural teeth [24, 28] and on dental implants [29].
However, a recent systematic review of the literature reports that there are still few studies concerning digital impression accuracy on multi-unit implants [30].
The primary aim of this in vitro study is to evaluate the accuracy of eight different implant impression techniques and material combinations, comparing conventional versus digital impression.
The second end point is to test the passive fit of four titanium-milled frameworks obtained respectively from the best and the worst impressions performed through traditional and digital techniques.
Materials and methods
Master cast fabrication
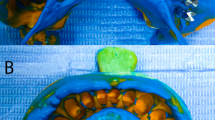
Four implant low-profile analogs (diameter = 4 mm) [low -profile abutment non-hexed temporary cylinder, Biomet 3i, Palm Beach Gardens, FL, USA] were screwed on a prosthetic metal framework (height = 6 mm; width = 3 mm; length = 100 mm) made in Au-Pd alloy (Pallorag 33, Cendres+Métaux, Biel, Switzerland), and a simplified master cast was poured. The four low-profile implant analogs were embedded into the master cast and were placed at the level of the canines (positions 13 and 23) and the first molars (positions 16 and 26) to simulate a full-arch rehabilitation on multiple implants (Fig. 1).
The master cast had a parallelepiped shape with flat surfaces (height = 35 mm; width = 100 mm; length = 160 mm).
Traditional impression techniques
Seven traditional impression (TI) techniques were investigated:
-
- Open tray technique with polyether#1 [Impregum Penta, 3M ESPE, Saint Paul, MN, USA] (OT-1);
-
- Open tray technique with polyether#1 and splinting of impression copings with acrylic resin (OTS-1);
-
- Closed tray technique with polyether#1 (CT-1);
-
- Open tray technique with polyether#2 [Ramitec Penta, 3M ESPE] (OT-2);
-
- Open tray technique with polyether#2 and splinting of impression copings with acrylic resin (OTS-2);
-
- Closed tray technique with polyether#2 (CT-2);
-
- Open tray technique and plaster impression material [BF Plaster, Dental Torino, Torino, Italy] (OT-P).
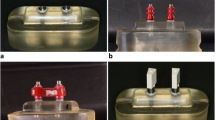
An impression simulator device was used to standardize the impression procedure [7] (Fig. 2). It presented a lower metal platform, where two lateral clamps fixed the master cast in a set position. Four rails connected the lower platform to an upper platform provided with a central pin and ball bearings. During the impression procedure, the upper platform gradually entered into contact with the impression tray in order to uniformly press it over the master cast.
All the TIs were performed using disposable plastic trays for maxillary arch [U3 tray, Dental Trey s.r.l., Predappio, Italy]. Dental wax was applied on each impression tray for posterior palatal seal [Cera Azzurrina Morbidissima, Industria Zingardi srl, Zeta, Novi Ligure, Italy].
When an open tray technique was performed (OT-1, OTS-1, OT-2, OTS-2, OT-P), four access holes on the tray allowed the passage of pick-up impression copings [low-profile abutment non-hexed pick-up impression coping, Biomet 3i].
In case of closed tray techniques (CT-1, CT-2), transfer impression copings [low-profile non-hexed transfer impression coping, Biomet 3i] were used.
Impression adhesive [Polyether Adhesive, 3M ESPE] was applied 15 min before taking the impression with a polyether material.
Polyether materials used in this study were mixed with an automatic mixing unit [Pentamix, 3M ESPE], while a calibrated operator manually mixed the impression plaster, according to the manufacturer’s instructions.
Self-curing acrylic resin [Duralay pattern resin, Reliance Dental Mfg. Co., Worth, IL, USA] supported by a dental floss framework was used to splint the pick-up impression copings 7 min before taking the impression (OTS-1, OTS-2).
Five impressions of the master cast were performed for each traditional technique, thus 35 sample casts (hereafter: TI casts) were poured. All the TI casts presented the same kind of implant low-profile analogs used for the master cast.
Digital impression technique
Each of three expert prosthodontists performed five digital impressions (DI) of the master cast using an intraoral digitizer system [True Definition Scanner, 3M ESPE]. The intraoral digitizer device consists in a 3D video system able to capture up to 20 3D datasets per second [27], through a real-time registration (also known as 3D in motion technique). The three operators had never used an intraoral digitizer before and followed a learning curve of 1 day with the digitizer system. The training session comprised a 4-h explanation of the system and its application and 4 h of practice using the master cast. The clinicians complied with a defined protocol: before taking the scan, four scan bodies (diameter = 4 mm; height = 8 mm) made of polyether ether ketone (PEEK) [Createch Medical, Createch Medical S.L., Mendaro, Spain] were screwed on the master cast implant analogs to digitally detect implant position.
Subsequently, the master cast was powdered with an homogeneous layer of dust [3M High-Resolution Scanning Spray, 3M ESPE] for digitizing procedures.
Each of three operators performed the powdering of the master cast before the start of the first digital impression: the layer of dust had to be removed carefully with an air blast after having accomplished a series of five impressions.
The digitizing procedure started from implant 26 and proceeded in continuous mode around all the scan bodies, reaching implant 16, in order to obtain a first overall scan, as described by Gimenez et al. [20]. Then a further scan of each scan body was accomplished, making circular movements around the scan bodies. The whole digitizing process had to be performed in less than 7 min. At the end of the impression procedure, the operating system confirmed the suitability of the scan or highlighted the need to repeat the scan, in order to acquire missing or incorrectly digitized areas. No casts were fabricated from DI scans.
CMM analysis
A coordinate measurement machine (CMM) [Coordinate Measurement Machine CRYSTA-Apex S, Mitutoyo America Corporation, IL, USA] was used to detect the three-dimensional spatial position of implant analogs in both the master cast and the TI casts, according to the method described by Gimenez et al. [20].
CMM touch spherical probe (diameter = 1 mm) measured the points of each scan body head (Fig. 3: plane 1a) and lateral surfaces to find their respective coordinates on the x-axis, y-axis, and z-axis.
Measurement of inter-implant distances. a The central point 1 (or “control point 1”) of implant 26 is defined as the intersection between the central axis of the implant 26 scan body (“Line 1” in the picture) and the horizontal plane of the head of implant analog 26 (“Plane 1b” in the picture). “Plane 1a” corresponds to the head of the scan body screwed on implant 26. b Control point 1, which refers to implant 26, is joined with the other implant analogs control points, and three inter-implant linear distances (26–23; 26–13; 26–16) are calculated
The master cast data were considered as reference in the present study.
Standard Tessellation Language (STL) files of each DI scan, as well as TI casts data collected by CMM, were compared with the master cast using a CAD reverse engineering software [Rapidform, 3D Systems, Rock Hill, SC, USA].
The software identified the central axis of all the scan bodies (Fig. 3: line 1) as well as the central axis of the four implant analogs (Fig. 3: analog axis) [20]. Since the height of the scan bodies used in the present study is 8 mm, the perpendicular plane at the level of the implant analog head (Fig. 3: Plane 1b) results in a parallel to the top plane (Fig. 3: Plane 1a) at 8 mm offset.
The intersection between the central axis and the perpendicular horizontal plane of each implant analog head allowed to find a “central point” (or “control point”): then, three inter-implant linear distances (26–23; 26–13; 26–16) (Fig. 3) as well as three inter-implant angular values (26–23; 26–13; 26–16) (Fig. 4) were measured.
Measurement of inter-implant angular values. a Superimposition of implant 26 and implant 23 scan body control points. Line 1 and Line 2 are the central axes of scan body 26 and scan body 23, respectively. b The angles between the central axis (Line 1) of implant 26 scan body and the rest of scan body central axes are displayed. Subsequently, three inter-implant angular values (26–23; 26–13; 26–16) are calculated
Two main parameters were highlighted: Distance Error (mm) and Angle Absolute (ABS) Error (°).
Distance Error is the mean value of deviation from the master cast, and it is calculated by subtracting master cast inter-implant distance data to TI cast (or DI scan) distance data.
Angle ABS Error is the mean angular deviation from the master cast, and it is obtained by subtracting the master cast inter-implant angular data to TI cast (or DI scan) angular data.
Framework accuracy
The best and the worst TI casts (as assessed by CMM analysis), as well as the best and the worst DI scans, were selected in order to fabricate four milled-titanium frameworks.
The passive fit of each metal framework was evaluated with the Sheffield test (also known as one-screw test) [31], screwing each framework on the master cast (Fig. 5).
A stereomicroscope [Wild M3Z, Wild Heerbrugg, Heerbrugg, Switzerland], coupled with an eyepiece camera connected to a computer [Dino-Eye AM4023X, Dino-Lite Digital Microscope, AnMo Electronics Corporation, New Taipei City, Taiwan], and the software DinoCapture 2.0 [Dino-Lite Digital Microscope, AnMo Electronics Corporation] were used to detect the maximum gap (mm) between each implant analog and the framework, with a ×40 magnification (Fig. 6).
A total of eight measurements were recorded for each metal framework: four screwing the framework at implant site 26, and another four screwing the framework at implant site 16.
Statistical analysis
Distance Error and Angle ABS Error parameters were statistically analyzed with one-way ANOVA test.
Alpha level was set at 0.05 (CI 95%), and all the statistical analyses were performed using SPSS software v.20 [IBM Corp., Armonk, NY, USA].
Results
CMM analysis results
CMM findings are reported in Table 1.
Statistically significant differences were reported between DI and TI techniques both for Distance Error (p = 0.000) and Angle ABS Error (p = 0.001).
DI reported low values of deviation from the master cast, showing higher reproducibility in the results with respect to TI techniques (Fig. 7 and Fig. 8). TI techniques revealed a greater variability in the results, especially in Distance Error (Fig. 7).
OT-P and OTS-1 performed the best in Angle ABS Error, showing the lowest variation for this parameter.
Framework accuracy results
The best and the worst DI as well as the best TI cast (from OTS-1 group) and the worst TI cast (from CT-1 group) were selected for the fabrication of four titanium bars. Sheffield test results are reported in Table 2.
The worst TI (CT-1) showed the highest mean value of gap (0.063 ± 0.059 mm) at the framework-implant analog interface compared to the other groups. The worst DI showed results similar to the best TI and the best DI.
Discussion
The findings of CMM analysis are in full accordance with those studies reporting that conventional impression deformations are almost inevitable [2, 6, 8] and unpredictable, since they tend to show a casual pattern of display [32]. Indeed, in the present research TI techniques showed great variability in Distance Error parameter, compared to the DI group (Table 1). Digital impression resulted to be more predictable considering both distance and angle errors, with low values of deviation from the master cast. It should also be underlined that such results were obtained by operators who had no experience in the use of the intraoral digitizer before the start of the study. They attended a 1-day training session the day before the start of the study. Gimenez et al. [20] investigated the accuracy of digital impressions performed by untrained operators versus expert clinicians.
According to their results, expert clinicians reported higher accuracy in Distance Error (mean − 0.03 ± 0.025 mm; range − 0.088 to 0.027 mm) compared to untrained operators (mean 0.013 ± 0.051 mm; range − 0.083 to 0.11 mm), with a difference of 44 μm between the two groups.
Our findings are similar to the outcomes reported for the untrained operators group by Gimenez et al. [20].
Indeed, the DI group in the present study showed a mean value of deviation in Distance Error close to 0 (− 0.012 ± 0.026 mm) (Table 1; Fig. 7).
Some authors emphasized that improvement in accuracy with digital impression systems can be achieved by practicing with an increased number of tests [19, 20]. Since experience represents a quite subjective matter, it is not easy to establish how many digital impressions are needed to achieve a satisfactory learning curve before clinical application [20].
Unlike the TI groups comprising different material-technique combinations, always the same impression protocol was used in the DI group. Three different clinicians performed the digital impressions, while TI techniques were made with an impression simulator. Thus, an inter-operator variability was introduced in the DI group. The strict compliance with the impression protocol indicated by the manufacturer of the intraoral digitizer could be one of the reasons for the more reproducible outcomes of the DI group compared to TI groups. Each step of the prosthodontic procedure, from the impression making to the plaster cast fabrication, might have influenced the higher variability of data distribution of the TI techniques compared to the DI group.
Indeed, sources of distortions can be the machining tolerance of the impression copings and implant analogs, the displacement of impression copings due to the shrinkage of the impression material, and the displacement of implant analogs due to the expansion of the plaster cast during the pouring step [1, 20].
The digital acquisition of implant position allows to eliminate several clinical and laboratory phases [19,20,21,22,23], which might introduce distortions [2, 6, 8]. This is significant, because the ability to simplify the prosthodontic workflow, by removing one or more steps, leads to error reduction, with an enhancement of final accuracy as a consequence [29].
As regards conventional impressions, the outcomes of the present study do not establish which impression technique is the most accurate.
To choose the best impression material and technique, clinicians have to take into account the following factors in good balance: reproducibility, ease of application, reduction in time and costs, and patient’s compliance. Impression plaster exhibited optimal outcomes in the present study, showing the lowest angle error among tested materials. The main advantages related to impression plaster material are high degree of stiffness, reduced costs, and setting time compared to polyethers [33]. Impression material stiffness after setting has been acknowledged as a critical property to reliably reproduce implant position. Indeed, implant component displacement during the impression tray removal, as well as during the laboratory steps, negatively affects the accuracy of the prosthodontic rehabilitation [1, 7].
However, the presence of teeth, deep anatomical undercuts, and low patient acceptance limit the use of impression plaster.
Polyethers are widely used in implant prosthodontics thanks to their excellent properties, including higher rigidity compared to polyvinylsiloxanes. The high hydrophilicity of polyethers allows a reliable reproduction of details, even in the presence of blood or saliva, in both partially and totally edentulous patients [1, 2].
For this reason, it may be a viable alternative to plaster impression material.
Conversely to polyether#1, polyether#2 is a bite registration material without defined clinical indications in implant dentistry. However, polyether#2 was tested in this study because its rigidity after setting is higher than polyether#1 [7].
According to Burns et al. [34], the customized tray, thanks to its higher stiffness compared to stock trays, allows to get a more accurate impression and a uniform thickness because of the better distribution of the impression material within the tray.
However, Shen et al. [35] suggested that the use of customized trays is not critical for an improved accuracy if polyethers and PVS are used, because these elastomeric materials already present a satisfactory inherent rigidity and high dimensional stability, both of which represent key factors to reduce the risk of distortions.
Disposable plastic impression trays were chosen for all the traditional impression techniques tested in this study, in order to simulate clinical practice when full-arch impressions are taken in immediate loading rehabilitations. In this case, plastic trays were used because the access holes for the pick-up copings used for the direct impression techniques can be easily made.
Splinting of impression copings with acrylic resin is aimed to prevent movements of the implants during the impression procedure [1, 2].
Autopolymerizing acrylic resins are commonly used as splinting materials [9].
The inevitable polymerization shrinkage of the resins represents a factor of distortion which could negatively affect the accuracy of the implant prosthesis.
Mojon et al. [36] reported a shrinkage rate of 7.9% after 24 h. Moreover, almost 80% of the shrinkage occurs within the first 17 min.
The polymerization shrinkage of the pattern resin is directly proportional to the mass of the splint.
Therefore, the resulting splinting length when long spans are present in full-arch impressions may negatively affect the dimensional stability of the resin used.
Some authors suggested cutting the splint and subsequently joining the cut parts after 24 h by adding further resin, in order to restore the splint and minimize the polymerization shrinkage at the same time [37].
However, this procedure does not represent the ideal solution in case of full-arch immediate-loading implant protocols, mainly because of the lengthening of working time and the need for a second appointment [7]. This is the reason why the splint was not cut and reconnected in OTS-1 and OTS-2 groups.
Our findings are in accordance with the studies supporting that splinting of the copings is not critical for improving the impression accuracy [17, 18].
Kim et al. [17] and Choi et al. [18] tested the direct impression technique with full-arch bridges and partial bridges, respectively, splinting the impression copings with self-curing acrylic resin. The splint was cut and reconnected with incremental application of resin in order to reduce the polymerization shrinkage.
Although it is not possible to achieve absolute passive fit of implant prostheses [1, 2, 9], every effort should be made to minimize misfits at the implant-framework interface.
The Sheffield test is a widespread method to detect clinically implant framework misfits [1, 19]. Nejatidanesh et al. [38] used the Sheffield test, combined with a stereomicroscopy investigation, to measure the gap size at the implant-framework interface in vitro such as in the present research.
The metal framework obtained from the worst TI cast (CT-1) exhibited the worst results in terms of accuracy, while all the other frameworks presented comparable mean values of discrepancy < 23 μm (Table 2). However, since a recent systematic review of literature [1] considered a tolerable misfit around 150 μm, all the tested milled titanium frameworks showed a clinically acceptable mean value of gap at the implant-framework interface (Table 2). The present in vitro study compared the accuracy of various conventional impression techniques versus a digital approach with an intraoral digitizer system. There were some limitations in reproducing clinical conditions, such as oral cavity temperature and moisture and presence of saliva or blood.
However, the use of an impression simulator device and a simplified master cast was aimed to reduce the effect of confounding factors related to operator-dependent variability and dental arch anatomy.
The three-dimensional position of the implants was detected on the master cast using a CMM device.
The CMM presents remarkable advantages, allowing the recording of both three-dimensional and rotational distortions with a standardized and repeatable measurement process. The National Entity of Accreditation certified the accuracy of the CMM device used in this study, with a maximum permissible error for length measurement of 1.9 + 3 L/1000 μm (ISO 10360-02 geometrical product specifications) [20].
However, there are some limitations, for instance, the low scan speed and the reduced accuracy in measuring freeform surfaces (such as fissure lines, interproximal areas in dentate casts) because of the size and shape of the touch spherical probe tip (diameter = 1 mm) [39].
Furthermore, the prior knowledge of the surface shape of the object being tested is required before scanning.
Other methods for the detection of implant position and discrepancies in the x-axis, y-axis, and z-axis such as profile projectors, 3D-optical digitizers, 3D optical scanners, and digital micrometers have been reported [9].
The “zero method,” which was described in a previous publication by Gimenez et al. [20], was applied in the present study to make a comparison between the DI group scans and the STL dataset of the master cast (i.e., the cast of reference) recorded with the CMM.
In detail, the center point of implant analog 26 was considered as the origin, so that both linear distances and angular deviations among the implants were obtained, without the need to make a global data overlap.
Indeed, an alternative method to compare the accuracy between digital impressions and a control dataset is to perform a superimposition of the STL datasets according to a “best-fit algorithm.” The best-fit algorithm allows to overlap two point clouds in the best possible way. However, some authors suggest that this method does not show the real divergences adequately because it makes an average of errors by calculating the arithmetic mean of positive and negative values of deviation, which tends to 0 [20, 40].
Conclusions
Within the limitations of this in vitro study, the use of an intraoral digitizer might represent a viable alternative to traditional impression materials for the fabrication of full-arch implant-supported prostheses provided with a satisfactory passive fit.
Dealing with traditional impressions on multiple implants, the use of impression materials with a high degree of stiffness (such as plaster or rigid polyethers) seems favorable to achieve accuracy.
Splinting of pick-up impression copings with acrylic resin is not useful to improve precision in full-arch cases.
Further in vivo studies are required to confirm digital impression accuracy in a clinical setting.
References
Buzayan MM, Yunus NB (2014) Passive fit in screw retained multi-unit implant prosthesis understanding and achieving: a review of the literature. J Indian Prosthodont Soc 14:16–23
Lee H, So JS, Hochstedler JL, Ercoli C (2008) The accuracy of implant impressions: a systematic review. J Prosthet Dent 100:285–291
Shadid R, Sadaqa N (2012) A comparison between screw- and cement-retained implant prostheses. A literature review. J Oral Implantol 38:298–307
Pera P, Menini M, Bevilacqua M, Pesce P, Pera F, Signori A, Tealdo T (2014) Factors affecting the outcome in the immediate loading rehabilitation of the maxilla: a 6-year prospective study. Int J Periodontics Restorative Dent 34:657–665
Menini M, Dellepiane E, Pera P, Bevilacqua M, Pesce P, Pera F, Tealdo T (2016) A luting technique for passive fit of implant-supported fixed dentures. J Prosthodont 25:77–82
Stimmelmayr M, Güth JF, Erdelt K, Edelhoff D, Beuer F (2012) Digital evaluation of the reproducibility of implant scanbodyfit—an in vitro study. Clin Oral Investig 16:851–856
Pera F, Pesce P, Bevilacqua M, Setti P, Menini M (2016) Analysis of different impression techniques and materials on multiple implants through 3-dimensional laser scanner. Implant Dent 25:232–237
Heckmann SM, Karl M, Wichmann MG, Winter W, Graef F, Taylor TD (2004) Cement fixation and screw retention: parameters of passive fit. An in vitro study of three-unit implant-supported fixed partial dentures. Clin Oral Implants Res 15:466–473
Baig MR (2014) Accuracy of impressions of multiple implants in the edentulous arch: a systematic review. Int J Oral Maxillofac Implants 29:869–880
Humphries RM, Yaman P, Bloem TJ (1990) The accuracy of implant master casts constructed from transfer impressions. Int J Oral Maxillofac Implants 5:331–336
De La Cruz JE, Funkenbusch PD, Ercoli C, Moss ME, Graser GN, Tallents RH (2002) Verification jig for implant-supported prostheses: a comparison of standard impressions with verification jigs made of different materials. J Prosthet Dent 88:329–336
Naconecy MM, Teixeira ER, Shinkai RS, Frasca LC, Cervieri A (2004) Evaluation of the accuracy of 3 transfer techniques for implant-supported prostheses with multiple abutments. Int J Oral Maxillofac Implants 19:192–198
Vigolo P, Majzoub Z, Cordioli G (2003) Evaluation of the accuracy of three techniques used for multiple implant abutment impressions. J Prosthet Dent 89:186–192
Burawi G, Houston F, Byrne D, Claffey N (1997) A comparison of the dimensional accuracy of the splinted and unsplinted impression techniques for the Bone-Lockimplant system. J Prosthet Dent 77:68–75
Chang WG, Vahidi F, Bae KH, Lim S (2012) Accuracy of three implant impression techniques with different impression materials and stones. Int J Prosthodont 25:44–47
Conrad HJ, Pesun IJ, DeLong R, Hodges JS (2007) Accuracy of two impression techniques with angulated implants. J Prosthet Dent 97:349–356
Kim S, Nicholls JI, Han CH, Lee KW (2006) Displacement of implant components from impressions to definitive casts. Int J Oral Maxillofac Implants 21:747–755
Choi JH, Lim YJ, Yim SH, Kim CW (2007) Evaluation of the accuracy of implant-level impression techniques for internal-connection implant prostheses in parallel and divergent models. Int J Oral Maxillofac Implants 22:761–768
Lin WS, Harris BT, Zandinejad A, Morton D (2014) Use of digital data acquisition and CAD/CAM technology for the fabrication of a fixed complete dental prosthesis on dental implants. J Prosthet Dent 111:1–5
Giménez B, Özcan M, Martínez-Rus F, Pradíes G (2015) Accuracy of a digital impression system based on active wavefront sampling technology for implants considering operator experience, implant angulation, and depth. Clin Implant Dent Relat Res 17:54–64
Seelbach P, Brueckel C, Wöstmann B (2012) Accuracy of digital and conventional impression techniques and workflow. Clin Oral Investig 17:1759–1764
Patzelt SB, Bishti S, Stampf S, Att W (2014) Accuracy of full-arch scans using intraoral scanners. Clin Oral Investig 18:1687–1694
Ting-Shu S, Jian S (2015) Intraoral digital impression technique: a review. J Prosthodont 24:313–321
Keul C, Stawarczyk B, Erdelt KJ, Beuer F, Edelhoff D, Güth JF (2014) Fit of 4-unit FDPs made of zirconia and CoCr-alloy after chairside and labside digitalization-a laboratory study. Dent Mater 30:400–407
Lee SJ, Gallucci GO (2013) Digital vs. conventional implant impressions: efficiency outcomes. Clin Oral Implants Res 24:111–115
Flügge TV, Schlager S, Nelson K, Nahles S, Metzger MC (2013) Precision of intraoral digital dental impressions with iTero and extraoral digitization with the iTero and a model scanner. Am J Orthod Dentofac Orthop 144:471–478
Wismeijer D, Mans R, van Genuchten M, Reijers HA (2014) Patients’ preferences when comparing analogue implant impressions using a polyether impression material versus digital impressions (Intraoral Scan) of dental implants. Clin Oral Implants Res 25:1113–1118
Syrek A, Reich G, Ranftl D, Klein C, Cerny B, Brodesser J (2010) Clinical evaluation of all-ceramic crowns fabricated from intraoral digital impressions based on the principle of active wavefront sampling. J Dent 38:553–559
Joda T, Katsoulis J, Brägger U (2015) Clinical fitting and adjustment time for implant-supported crowns comparing digital and conventional workflows. Clin Implant Dent Relat Res. https://doi.org/10.1111/cid.12377
Baig MR (2014) Multi-unit implant impression accuracy: a review of the literature. Quintessence Int 45:39–51
Kan JY, Rungcharassaeng K, Bohsali K, Goodacre CJ, Lang BR (1999) Clinical methods for evaluating implant framework fit. J Prosthet Dent 81:7–13
Hoods-Moonsammy VJ, Owen P, Howes DG (2014) A comparison of the accuracy of polyether, polyvinyl siloxane, and plaster impressions for long-span implant-supported prostheses. Int J Prosthodont 27:433–438
Assif D, Nissan J, Varsano I, Singer A (1999) Accuracy of implant impression splinted techniques: effect of splinting material. Int J Oral Maxillofac Implants 14:885–888
Burns J, Palmer R, Howe L, Wilson R (2003) Accuracy of open tray implant impressions: an in vitro comparison of stock versus custom trays. J Prosthet Dent 89:250–255
Shen C (2003) Impression materials. In: Anusavice KJ (ed) Phillips’ Science of Dental Materials, 11th edn. Saunders, Philadelphia, pp 205–254
Mojon P, Oberholzer JP, Meyer JM, Belser UC (1990) Polymerization shrinkage of index and pattern acrylic resins. J Prosthet Dent 64:684–688
Gibbs SB, Versluis A, Tantbirojn D, Ahuja S (2014) Comparison of polymerization shrinkage of pattern resins. J Prosthet Dent 112:293–298
Nejatidanesh F, Shakibamehr AH, Savabi O (2016) Comparison of marginal and internal adaptation of CAD/CAM and conventional cement retained implant-supported single crowns. Implant Dent 25:103–108
Ender A, Mehl A (2013) Accuracy of complete-arch dental impressions: a new method of measuring trueness and precision. J Prosthet Dent 109:121–128
Güth JF, Keul C, Stimmelmayr M, Beuer F, Edelhoff D (2013) Accuracy of digital models obtained by direct and indirect data capturing. Clin Oral Investig 17:1201–1208
Acknowledgements
The authors thank 3M ESPE for providing materials.
Furthermore, the authors wish to thank Prof. Fabrizio Barberis and Dr. Alberto Lagazzo (Department of Civil, Chemical and Environmental Engineering, University of Genova) for their assistance in data analysis.
Funding
The work was supported by the Department of Surgical and Diagnostic Sciences (DISC), Division of Prosthodontics, University of Genova, Genova, Italy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Menini, M., Setti, P., Pera, F. et al. Accuracy of multi-unit implant impression: traditional techniques versus a digital procedure. Clin Oral Invest 22, 1253–1262 (2018). https://doi.org/10.1007/s00784-017-2217-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-017-2217-9