Abstract
Objectives
The clinical standard for alveolar cleft osteoplasty is augmentation with autologous bone being available in limited amounts and might be associated with donor site morbidity. The aim of the present study was the creation of tissue-engineered bone grafts and their in vivo evaluation regarding their potential to promote osteogenesis in an alveolar cleft model.
Materials and methods
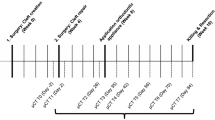
Artificial bone defects with a diameter of 3.3 mm were created surgically in the palate of 84 adult Lewis rats. Four experimental groups (n = 21) were examined: bovine hydroxyl apatite/collagen (bHA) without cells, bHA with undifferentiated mesenchymal stromal cells (MSC), bHA with osteogenically differentiated MSC. In a control group, the defect remained empty. After 6, 9 and 12 weeks, the remaining defect volume was assessed by cone beam computed tomography. Histologically, the remaining defect width and percentage of bone formation was quantified.
Results
After 12 weeks, the remaining defect width was 60.1% for bHA, 74.7% for bHA with undifferentiated MSC and 81.8% for bHA with osteogenically differentiated MSC. For the control group, the remaining defect width measured 46.2% which was a statistically significant difference (p < 0.001).
Conclusions
The study design was suitable to evaluate tissue-engineered bone grafts prior to a clinical application. In this experimental set-up with the described maxillary defect, no promoting influence on bone formation of bone grafts containing bHA could be confirmed.
Clinical relevance
The creation of a sufficient tissue-engineered bone graft for alveolar cleft osteoplasty could preserve patients from donor site morbidity.





Similar content being viewed by others
References
Dixon MJ, Marazita ML, Beaty TH et al (2011) Cleft lip and palate: understanding genetic and environmental influences. Nat Rev Genet 12(3):167–178. doi:10.1038/nrg2933
Witsenburg B (1985) The reconstruction of anterior residual bone defects in patients with cleft lip, alveolus and palate. A review. J Maxillofac Surg 13(5):197–208
Horswell BB, Henderson JM (2003) Secondary osteoplasty of the alveolar cleft defect. J Oral Maxillofac Surg 61(9):1082–1090
Younger EM, Chapman MW (1989) Morbidity at bone graft donor sites. J Orthop Trauma 3(3):192–195
Moreau JL, Caccamese JF, Coletti DP et al (2007) Tissue engineering solutions for cleft palates. J Oral Maxillofac Surg 65(12):2503–2511. doi:10.1016/j.joms.2007.06.648
Nguyen PD, Lin CD, Allori AC et al (2009) Establishment of a critical-sized alveolar defect in the rat: a model for human gingivoperiosteoplasty. Plast Reconstr Surg 123(3):817–825. doi:10.1097/PRS.0b013e31819ba2f4
Draenert FG, Huetzen D, Neff A et al (2014) Vertical bone augmentation procedures: basics and techniques in dental implantology. J Biomed Mater Res A 102(5):1605–1613. doi:10.1002/jbm.a.34812
Herford AS, Nguyen K (2015) Complex bone augmentation in alveolar ridge defects. Oral Maxillofac Surg Clin North Am 27(2):227–244. doi:10.1016/j.coms.2015.01.003
Feinberg SE, Weisbrode SE, Heintschel G (1989) Radiographic and histological analysis of tooth eruption through calcium phosphate ceramics in the cat. Arch Oral Biol 34(12):975–984
Salgado AJ, Coutinho OP, Reis RL (2004) Bone tissue engineering: state of the art and future trends. Macromol Biosci 4(8):743–765. doi:10.1002/mabi.200400026
Fisher JN, Peretti GM, Scotti C (2016) Stem cells for bone regeneration: from cell-based therapies to decellularised engineered extracellular matrices. Stem Cells Int 2016:9352598. doi:10.1155/2016/9352598
Yousefi A, James PF, Akbarzadeh R et al (2016) Prospect of stem cells in bone tissue engineering: a review. Stem Cells Int 2016:6180487. doi:10.1155/2016/6180487
Logeart-Avramoglou D, Anagnostou F, Bizios R et al (2005) Engineering bone: challenges and obstacles. J Cell Mol Med 9(1):72–84
Gladysz D, Hozyasz KK (2015) Stem cell regenerative therapy in alveolar cleft reconstruction. Arch Oral Biol 60(10):1517–1532. doi:10.1016/j.archoralbio.2015.07.003
Mastrangelo F, Quaresima R, Grilli A et al (2013) A comparison of bovine bone and hydroxyapatite scaffolds during initial bone regeneration: an in vitro evaluation. Implant Dent 22(6):613–622. doi:10.1097/ID.0b013e3182a69858
Santos PL, Gulinelli JL, Telles CS et al (2013) Bone substitutes for peri-implant defects of postextraction implants. Int J Biomater 2013:307136. doi:10.1155/2013/307136
Oliveira R, El HM, Carrel JP et al (2012) Rehabilitation of the edentulous posterior maxilla after sinus floor elevation using deproteinized bovine bone: a 9-year clinical study. Implant Dent 21(5):422–426. doi:10.1097/ID.0b013e3182691873
Kato E, Lemler J, Sakurai K et al (2014) Biodegradation property of beta-tricalcium phosphate-collagen composite in accordance with bone formation: a comparative study with Bio-Oss Collagen(R) in a rat critical-size defect model. Clin Implant Dent Relat Res 16(2):202–211. doi:10.1111/j.1708-8208.2012.00467.x
Lammers L, Naujoks C, Berr K et al (2012) Impact of DAG stimulation on mineral synthesis, mineral structure and osteogenic differentiation of human cord blood stem cells. Stem Cell Res 8(2):193–205. doi:10.1016/j.scr.2011.09.004
Kunert-Keil C, Scholz F, Gedrange T et al (2015) Comparative study of biphasic calcium phosphate with beta-tricalcium phosphate in rat cranial defects—a molecular-biological and histological study. Ann Anat 199:79–84. doi:10.1016/j.aanat.2013.12.001
Korn P, Schulz MC, Range U et al (2014) Efficacy of tissue engineered bone grafts containing mesenchymal stromal cells for cleft alveolar osteoplasty in a rat model. J Craniomaxillofac Surg 42(7):1277–1285. doi:10.1016/j.jcms.2014.03.010
Donath K, Breuner G (1982) A method for the study of undecalcified bones and teeth with attached soft tissues. The Sage-Schliff (sawing and grinding) technique. J Oral Pathol 11(4):318–326
Pradel W, Lauer G (2012) Tissue-engineered bone grafts for osteoplasty in patients with cleft alveolus. Ann Anat 194(6):545–548. doi:10.1016/j.aanat.2012.06.002
Mehrara BJ, Saadeh PB, Steinbrech DS et al (2000) A rat model of gingivoperiosteoplasty. J Craniofac Surg 11(1):54–58
Mostafa NZ, Doschak MR, Major PW et al (2014) Reliable critical sized defect rodent model for cleft palate research. J Craniomaxillofac Surg 42(8):1840–1846. doi:10.1016/j.jcms.2014.07.001
Pourebrahim N, Hashemibeni B, Shahnaseri S et al (2013) A comparison of tissue-engineered bone from adipose-derived stem cell with autogenous bone repair in maxillary alveolar cleft model in dogs. Int J Oral Maxillofac Surg 42(5):562–568. doi:10.1016/j.ijom.2012.10.012
Zhang J, Yang R, Liu Z et al (2015) Loss of lysyl oxidase-like 3 causes cleft palate and spinal deformity in mice. Hum Mol Genet 24(21):6174–6185. doi:10.1093/hmg/ddv333
Yamada M, Yamamoto N, Ohgami S et al (2014) The effect of sevoflurane on developing A/J strain mouse embryos using a whole-embryo culture system—the incidence of cleft lip in culture embryos. Vitro Cell Dev Biol Anim 50(3):237–242. doi:10.1007/s11626-013-9697-y
Harris CT, Cooper LF (2004) Comparison of bone graft matrices for human mesenchymal stem cell-directed osteogenesis. J Biomed Mater Res A 68(4):747–755. doi:10.1002/jbm.a.20107
Lohberger B, Payer M, Rinner B et al (2012) Human intraoral harvested mesenchymal stem cells: characterization, multilineage differentiation analysis, and 3-dimensional migration of natural bone mineral and tricalcium phosphate scaffolds. J Oral Maxillofac Surg 70(10):2309–2315. doi:10.1016/j.joms.2011.06.216
Liu Q, Douglas T, Zamponi C et al (2011) Comparison of in vitro biocompatibility of NanoBone((R)) and BioOss((R)) for human osteoblasts. Clin Oral Implants Res 22(11):1259–1264. doi:10.1111/j.1600-0501.2010.02100.x
Carmagnola D, Adriaens P, Berglundh T (2003) Healing of human extraction sockets filled with Bio-Oss. Clin Oral Implants Res 14(2):137–143
Esposito M, Grusovin MG, Coulthard P et al (2006) The efficacy of various bone augmentation procedures for dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants 21(5):696–710
Mangano C, Scarano A, Perrotti V et al (2007) Maxillary sinus augmentation with a porous synthetic hydroxyapatite and bovine-derived hydroxyapatite: a comparative clinical and histologic study. Int J Oral Maxillofac Implants 22(6):980–986
Pittenger MF, Mackay AM, Beck SC et al (1999) Multilineage potential of adult human mesenchymal stem cells. Science 284(5411):143–147
Lieberman JR, Daluiski A, Einhorn TA (2002) The role of growth factors in the repair of bone. Biology and clinical applications. J Bone Joint Surg Am 84-A(6):1032–1044
Komori T (2003) Requisite roles of Runx2 and Cbfb in skeletal development. J Bone Miner Metab 21(4):193–197. doi:10.1007/s00774-002-0408-0
Pratap J, Galindo M, Zaidi SK et al (2003) Cell growth regulatory role of Runx2 during proliferative expansion of preosteoblasts. Cancer Res 63(17):5357–5362
Jonason JH, Xiao G, Zhang M et al (2009) Post-translational regulation of Runx2 in bone and cartilage. J Dent Res 88(8):693–703. doi:10.1177/0022034509341629
Jensen ED, Gopalakrishnan R, Westendorf JJ (2010) Regulation of gene expression in osteoblasts. Biofactors 36(1):25–32. doi:10.1002/biof.72
Ducy P (2000) Cbfa1: a molecular switch in osteoblast biology. Dev Dyn 219(4):461–471. doi:10.1002/1097-0177(2000)9999:9999<:AID-DVDY1074>3.0.CO;2-C
Komori T, Yagi H, Nomura S et al (1997) Targeted disruption of Cbfa1 results in a complete lack of bone formation owing to maturational arrest of osteoblasts. Cell 89(5):755–764
Mostafa NZ, Talwar R, Shahin M et al (2015) Cleft palate reconstruction using collagen and nanofiber scaffold incorporating bone morphogenetic protein in rats. Tissue Eng Part A 21(1–2):85–95. doi:10.1089/ten.tea.2014.0075
Mayer M, Hollinger J, Ron E et al (1996) Maxillary alveolar cleft repair in dogs using recombinant human bone morphogenetic protein-2 and a polymer carrier. Plast Reconstr Surg 98(2):247–259
Nguyen PD, Lin CD, Allori AC et al (2009) Scaffold-based rhBMP-2 therapy in a rat alveolar defect model: implications for human gingivoperiosteoplasty. Plast Reconstr Surg 124(6):1829–1839. doi:10.1097/PRS.0b013e3181bf8024
Araujo M, Linder E, Lindhe J (2009) Effect of a xenograft on early bone formation in extraction sockets: an experimental study in dog. Clin Oral Implants Res 20(1):1–6. doi:10.1111/j.1600-0501.2008.01606.x
van Hout WMMT, van der Molen M, Aebele B, Breugem CC et al (2011) Reconstruction of the alveolar cleft: can growth factor-aided tissue engineering replace autologous bone grafting? A literature review and systematic review of results obtained with bone morphogenetic protein-2. Clin Oral Investig 15(3):297–303. doi:10.1007/s00784-011-0547-6
Herford AS, Boyne PJ, Rawson R et al (2007) Bone morphogenetic protein-induced repair of the premaxillary cleft. J Oral Maxillofac Surg 65(11):2136–2141. doi:10.1016/j.joms.2007.06.670
Dickinson BP, Ashley RK, Wasson KL et al (2008) Reduced morbidity and improved healing with bone morphogenic protein-2 in older patients with alveolar cleft defects. Plast Reconstr Surg 121(1):209–217. doi:10.1097/01.prs.0000293870.64781.12
Alonso N, Tanikawa DY, Freitas RS et al (2010) Evaluation of maxillary alveolar reconstruction using a resorbable collagen sponge with recombinant human bone morphogenetic protein-2 in cleft lip and palate patients. Tissue Eng Part C Methods 16(5):1183–1189. doi:10.1089/ten.TEC.2009.0824
Benlidayi ME, Tatli U, Kurkcu M et al (2012) Comparison of bovine-derived hydroxyapatite and autogenous bone for secondary alveolar bone grafting in patients with alveolar clefts. J Oral Maxillofac Surg 70(1):e95–e102. doi:10.1016/j.joms.2011.08.041
Behnia H, Khojasteh A, Kiani MT et al (2013) Bone regeneration with a combination of nanocrystalline hydroxyapatite silica gel, platelet-rich growth factor, and mesenchymal stem cells: a histologic study in rabbit calvaria. Oral Surg Oral Med Oral Pathol Oral Radiol 115(2):e7–15. doi:10.1016/j.oooo.2011.09.034
Berger M, Probst F, Schwartz C et al (2015) A concept for scaffold-based tissue engineering in alveolar cleft osteoplasty. J Craniomaxillofac Surg 43(6):830–836. doi:10.1016/j.jcms.2015.04.023
Acknowledgements
The authors want to thank Mrs. Diana Jünger for her extensive assistance in preparing the bone grafts. Furthermore, the authors are grateful to Dr. Roland Jung and the team of the Experimental Centre of the Medical Faculty “Carl Gustav Carus”, Technische Universität Dresden, for the care of the animals and assistance during the surgical interventions. Dr. Heike Meißner is acknowledged for the scanning electron microscope images. Moreover, the authors thank Mr. Torsten Jannasch for the assistance in preparing the images.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The study was financially supported by an internal research grant “MeDDrive Projekt Start” of the Faculty of Medicine “Carl Gustav Carus”, Technische Universität Dresden, Germany. The bone substitute was kindly provided by Geistlich Biomaterials, Wolhusen, Switzerland.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors. All applicable international, national and/or institutional guidelines for the care and use of animals were followed.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Korn, P., Hauptstock, M., Range, U. et al. Application of tissue-engineered bone grafts for alveolar cleft osteoplasty in a rodent model. Clin Oral Invest 21, 2521–2534 (2017). https://doi.org/10.1007/s00784-017-2050-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-017-2050-1