Abstract
Objective
This study aimed to evaluate the effects of a porcine acellular dermal matrix (PADM) with or without an enamel matrix derivative (EMD) on gingival recession defects treated with a coronally advanced flap (CAF) in dogs.
Materials and methods
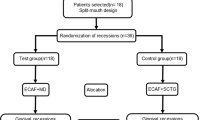
Miller class II gingival recession defects (5 mm wide and 7 mm deep) were surgically created on the labial side of bilateral maxillary canines in 12 dogs. After 8 weeks of plaque accumulation, the 24 chronic defects were randomly assigned to one of the following 4 treatments: CAF, CAF with PADM (CAF/PADM), CAF with EMD (CAF/EMD), and CAF with EMD and PADM (CAF/EMD/PADM). The animals were sacrificed 10 weeks after surgery for histologic evaluation.
Results
In all groups, root coverage was obtained to a varying degree. PADM was well incorporated in gingival connective tissue in the CAF/PADM and in the CAF/EMD/PADM groups. The height of newly formed bone was significantly greater in the CAF/EMD/PADM group than in the CAF and CAF/PADM groups. New cementum with periodontal ligament-like tissue was predominantly found in the CAF/EMD and CAF/EMD/PADM groups. The CAF/EMD/PADM group showed the greatest amount of new cementum among the groups examined, although the difference was not statistically significant.
Conclusion
Within the limitations of the present study, it can be concluded that CAF/EMD/PADM treatment may promote periodontal regeneration in gingival recession defects.
Clinical relevance
The present results suggest that the combination of EMD and PADM in conjunction with CAF may represent a promising approach for treating single Miller class II gingival recessions.






Similar content being viewed by others
References
Löe H, Anerud A, Boysen H (1992) The natural history of periodontal disease in man: prevalence, severity, and extent of gingival recession. J Periodontol 63:489–495
Cheng GL, Fu E, Tu YK, Shen EC, Chiu HC, Huang RY, Yuh DY, Chiang CY (2014) Root coverage by coronally advanced flap with connective tissue graft and/or enamel matrix derivative: a meta-analysis. J Periodontal Res. doi:10.1111/jre12199
Hofmänner P, Alessandri R, Laugisch O, Aroca S, Salvi GE, Stavropoulos A, Sculean A (2012) Predictability of surgical techniques used for coverage of multiple adjacent gingival recessions—a systematic review. Quintessence Int 43:545–554
Griffin TJ, Cheung WS, Zavras AI, Damoulis PD (2006) Postoperative complications following gingival augmentation procedures. J Periodontol 77:2070–2079
Aroca S, Molnár B, Windisch P, Gera I, Salvi GE, Nikolidakis D, Sculean A (2013) Treatment of multiple adjacent Miller class I and II gingival recessions with a modified coronally advanced tunnel (MCAT) technique and a collagen matrix or palatal connective tissue graft: a randomized, controlled clinical trial. J Clin Periodontol 40:713–720
Harris RJ (1998) Root coverage with a connective tissue with partial thickness double pedicle graft and an acellular dermal matrix graft: a clinical and histological evaluation of a case report. J Periodontol 69:1305–1311
Gapski R, Parks CA, Wang HL (2005) Acellular dermal matrix for mucogingival surgery: a meta-analysis. J Periodontol 76:1814–1822
Nuñez J, Caffesse R, Vignoletti F, Guerra F, San Roman F, Sanz M (2009) Clinical and histological evaluation of an acellular dermal matrix allograft in combination with the coronally advanced flap in the treatment of Miller class I recession defects: an experimental study in the mini-pig. J Clin Periodontol 36:523–531
Moslemi N, Mousavi Jazi M, Haghighati F, Morovati SP, Jamali R (2011) Acellular dermal matrix allograft versus subepithelial connective tissue graft in treatment of gingival recessions: a 5-year randomized clinical study. J Clin Periodontol 38:1122–1129
Henderson RD, Greenwell H, Drisko C, Regennitter FJ, Lamb JW, Mehlbauer MJ, Goldsmith LJ, Rebitski G (2001) Predictable multiple site root coverage using an acellular dermal matrix allograft. J Periodontol 76:1814–1822
Cummings LC, Kaldahl WB, Allen EP (2005) Histologic evaluation of autogenous connective tissue and acellular dermal matrix grafts in humans. J Periodontol 76:178–186
Carney CM, Rossmann JA, Kerns DG, Cipher DJ, Ress TD, Soloman ES, Rivera-Hidalgo F, Beach MM (2012) A comparative study of root defect coverage using an acellular dermal matrix with and without a recombinant human platelet-derived growth factor. J Periodontol 83:893–901
Pabst AM, Happe A, Callaway A, Ziebart T, Stratul SI, Ackermann M, Konerding MA, Willershausen B, Kasaj A (2014) In vitro and in vivo characterization of porcine acellular dermal matrix for gingival augmentation procedures. J Periodontal Res 49:371–381
McGuire MK, Scheyer ET (2010) Xenogeneic collagen matrix with coronally advanced flap compared to connective tissue with coronally advanced flap for the treatment of dehiscence-type recession defects. J Periodontol 81:1108–1117
Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L (2012) Treatment of gingival recession defects using coronally advanced flap with a porcine collagen matrix compared to coronally advanced flap with connective tissue graft: a randomized controlled clinical trial. J Periodontol 83:321–328
Jepsen K, Jepsen S, Zucchelli G, Stefanini M, de Sanctis M, Baldini N, Greven B, Heinz B, Wennström J, Cassel B, Vignoletti F, Sanz M (2013) Treatment of gingival recession defects with a coronally advanced flap and a xenogeneic collagen matrix: a multicenter randomized clinical trial. J Clin Periodontol 40:82–89
Molnar B, Aroca S, Keglevich T, Gera I, Windisch P, Stavropoulos A, Sculean A (2013) Treatment of multiple adjacent Miller class I and II gingival recessions with collagen matrix and the modified coronally advanced tunnel technique. Quintessence Int 44:17–24
Sculean A, Mihatovic I, Shirakata Y, Bosshardt DD, Schwarz F, Iglhaut G (2015) Healing of localized gingival recessions treated with coronally advanced flap alone or combined with either a resorbable collagen matrix or subepithelial connective tissue graft. A preclinical study. Clin Oral Investig 19:903–909
Fickl S, Nannmark U, Schlagenhauf U, Hürzeler MB, Kebschull M (2014) Porcine dermal matrix in the treatment of dehiscence-type defects—an experimental split-mouth animal trial. Clin Oral Implants Res. doi:10.1111/clr12355
Pabst AM, Lehmann KM, Walter C, Krüger M, Stratul SI, Kasaj A (2014) Influence of porcine-derived collagen matrix on endothelial progenitor cells: an in vitro study. Odontology Dec 9
Rothamel D, Benner M, Fienitz T, Happe A, Kreppel M, Nickenig HJ, Zöller JE (2014) Biodegradation pattern and tissue integration of native and cross-linked porcine collagen soft tissue augmentation matrices—an experimental study in the rat. Head Face Med. doi:10.1186/1746-160X-10-10
Hammarström L, HeijlL L, Gestrelius S (1997) Periodontal regeneration in a buccal dehiscence model in monkeys after application of enamel matrix proteins. J Clin Periodontol 24:669–677
HeijlL L, Heden G, Svardström G, Östgren A (1997) Enamel matrix derivative (Emdogain®) in the treatment of intrabony periodontal defects. J Clin Periodontol 24:705–714
Al-Hezaimi K, Al-Fahad H, O’Neill R, Shuman L, Griffin T (2012) The effect of enamel matrix protein on gingival tissue thickness in vivo. Odontology 100:61–66
Mellonig JT (1999) Enamel matrix derivative for periodontal reconstructive surgery: technique and clinical and histologic case report. Int J Periodontics Restorative Dent 19:8–19
Araũjo MG, Lindhe J (1998) GTR treatment of degree III furcation defects following application of enamel matrix proteins. J Clin Periodontol 25:524–530
Shirakata Y, Taniyama K, Yoshimoto T, Miyamoto M, Takeuchi N, Matsuyama T, Noguchi K (2010) Regenerative effect of basic fibroblast growth factor on periodontal healing in two-wall intrabony defects in dogs. J Clin Periodontol 37:374–381
Hoang AM, Klebe RG, Steffensen B, Ryu OH, Simmer JP, Cochran DL (2002) Amelogenin is a cell adhesion protein. J Dent Res 81:497–500
Schlueter SR, Carnes DL, Cochran DL (2007) In vitro effects of enamel matrix derivative on microvascular cells. J Periodontol 78:141–151
Miron RJ, Dard M, Weinreb M (2014) Enamel matrix derivative, inflammation and soft tissue wound healing. J Periodontal Res. doi:10.1111/jre12245
Lee EJ, Meraw SJ, Oh TJ, Giannobile WV, Wang HL (2002) Comparative histologic analysis of coronally advanced flap with and without collagen membrane for root coverage. J Periodontol 73:779–788
Sallum EA, Casati MZ, Caffesse RG, Funis LP, Nociti Júnior FH, Sallum AW (2003) Coronally positioned flap with or without enamel matrix protein derivative for the treatment of gingival recessions. Am J Dent 16:287–291
de Oliveira CA, Spolidório LC, Cirelli JA, Marcantonio RA (2005) Acellular dermal matrix allograft used alone and in combination with enamel matrix protein in gingival recession: histologic study in dogs. Int J Periodontics Restorative Dent 25:595–603
Suaid FF, Carvalho MD, Santamaria MP, Casati MZ, Nociti Jr FH, SallumAW SEA (2008) Platelet-rich plasma and connective tissue grafts in the treatment of gingival recessions: a histometric study in dogs. J Periodontol 79:888–895
Al-Hezaimi K, Rudek I, Al-Hamdan KS, Javed F, Iezzi G, Piattelli A, Wang HL (2013) Efficacy of acellular dermal matrix and coronally advanced flaps for the treatment of induced gingival recession defects: a histomorphometric study in dogs. J Periodontol 84:1172–1179
Windisch P, Sculean A, Klein F, Tóth V, Gera I, Reich E, Eickholz P (2002) Comparison of clinical, radiographic, and histometric measurements following treatment with guided tissue regeneration or enamel matrix proteins in human periodontal defects. J Periodontol 73:409–417
Fujita T, Yamamoto S, Ota M, Shibukawa Y, Yamada S (2011) Coverage of gingival recession defects using guided tissue regeneration with and without adjunctive enamel matrix derivative in a dog model. Int J Periodontics Restorative Dent 31:247–253
Haney JM, Nilveus RE, McMillan PJ, Wikesjö UME (1993) Periodontal repair in dogs: expanded polytetrafluoroethylene barrier membranes support wound stabilization and enhance bone regeneration. J Periodontol 64:883–890
Wikesjö UM, Sigurdsson TJ, Lee MB, Tatakis DN, Selvig KA (1995) Dynamics of wound healing in periodontal regenerative therapy. J Calif Dent Assoc 23:30–35
Fickl S, Kebschull M, Schupbach P, Zuhr O, Schlagenhauf U, Hürzeler MB (2011) Bone loss after full-thickness and partial-thickness flap elevation. J Clin Periodontol 38:157–162
Miron RJ, Bosshardt DD, Hedbom E, Zhang Y, Haenni B, Buser D, Sculean A (2012) Adsorption of enamel matrix proteins to a bovine-derived bone grafting material and its regulation of cell adhesion, proliferation, and differentiation. J Periodontol 83:936–947
Ziegler J, Mayr-Wohlfart U, Kessler S, Breitig D, Günther KP (2002) Adsorption and release properties of growth factors from biodegradable implants. J Biomed Mater Res 59:422–428
Woo KM, Chen VJ, Ma PX (2003) Nano-fibrous scaffolding architecture selectively enhances protein adsorption contributing to cell attachment. J Biomed Mater Res A 67A:531–537
Postlethwaite AE, Seyer JM, Kang AH (1978) Chemotactic attraction of human fibroblasts to type I, II, and III collagens and collagen-derived peptides. Proc Natl Acad Sci U S A 75:871–875
Zeldich E, Korean R, Nemcovsky C, Weinreb M (2007) Enamel matrix derivative stimulates human gingival fibroblast proliferation via ERK. J Dent Res 86:41–46
Keila S, Nemcovsky CE, Moses O, Artzi Z, Weinreb M (2004) In vitro effects of enamel matrix proteins on rat bone marrow cells and gingival fibroblasts. J Dent Res 83:134–138
Zeldich E, Korean R, Dard M, Nemcovsky C, Weinreb M (2007) Enamel matrix derivative protects human gingival fibroblasts from TNF-induced apoptosis by inhibiting caspase activation. J Cell Physiol 213:750–758
Haase HR, Bartold PM (2001) Enamel matrix derivative induces matrix synthesis by cultured human periodontal fibroblast cells. J Periodontol 72:341–348
Faler BJ, Macsata RA, Plummer D, Mishra L, Sidawy AN (2006) Transforming growth factor-beta and wound healing. Perspect Vasc Surg Endovasc Ther 18:55–62
Rodrigues TL, Marchesan JT, Coletta RD, Novaes Jr AB, Grisi MF, Souza SL, Taba Jr M, Palioto DB (2007) Effects of enamel matrix derivative and transforming growth factor-beta 1 on human periodontal ligament fibroblasts. J Clin Periodontol 34:514–522
Van der Pauw MT, Van den Bos T, Everts V, Beertsen W (2000) Enamel matrix-derived protein stimulates attachment of periodontal ligament fibroblasts and enhances alkaline phosphatase activity and transforming growth factor beta1 release of periodontal ligament and gingival fibroblasts. J Periodontol 71:31–43
Okubo K, Kobayashi M, Takiguchi T, Takada T, Ohazama A, Okamatsu Y, Hasegawa K (2003) Participation of endogenous IGF-I and TGF-beta 1 with enamel matrix derivative-stimulated cell growth in human periodontal ligament cells. J Periodontal Res 38:1–9
Acknowledgments
This study was partly supported by Grants-in-Aid for Scientific Research (C) (No. 25463052) from the Ministry of Education, Science, Sports and Culture of Japan. Porcine acellular dermal matrix (PADM: Mucoderm®) was provided free of charge by Botiss Dental, Berlin, Germany.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was partly supported by Grants-in-Aid for Scientific Research (C) (No. 25463052) from the Ministry of Education, Science, Sports and Culture of Japan.
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The procedures and protocol design described here were approved by the ethical committee of the Animal Research Center of Kagoshima University, Japan (MD13164).
Rights and permissions
About this article
Cite this article
Shirakata, Y., Sculean, A., Shinohara, Y. et al. Healing of localized gingival recessions treated with a coronally advanced flap alone or combined with an enamel matrix derivative and a porcine acellular dermal matrix: a preclinical study. Clin Oral Invest 20, 1791–1800 (2016). https://doi.org/10.1007/s00784-015-1680-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1680-4