Abstract
Objectives
To evaluate the influence of restorative materials used on the rehabilitation of MOD cavities and loading type, on biomechanical behavior of wedge-shaped (WS) lesions in endodontically treated maxillary premolars. The investigation was conducted by 3D finite element analysis (FEA) and strain gauge test.
Materials and methods
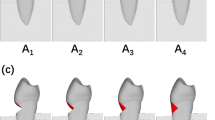
Six models were generated, with MOD cavities and endodontic treatment: A (MOD amalgam restoration), R (MOD composite restoration), AL (A + cervical lesion (L)), RL, ALR (A + cervical lesion restored with composite (LR)), and RLR. Each model underwent two compressive loading (100N): axial and oblique—45° angle to the long axis on the buccal cusp. The models were analyzed by von Mises criteria. For strain gauge test, 14 standardized maxillary premolars were treated according to the groups described for FEA. Two strain gauges were bonded on each sample submitted to compressive loading in a mechanical testing machine.
Results
A presented higher stress concentration and strain values than R. Oblique loading promoted highest stress concentration and strain rates for all groups. ALR and RLR presented similar stress–strain distribution pattern when compared to A and R.
Conclusion
The interaction between MOD cavity restored with amalgam and oblique loading propitiated the highest stress concentration and strain values on cervical region and WS lesion.
Clinical relevance
The MOD cavity restored with composite resin is a better option than amalgam to improve the biomechanical behavior of wedge-shaped lesion, avoiding dental failure. In addition, the occlusal interferences must be removed, allowing homogeneous contact distribution and preventing WS lesion progression.






Similar content being viewed by others
References
Grippo JO, Simring M, Coleman TA (2012) Abfraction, abrasion, biocorrosion, and the enigma of noncarious cervical lesions: a 20-year perspective. J Esthet Restor Dent 24:10–23
Antonelli JR, Hottel TL, Garcia-Godoy F. Abfraction lesions—where do they come from? A review of the literature. J Tenn Dent Assoc 93:14–19
Bartlett DW, Shah P (2006) A critical review of non-carious cervical (wear) lesions and the role of abfraction, erosion, and abrasion. J Dent Res 85:306–312
Michael JA, Townsend GC, Greenwood LF, Kaidonis JA (2009) Abfraction: separating fact from fiction. Aust Dent J 54:2–8
Benazzi S, Grosse IR, Gruppioni G, Weber GW, Kullmer O (2014) Comparison of occlusal loading conditions in a lower second premolar using three-dimensional finite element analysis. Clin Oral Investig 18:369–375
Ommerborn MA, Schneider C, Giraki M, Schafer R, Singh P, Franz M, Raab WH (2007) In vivo evaluation of noncarious cervical lesions in sleep bruxism subjects. J Prosthet Dent 98:150–158
Staninec M, Nalla RK, Hilton JF, Ritchie RO, Watanabe LG, Nonomura G, Marshall GW, Marshall SJ (2005) Dentin erosion simulation by cantilever beam fatigue and pH change. J Dent Res 84:371–375
Bernhardt O, Gesch D, Schwahn C, Mack F, Meyer G, John U, Kocher T (2006) Epidemiological evaluation of the multifactorial aetiology of abfractions. J Oral Rehabil 33:17–25
Soares PV, Santos-Filho PC, Gomide HA, Araujo CA, Martins LR, Soares CJ (2008) Influence of restorative technique on the biomechanical behavior of endodontically treated maxillary premolars. Part II: strain measurement and stress distribution. J Prosthet Dent 99:114–122
Shafiei F, Memarpour M, Karimi F (2011) Fracture resistance of cuspal coverage of endodontically treated maxillary premolars with combined composite-amalgam compared to other techniques. Oper Dent 36:439–447
Brandini DA, Trevisan CL, Panzarini SR, Pedrini D (2012) Clinical evaluation of the association between noncarious cervical lesions and occlusal forces. J Prosthet Dent 108:298–303
Daley TJ, Harbrow DJ, Kahler B, Young WG (2009) The cervical wedge-shaped lesion in teeth: a light and electron microscopic study. Aust Dent J 54:212–219
Reyes E, Hildebolt C, Langenwalter E, Miley D (2009) Abfractions and attachment loss in teeth with premature contacts in centric relation: clinical observations. J Periodontol 80:1955–1962
Telles D, Pegoraro LF, Pereira JC (2000) Prevalence of noncarious cervical lesions and their relation to occlusal aspects: a clinical study. J Esthet Dent 12:10–15
Walter C, Kress E, Gotz H, Taylor K, Willershausen I, Zampelis A (2014) The anatomy of non-carious cervical lesions. Clin Oral Investig 18:139–146
Lee WC, Eakle WS (1984) Possible role of tensile stress in the etiology of cervical erosive lesions of teeth. J Prosthet Dent 52:374–380
Palamara D, Palamara JE, Tyas MJ, Pintado M, Messer HH (2001) Effect of stress on acid dissolution of enamel. Dent Mater 17:109–115
Grippo JO, Chaiyabutr Y, Kois JC (2013) Effects of cyclic fatigue stress-biocorrosion on noncarious cervical lesions. J Esthet Restor Dent 25:265–272
Wood ID, Kassir AS, Brunton PA (2009) Effect of lateral excursive movements on the progression of abfraction lesions. Oper Dent 34:273–279
Brandini DA, Pedrini D, Panzarini SR, Benete IM, Trevisan CL (2012) Clinical evaluation of the association of noncarious cervical lesions, parafunctional habits, and TMD diagnosis. Quintessence Int 43:255–262
McCoy G (1983) On the longevity of teeth. J Oral Implantol 11:248–267
Rees JS (2002) The effect of variation in occlusal loading on the development of abfraction lesions: a finite element study. J Oral Rehabil 29:188–193
Dejak B, Mlotkowski A, Romanowicz M (2005) Finite element analysis of mechanism of cervical lesion formation in simulated molars during mastication and parafunction. J Prosthet Dent 94:520–529
Zucchelli G, Gori G, Mele M, Stefanini M, Mazzotti C, Marzadori M, Montebugnoli L, De Sanctis M (2011) Non-carious cervical lesions associated with gingival recessions: a decision-making process. J Periodontol 82:1713–1724
Miller N, Penaud J, Ambrosini P, Bisson-Boutelliez C, Briancon S (2003) Analysis of etiologic factors and periodontal conditions involved with 309 abfractions. J Clin Periodontol 30:828–832
Smith WAJ, Marchan S, Rafeek RN (2008) The prevalence and severity of non-carious cervical lesions in a group of patients attending a university hospital in Trinidad. J Oral Rehabil 35:128–134
Soares PV, Verissimo C, Zeola LF, Pereira AG, Santos-Filho PCF, Fernandes-Neto AJ (2014) Effect of root morphology on biomechanical behaviour of premolars associated with abfraction lesions and different loading types. J Oral Rehabil 41:108–114
Rees JS, Hammadeh M, Jagger DC (2003) Abfraction lesion formation in maxillary incisors, canines and premolars: a finite element study. Eur J Oral Sci 111:149–154
Piotrowski BT, Gillette WB, Hancock EB (2001) Examining the prevalence and characteristics of abfractionlike cervical lesions in a population of U.S. veterans. J Am Dent Assoc 132:1694–1701, quiz 1726–1697
van Driel WD, van Leeuwen EJ, Von den Hoff JW, Maltha JC, Kuijpers-Jagtman AM (2000) Time-dependent mechanical behaviour of the periodontal ligament. Proc Inst Mech Eng H 214:497–504
Wang RZ, Weiner S (1998) Strain-structure relations in human teeth using Moire fringes. J Biomech 31:135–141
Ho SP, Balooch M, Goodis HE, Marshall GW, Marshall SJ (2004) Ultrastructure and nanomechanical properties of cementum dentin junction. J Biomed Mater Res A 68:343–351
Ho SP, Yu B, Yun W, Marshall GW, Ryder MI, Marshall SJ (2009) Structure, chemical composition and mechanical properties of human and rat cementum and its interface with root dentin. Acta Biomater 5:707–718
Rees JS (1998) The role of cuspal flexure in the development of abfraction lesions: a finite element study. Eur J Oral Sci 106:1028–1032
Magne P (2007) Efficient 3D finite element analysis of dental restorative procedures using micro-CT data. Dent Mater 23:539–548
Jiang W, Bo H, Yongchun G, LongXing N (2010) Stress distribution in molars restored with inlays or onlays with or without endodontic treatment: a three-dimensional finite element analysis. J Prosthet Dent 103:6–12
Sagsen B, Aslan B (2006) Effect of bonded restorations on the fracture resistance of root filled teeth. Int Endod J 39:900–904
Reeh ES, Messer HH, Douglas WH (1989) Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod 15:512–516
Soares PV, Santos-Filho PC, Soares CJ, Faria VL, Naves MF, Michael JA, Kaidonis JA, Ranjitkar S, Townsend GC (2013) Non-carious cervical lesions: influence of morphology and load type on biomechanical behaviour of maxillary incisors. Aust Dent J 58:306–314
Guimaraes JC, Guimaraes Soella G, Brandao Durand L, Horn F, Narciso Baratieri L, Monteiro S Jr, Belli R (2014) Stress amplifications in dental non-carious cervical lesions. J Biomech 47:410–416
Peumans M, De Munck J, Van Landuyt KL, Poitevin A, Lambrechts P, Van Meerbeek B (2012) A 13-year clinical evaluation of two three-step etch-and-rinse adhesives in non-carious class-V lesions. Clin Oral Investig 16:129–137
Burrow MF, Tyas MJ (2012) Comparison of two all-in-one adhesives bonded to non-carious cervical lesions--results at 3 years. Clin Oral Investig 16:1089–1094
Grippo JO (1992) Noncarious cervical lesions: the decision to ignore or restore. J Esthet Dent 4(Suppl):55–64
Efeoglu A, Hanzade M, Sari E, Alpay H, Karakas O, Koray F (2012) Combined periodontal and restorative approach to the treatment of gingival recessions with noncarious cervical lesions: a case treated with acellular dermal matrix allograft and compomer restorations. Int J Periodontics Restorative Dent 32:441–448
Ichim I, Li Q, Loughran J, Swain MV, Kieser J (2007) Restoration of non-carious cervical lesions part I. Modelling of restorative fracture. Dent Mater 23:1553–1561
Francisconi LF, Graeff MS, Martins Lde M, Franco EB, Mondelli RF, Francisconi PA, Pereira JC (2009) The effects of occlusal loading on the margins of cervical restorations. J Am Dent Assoc 140:1275–1282
Acknowledgments
The authors thank the NCCL Research Group from Dental School, and CPbio (Integrated Dental Research Laboratory), Federal University of Uberlandia, Brazil, for the structure offered to perform the strain gauge test. This study was supported by grants from the CAPES/MEC Federal Govern of Brazil and CNPq by grant #454453/2014-0.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Video 1
Finite element 3D-Model AL with Oblique Load. The amalgam restoration of MOD cavity was hided for demonstration of internal stress distribution. Observe the high stress concentration inside of MOD cavity and bottom of WS cervical lesion. (AVI 6061 kb)
Video 2
Finite element 3D-Model RL with Oblique Load. The composite resin restoration of MOD cavity was hided for demonstration of internal stress distribution. Observe that the stress concentration inside was reduced, but due Oblique Load there are stresses concentration in WS cervical lesion. (AVI 6458 kb)
Video 3
Finite element 3D-Model AL with Axial Load. The amalgam restoration of MOD cavity was hided for demonstration of internal stress distribution. Observe the reduction of stress concentration in cervical region, but the WS lesion needs of composite resin restoration. (AVI 4046 kb)
Video 4
Finite element 3D-Model RL with Axial Load. The composite resin restoration of MOD cavity was hided for demonstration of internal stress distribution. Observe the lowest stress concentration in cervical region, but the WS lesion needs of composite resin restoration. (AVI 4277 kb)
Video 5
Finite element 3D-Model RLR with Axial Load. The composite resin restoration of MOD cavity and WS cervical lesion were hided for demonstration of internal stress distribution. This model represent the satisfactory clinical situation, with MOD and WS lesion restored and axial load direction. (AVI 3378 kb)
Rights and permissions
About this article
Cite this article
Pereira, F.A., Zeola, L.F., de Almeida Milito, G. et al. Restorative material and loading type influence on the biomechanical behavior of wedge shaped cervical lesions. Clin Oral Invest 20, 433–441 (2016). https://doi.org/10.1007/s00784-015-1523-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1523-3