Abstract
Objectives
A comparison of different treatment modalities of peri-implantitis can lead to the development and application of more effective and efficient methods of therapy in clinical practice. This study compares the effectiveness of open flap debridement used alone, with an approach employing the additional use of a diode laser for the treatment of peri-implantitis.
Materials and methods
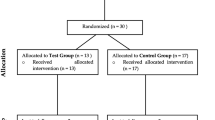
Nineteen patients were divided into two groups and treated for peri-implantitis. In the control group (C group), the therapy utilized access flaps, plastic curettes, and sterilized gauzes soaked in saline. The test group (L group) was treated similarly but with additional irradiation using a diode laser. The parameters studied were pocket depth (PD) as the primary outcome variable, clinical attachment level (CAL), bleeding on probing (BOP), and plaque index (PI) as secondary variables. Measurements were performed at three different time points, baseline (BSL), 3 months, and 6 months after treatment. Three months after treatment, a mean PD reduction of 1.19 mm for the control group and 1.38 mm for the laser group was recorded. The corresponding BOP changes were 72.9 and 66.7 %, respectively. These changes were significant and remained at the same levels at the 6-month examination (p < 0.05). CAL was reduced significantly only in group L from 5.25 mm at baseline to 4.54 mm at 3 months, remaining at this level at 6 months (p < 0.05). PI was reduced significantly in group C at 3 months from 37.5 to 6.3 %. The 6-month data showed no statistically significant difference (p < 0.05) from the 3-month measurements.
Results
The two methods of therapy for peri-implantitis examined seemed to be equally efficient in the reduction of the PD and BOP 3 months after surgery, with the results sustained at the same levels after 6 months. CAL significantly improved only in the test group after 3 months. PI was reduced and maintained at low levels in both groups.
Conclusions
Surgical treatment of peri-implantitis by access flaps leads to improvement of all clinical parameters studied while the additional use of diode laser does not seem to have an extra beneficiary effect.
Clinical relevance
The additional use of a diode laser in the surgical treatment of peri-implantitis offers a limited clinical benefit.











Similar content being viewed by others
References
Brånemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, Ohman A (1977) Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg 16:1–132
Zarb GA (1983) A status report on dental implants. J Can Dent Assoc 49:841–843
Zitzmann NU, Berglundh T (2008) Definition and prevalence of peri-implant diseases. J Clin Periodontol 35:286–291
Hultin M, Gustafsson A, Hallström H, Johansson LA, Ekfeldt A, Klinge B (2002) Microbiological findings and host response in patients with peri-implantitis. Clin Oral Implants Res 13:349–358
Leonhardt A, Renvert S, Dahlén G (1999) Microbial findings at failing implants. Clin Oral Implants Res 10:339–345
Becker W, Becker BE, Newman MG, Nyman S (1990) Clinical and microbiologic findings that may contribute to dental implant failure. Int J Oral Maxillofac Implants 5:31–38
Rams TE, Feik D, Slots J (1990) Staphylococci in human periodontal diseases. Oral Microbiol Immunol 5:29–32
Rosenberg ES, Torosian JP, Slots J (1991) Microbial differences in 2 clinically distinct types of failures of osseointegrated implants. Clin Oral Implants Res 2:135–144
Mombelli A, Lang NP (1992) Antimicrobial treatment of peri-implant infections. Clin Oral Implants Res 3:162–168
Salcetti JM, Moriarty JD, Cooper LF, Smith FW, Collins JG, Socransky SS, Offenbacher S (1997) The clinical, microbial, and host response characteristics of the failing implant. Int J Oral Maxillofac Implants 12:32–42
Mombelli A, van Oosten MA, Schurch E Jr, Land NP (1987) The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol 2:145–151
Roos-Jansåker AM, Renvert S, Egelberg J (2003) Treatment of peri-implant infections: a literature review. J Clin Periodontol 30:467–485
Kotsovilis S, Karoussis IK, Trianti M, Fourmousis I (2008) Therapy of peri-implantitis: a systematic review. J Clin Periodontol 35:621–629
Esposito M, Grusovin MG, Tzanetea E, Piattelli A, Worthington HV (2010) Interventions for replacing missing teeth: treatment of perimplantitis. Cochrane Database Syst Rev 16, CD004970
Bories C, Struillou X, Badran Z, Soueidan A (2011) Peri-implantitis: tools and techniques for disinfecting the implant surface. Schweiz Monatsschr Zahnmed 121:341–355
Ishikawa I, Aoki A, Takasaki AA, Mizutani K, Sasaki KM, Izumi Y (2009) Application of lasers in periodontics: true innovation or myth? Periodontol 50:90–126, 2000
Romanos GE, Nentwig GH (2008) Regenerative therapy of deep peri-implant infrabony defects after CO2 laser implant surface decontamination. Int J Periodontics Restor Dent 28:245–255
Giannini R, Vassalli M, Chellini F, Polidori L, Dei R, Giannelli M (2006) Neodymium: yttrium aluminum garnet laser irradiation with low pulse energy: a potential tool for the treatment of peri-implant disease. Clin Oral Implants Res 17:638–643
Kreisler M, Götz H, Duschner H (2002) Effect of Nd:YAG, Ho:YAG, Er:YAG, CO2, and GaAIAs laser irradiation on surface properties of endosseous dental implants. Int J Oral Maxillofac Implants 17:202–211
Schwarz F, Bieling K, Nuesry E, Sculean A, Becker J (2006) Clinical and histological healing pattern of peri-implantitis lesions following non-surgical treatment with an Er:YAG laser. Lasers Surg Med 38:663–671
Schwarz F, Bieling K, Bonsmann M, Latz T, Becker J (2006) Nonsurgical treatment of moderate and advanced periimplantitis lesions: a controlled clinical study. Clin Oral Investig 10:279–288
Schwarz F, Sahm N, Iglhaut G, Becker J (2011) Impact of the method of surface debridement and decontamination on the clinical outcome following combined surgical therapy of peri-implantitis: a randomized controlled clinical study. J Clin Periodontol 38:276–284
Persson GR, Roos-Jansåker AM, Lindahl C, Renvert S (2011) Microbiologic results after non-surgical erbium-doped:yttrium, aluminum, and garnet laser or air-abrasive treatment of peri-implantitis: a randomized clinical trial. J Periodontol 82:1267–1278
Renvert S, Lindahl C, Roos Jansåker AM, Persson GR (2011) Treatment of peri-implantitis using an Er:YAG laser or an air-abrasive device: a randomized clinical trial. J Clin Periodontol 38:65–73
Romanos GE, Everts H, Nentwig GH (2000) Effects of diode and Nd:YAG laser irradiation on titanium discs: a scanning electron microscope examination. J Periodontol 71:810–815
Romeo E, Ghisolfi M, Murgolo N, Chiapasco M, Lops D, Vogel G (2005) Therapy of peri-implantitis with resective surgery. A 3-year clinical trial on rough screw-shaped oral implants. Part I: clinical outcome. Clin Oral Implants Res 16:9–18
Romeo E, Lops D, Chiapasco M, Ghisolfi M, Vogel G (2007) Therapy of peri-implantitis with resective surgery. A 3-year clinical trial on rough screw-shaped oral implants. Part II: radiographic outcome. Clin Oral Implants Res 18:179–187
Serino G, Turri A (2011) Outcome of surgical treatment of peri-implantitis: results from a 2-year prospective clinical study in humans. Clin Oral Implants Res 22:1214–1220
Schwarz F, John G, Mainusch S, Sahm N, Becker J (2012) Combined surgical therapy of peri-implantitis evaluating two methods of surface debridement and decontamination. A two-year clinical follow up report. J Clin Periodontol 39:789–797
Schwarz F, Bieling K, Latz T, Nuesry E, Becker J (2006) Healing of intrabony peri-implantitis defects following application of a nanocrystalline hydroxyapatite (Ostim) or a bovine-derived xenograft (Bio-Oss) in combination with a collagen membrane (Bio-Gide). A case series. J Clin Periodontol 33:491–499
Behneke A, Behneke N, d’Hoedt B (2000) Treatment of peri-implantitis defects with autogenous bone grafts: six-month to 3-year results of a prospective study in 17 patients. Int J Oral Maxillofac Implants 15:125–138
Haas R, Baron M, Dörtbudak O, Watzek G (2000) Lethal photosensitization, autogenous bone, and e-PTFE membrane for the treatment of peri-implantitis: preliminary results. Int J Oral Maxillofac Implants 15:374–382
Roccuzzo M, Bonino F, Bonino L, Dalmasso P (2011) Surgical therapy of peri-implantitis lesions by means of a bovine-derived xenograft: comparative results of a prospective study on two different implant surfaces. J Clin Periodontol 38:738–745
Khoury F, Buchmann R (2001) Surgical therapy of peri-implant disease: a 3-year follow-up study of cases treated with 3 different techniques of bone regeneration. J Periodontol 72:1498–1508
Roos-Jansåker AM, Renvert H, Lindahl C, Renvert S (2007) Surgical treatment of peri-implantitis using a bone substitute with or without a resorbable membrane: a prospective cohort study. J Clin Periodontol 34:625–632
Roos-Jansåker AM, Renvert H, Lindahl C, Renvert S (2007) Submerged healing following surgical treatment of peri-implantitis: a case series. J Clin Periodontol 34:723–727
Schwarz F, Sculean A, Bieling K, Ferrari D, Rothamel D, Becker J (2008) Two-year clinical results following treatment of peri-implantitis lesions using a nanocrystalline hydroxyapatite or a natural bone mineral in combination with a collagen membrane. J Clin Periodontol 35:80–87
Schwarz F, Sahm N, Bieling K, Becker J (2009) Surgical regenerative treatment of peri-implantitis lesions using a nanocrystalline hydroxyapatite or a natural bone mineral in combination with a collagen membrane: a four-year clinical follow-up report. J Clin Periodontol 36:807–814
Roos-Jansåker AM, Lindahl C, Persson GR, Renvert S (2011) Long-term stability of surgical bone regenerative procedures of peri-implantitis lesions in a prospective case–control study over 3 years. J Clin Periodontol 38:590–597
Shibli JA, Martins MC, Theodoro LH, Lotufo RF, Garcia VG, Marcantonio EJ (2003) Lethal photosensitization in microbiological treatment of ligature-induced peri-implantitis: a preliminary study in dogs. J Oral Sci 45:17–23
Shibli JA, Martins MC, Ribeiro FS, Garcia VG, Nociti FH Jr, Marcantonio E Jr (2006) Lethal photosensitization and guided bone regeneration in treatment of peri-implantitis: an experimental study in dogs. Clin Oral Implants Res 17:273–281
Hayek RR, Araújo NS, Gioso MA, Ferreira J, Baptista-Sobrinho CA, Yamada AM, Ribeiro MS (2005) Comparative study between the effects of photodynamic therapy and conventional therapy on microbial reduction in ligature-induced peri-implantitis in dogs. J Periodontol 76:1275–1281
Dörtbudak O, Haas R, Bernhart T, Mailath-Pokorny G (2001) Lethal photosensitization for decontamination of implant surfaces in the treatment of peri-implantitis. Clin Oral Implants Res 12:104–108
Deppe H, Horch HH, Neff A (2007) Conventional versus CO2 laser-assisted treatment of peri-implant defects with the concomitant use of pure-phase beta-tricalcium phosphate: a 5-year clinical report. Int J Oral Maxillofac Implants 22:79–86
Schwarz F, Sculean A, Rothamel D, Schwenzer K, Georg T, Becker J (2005) Clinical evaluation of an Er:YAG laser for nonsurgical treatment of peri-implantitis: a pilot study. Clin Oral Implants Res 16:44–52
Schuklenk U (2001) Helsinki declaration revisions. Issues Med Ethics 9:29
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41:1149–1160
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25:229–235
O’Lery TJ, Drake RB, Naylor JE (1972) The plaque control record. J Periodontol 43:38–40
West BT, Welch KB, Galecki AT (2007) Linear mixed models: a practical guide to using statistical software. Chapman & Hall/CRC, New York
Bach G, Neckel C, Mall C, Krekeler G (2000) Conventional versus laser-assisted therapy of periimplantitis: a five-year comparative study. Implant Dent 9:247–251
Schwarz F, Jepsen S, Herten M, Sager M, Rothamel D, Becker J (2006) Influence of different treatment approaches on non-submerged and submerged healing of ligature induced peri-implantitis lesions: an experimental study in dogs. J Clin Periodontol 33:584–595
Leonhardt A, Dahlén G, Renvert S (2003) Five-year clinical, microbiological, and radiological outcome following treatment of peri-implantitis in man. J Periodontol 74:1415–1422
Máximo MB, de Mendonça AC, Renata Santos V, Figueiredo LC, Feres M, Duarte PM (2009) Short-term clinical and microbiological evaluations of peri-implant diseases before and after mechanical anti-infective therapies. Clin Oral Implants Res 20:99–108
Duarte PM, de Mendonça AC, Máximo MB, Santos VR, Bastos MF, Nociti FH (2009) Effect of anti-infective mechanical therapy on clinical parameters and cytokine levels in human peri-implant diseases. J Periodontol 80:234–243
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Papadopoulos, C.A., Vouros, I., Menexes, G. et al. The utilization of a diode laser in the surgical treatment of peri-implantitis. A randomized clinical trial. Clin Oral Invest 19, 1851–1860 (2015). https://doi.org/10.1007/s00784-014-1397-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-014-1397-9