Abstract
Objectives
The success of ridge preservation techniques in reducing bone resorption is well documented, but no clear guidelines have been provided regarding the type of the biomaterial or technique to be used. This experimental animal study aimed at comparing the effectiveness of two ridge preservation techniques.
Materials and methods
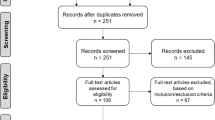
Following the extraction of the distal roots of the mandibular second and fourth premolars of four dogs, the sockets were preserved using a combination of a collagen membrane intimately covering the socket plus a collagen matrix or a collagen membrane alone. The mandibular quadrants were randomly assigned to one of the treatment groups. Histomorphometrical analyses as well as microscopic observations were performed.
Results
After 5 months of healing, the histological analysis revealed a similar picture of bone formation in both groups. No significant differences between the buccal and lingual dimensions were calculated between the two treatment groups. The mucosa covering the alveolar ridges is significantly more abundant in post-extraction sockets preserved with the double-layered approach.
Conclusions
The double-layered approach used to treat post-extraction sockets may result in a better preservation of the mucosal seal than the single-layered approach.
Clinical relevance
The use of the new collagen matrix associated with a collagen membrane could be a clinical option to preserve post-extraction ridges, especially when an improvement in soft tissue dimension and quality is desired. However, the cost-benefit ratio of this approach should be thoroughly evaluated in further studies.





Similar content being viewed by others
References
Leblebicioglu B, Salas M, Ort Y, Johnson A, Yildiz VO, Kim DG, Agarwal S, Tatakis DN (2013) Determinants of alveolar ridge preservation differ by anatomic location. J Clin Periodontol 40:387–395
Tan WL, Wong TL, Wong MC, Lang NP (2012) A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res 23(Suppl 5):1–21
Pinho MN, Roriz VL, Novaes AB Jr, Taba M Jr, Grisi MF, de Souza SL, Palioto DB (2006) Titanium membranes in prevention of alveolar collapse after tooth extraction. Implant Dent 15:53–61
Botticelli D, Berglundh T, Lindhe J (2004) Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol 31:820–828
Lambert F, Vincent K, Vanhoutte V, Seidel L, Lecloux G, Rompen E (2012) A methodological approach to assessing alveolar ridge preservation procedures in humans: hard tissue profile. J Clin Periodontol 39:887–894
Reichert C, Wenghöfer M, Götz W, Jäger A (2011) Pilot study on orthodontic space closure after guided bone regeneration. J Orofac Orthop 72:45–50. doi:10.1007/s00056-010-0006-z
Tarnow DP, Eskow RN (1996) Preservation of implant esthetics: soft tissue and restorative considerations. J Esthet Dent 8:12–19
Jung RE, Philipp A, Annen BM, Signorelli L, Thoma DS, Hämmerle CH, Attin T, Schmidlin P (2013) Radiographic evaluation of different techniques for ridge preservation after tooth extraction: a randomized controlled clinical trial. J Clin Periodontol 40:90–98
Poulias E, Greenwell H, Hill M, Morton D, Vidal R, Shumway B, Peterson TL (2013) Ridge preservation comparing a socket allograft alone to a socket allograft plus a facial overlay xenograft: a clinical and Histologic study in humans. J Periodontol 84:1567–1575
Ten Heggeler JM, Slot DE, Van der Weijden GA (2011) Effect of socket preservation therapies following tooth extraction in non-molar regions in humans: a systematic review. Clin Oral Implants Res 22:779–788
Horowitz R, Holtzclaw D, Rosen PS (2012) A review on alveolar ridge preservation following tooth extraction. J Evid Based Dent Pract 2(Suppl 3):149–160
Vignoletti F, Matesanz P, Figuero E, Martin C, Sanz M (2012) Surgical protocols for ridge preservation after tooth extraction. A systematic review. Clin Oral Implant Res 23(Suppl 5):22–38
Barone A, Toti P, Piattelli A, Iezzi G, Derchi G, Covani U (2014) Extraction socket healing in humans after ridge preservation techniques: a comparison between flapless and flapped procedure in a randomized clinical trial. J Periodontol 85:14–23
Darby I, Chen ST, Buser D Ridge preservation techniques for implant therapy. Int J Oral Maxillofac Implants (Suppl 24):260–71
Vittorini Orgeas G, Clementini M, De Risi V, de Sanctis M (2013) Surgical techniques for alveolar socket preservation: a systematic review. Int J Oral Maxillofac Implants 28:1049–1061
McGuire MK, Scheyer ET (2010) Xenogeneic collagen matrix with coronally advanced flap compared to connective tissue with coronally advanced flap for the treatment of dehiscence-type recession defects. J Periodontol 81:1108–1117
Vignoletti F, Nuñez J, Discepoli N, De Sanctis F, Caffesse R, Muñoz F, Lopez M, Sanz M (2011) Clinical and histological healing of a new collagen matrix in combination with the coronally advanced flap for the treatment of Miller class-I recession defects: an experimental study in the minipig. J Clin Periodontol 38:847–855
Sanz M, Lorenzo R, Aranda JJ, Martin C, Orsini M (2009) Clinical evaluation of a new collagen matrix (Mucograft prototype) to enhance the width of keratinized tissue in patients with fixed prosthetic restorations: a randomized prospective clinical trial. J Clin Periodontol 36:868–876
Nevins M, Nevins ML, Camelo M, Camelo JM, Schupbach P, Kim DM (2010) The clinical efficacy of DynaMatrix extracellular membrane in augmenting keratinized tissue. Int J Periodontics Restor Dent 30:151–161
Jung RE, Hürzeler MB, Thoma DS, Khraisat A, Hämmerle CH (2010) Local tolerance and efficiency of two prototype collagen matrices to increase the width of keratinized tissue. J Clin Periodontol 38:173–179
Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG (2010) Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol 29(8):e1000412. doi:10.1371/journal.pbio.1000412
COUNCIL DIRECTIVE of 24 November 1986 on the approximation of laws, regulations and administrative provisions of the Member States regarding the protection of animals used for experimental and other scientific purposes (86/609/EEC) ec.europa.eu/…/scientific/86-609-eec_en.pdf
Faggion CM Jr, Giannakopoulos NN, Listl S (2011) Risk of bias of animal studies on regenerative procedures for periodontal and peri-implant bone defects—a systematic review. J Clin Periodontol 38:1154–1160
Araujo MG, Silva CO, Mesti JC (2011) Ridge preservation, cpt 9. In: Giannobile WV, Nevins M (eds) Osteology guidelines for oral and maxillofacial regeneration. Preclinical models for translational models, Quintessence Publishing, pp. 123-139
Cioban C, Zăgănescu R, Roman A, Muste A, Beteg F, Câmpian RS, Boşca B (2013) Early healing after ridge preservation with a new collagen matrix in dog extraction sockets: preliminary observations. Rom J Morphol Embryol 54:125–130
Karnovsky MJ (1965) A formaldehyde-glutaraldehyde fixative of high osmolarity for use in electron microscopy. J Cell Biol 27:137A–138A
Donath K (1982) A method for the study of undecalcified bones and teeth with attached soft tissue. The Säge-Schliff (sawing and grinding) technique). J Oral Pathol 11:318–326
Erdfelder E, Faul F, Buchner A (1996) GPOWER: a general power analysis program. Behav Res Methods Instrum Comput 28:1–11
Cohen J (1994) The earth is round (p < .05). Am Psychol 49:997–1003
Cook DC, Mealey BL (2013) Histologic comparison of healing following tooth extraction with ridge preservation using two different xenograft protocols. J Periodontol 84:585–594
Araújo MG, Lindhe J (2005) Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol 32:212–218
Araújo MG, Lindhe J (2009) Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog. Clin Oral Implants Res 20:545–549
Araújo MG, Lindhe J (2009) Ridge preservation with the use of Bio-Oss collagen: a 6-month study in the dog. Clin Oral Implants Res 20:433–440
Brownfield LA, Weltman RL (2012) Ridge preservation with or without an osteoinductive allograft: a clinical, radiographic, micro-computed tomography, and histologic study evaluating dimensional changes and new bone formation of the alveolar ridge. J Periodontol 83:581–589
Lekovic V, Camargo PM, Klokkevold PR, Weinlaender M, Kenney EB, Dimitrijevic B, Nedic M (1998) Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. J Periodontol 69:1044–1049
Bashara H, Wohlfahrt JC, Polyzois I, Lyngstadaas SP, Renvert S, Claffey N (2012) The effect of permanent grafting materials on the preservation of the buccal bone plate after tooth extraction: an experimental study in the dog. Clin Oral Implants Res 23:911–917
Cardaropoli G, Araújo M, Lindhe J (2003) Dynamics of bone tissue formation in tooth extraction sites. An experimental study in dogs. J Clin Periodontol 30:809–818
Rothamel D, Schwarz F, Herten M, Engelhardt E, Donath K, Kuehn P, Becker J (2008) Dimensional ridge alterations following socket preservation using a nanocrystalline hydroxyapatite paste: a histomorphometrical study in dogs. Int J Oral Maxillofac Surg 37:741–747
Moses O, Vitrial D, Aboodi G, Sculean A, Tal H, Kozlovsky A, Artzi Z, Weinreb M, Nemcovsky CE (2008) Biodegradation of three different collagen membranes in the rat calvarium: a comparative study. J Periodontol 79:905–911
Thoma DS, Villar CC, Cochran DL, Hämmerle CH, Jung RE (2012) Tissue integration of collagen-based matrices: an experimental study in mice. Clin Oral Implants Res 23:1333–1339
Bornstein MM, Bosshardt D, Buser D (2007) Effect of two different bioabsorbable collagen membranes on guided bone regeneration: a comparative histomorphometric study in the dog mandible. J Periodontol 78:1943–1953
Al-Asfour A, Tengvall P, Andersson L, Dahlin C (2013) Histologic analysis of a novel extracellullar matrix membrane for guided bone regeneration: an experimental study in rabbits. Int J Periodontics Restor Dent 33:177–183
Tatakis DN, Promsudthi A, Wikesjö UM (1999) Devices for periodontal regeneration. Periodontol 2000(19):59–73
Kim SH, Kim DY, Kim KH, Ku Y, Rhyu IC, Lee YM (2009) The efficacy of a double-layer collagen membrane technique for overlaying block grafts in a rabbit calvarium model. Clin Oral Implants Res 20:1124–1132
Al-Hezaimi K, Iezzi G, Rudek I, Al-Daafas A, Al-Hamdan K, Al-Rasheed A, Javed F, Piatelli A, Wang HL (2013) Histomorphometric analysis of bone regeneration using a dual-layer of membranes (dPTFE placed over collagen) in fresh extraction sites: In Canine Model. J Oral Implantol. [Epub ahead of print]
Ivanovic A, Bosshardt DD, Mihatovic I, Schwarz F, Gruber R, Sculean A (2013) Effect of pulverized natural bone mineral on regeneration of three-wall intrabony defects. A preclinical study. Clin Oral Investig. [Epub ahead of print]
Thoma DS, Hämmerle CH, Cochran DL, Jones AA, Görlach C, Uebersax L, Mathes S, Graf-Hausner U, Jung RE (2011) Soft tissue volume augmentation by the use of collagen-based matrices in the dog mandible—a histological analysis. J Clin Periodontol 38:1063–1070
Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L (2012) Treatment of gingival recession defects using coronally advanced flap with a porcine collagen matrix compared to coronally advanced flap with connective tissue graft: a randomized controlled clinical trial. J Periodontol 83:321–328
Camelo M, Nevins M, Nevins ML, Schupbach P, Kim DM (2012) Treatment of gingival recession defects with xenogenic collagen matrix: a histologic report. Int J Periodontics Restor Dent 32:167–173
Molnár B, Aroca S, Keglevich T, Gera I, Windisch P, Stavropoulos A, Sculean A (2013) Treatment of multiple adjacent Miller Class I and II gingival recessions with collagen matrix and the modified coronally advanced tunnel technique. Quintessence Int 44:17–24
Brägger U, Bürgin WB, Hämmerle CH, Lang NP (1997) Associations between clinical parameters assessed around implants and teeth. Clin Oral Implants Res 8:412–421
Artzi Z, Carmeli G, Kozlovsky A (2006) A distinguishable observation between survival and success rate outcome of hydroxyapatite-coated implants in 5–10 years in function. Clin Oral Implants Res 17:85–93
Zigdon H, Machtei EE (2008) The dimensions of keratinized mucosa around implants affect clinical and immunological parameters. Clin Oral Implants Res 19:387–392. doi:10.1111/j.1600-0501.2007.01492.x
Lin GH, Chan HL, Wang HL (2013) The significance of keratinized mucosa on implant health: a systematic review. J Periodontol 84:1755–1767
Thoma DS, Sancho-Puchades M, Ettlin DA, Hämmerle CH, Jung RE (2012) Impact of a collagen matrix on early healing, aesthetics and patient morbidity in oral mucosal wounds—a randomized study in humans. J Clin Periodontol 39:157–165
Schwarz F, Mihatovic I, Shirakata Y, Becker J, Bosshardt D, Sculean A (2012) Treatment of soft tissue recessions at titanium implants using a resorbable collagen matrix: a pilot study. Clin Oral Implants Res 23:83–89
Schmitt CM, Tudor C, Kiener K, Wehrhan F, Schmitt J, Eitner S, Agaimy A, Schlegel KA (2013) Vestibuloplasty: porcine collagen matrix versus free gingival graft: a clinical and histologic study. J Periodontol 84:914–923
Acknowledgments
The authors would like to thank Geistlich Biomaterials for providing unconditionally the materials for ridge preservations used in this study. Remaining costs were covered by a grant from the Iuliu Hatieganu University of Medicine and Pharmacy (No. 22714/10/06.10.2011) and partially by the authors.
The authors thank Dr. Florin Beteg and Marius-Mihai Muste for assistance with the follow-up of the animals after surgeries.
Conflict of interest
The authors declare that there are no conflicts of interest in this study.
Clinical relevance
Scientific rationale for the study. The success of ridge preservation techniques in reducing bone resorption and in providing more predictable implant rehabilitation outcomes is well documented in previous studies. However, no clear guideline has been provided regarding the type of the biomaterial to be used. In this animal study, the effect of two types of ridge preservation using a collagen membrane plus a collagen matrix vs. a collagen membrane was evaluated in terms of osseous and soft tissue dimensions and quality.
Principal findings. The double-layered ridge preservation approach may result in a better preservation of the mucosal seal than the single-layered approach.
Practical implications. The use of the new collagen matrix associated with a collagen membrane could be a clinical option to preserving post-extraction ridges especially when an improvement in soft tissue dimension and quality is desired. However, the cost-benefit ratio of this approach should be thoroughly evaluated in further studies.
Ethical standards
The manuscript does not contain clinical studies or patient data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roman, A., Cioban, C., Stratul, SI. et al. Ridge preservation using a new 3D collagen matrix: a preclinical study. Clin Oral Invest 19, 1527–1536 (2015). https://doi.org/10.1007/s00784-014-1368-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-014-1368-1