Abstract
Objectives
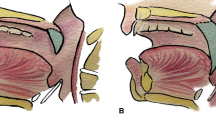
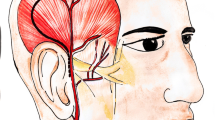
Successful reconstruction of palatomaxillary defects following cancer ablation represents a formidable challenge for surgeons to achieve consistently favorable outcomes. The purpose of this article is to present our experience in oncologic palatomaxillary repair with temporalis muscle flap (TMF) for medically compromised patients who are not ideal candidates for microvascular reconstruction at a Chinese tertiary referral hospital over a 15-year period (1998–2012).
Method
A retrospective chart review was performed to identify patients with compromised medical conditions who underwent oncologic palatomaxillary reconstruction using TMF. Patients’ demographics, clinicopathological variables, and surgical techniques were presented. Postoperative functional and aesthetic outcomes were assessed by measurements and patients self-evaluations.
Results
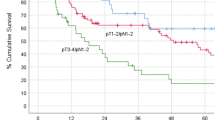
Sixty-nine TMFs were successfully harvested and used for immediate oncologic palatomaxillary reconstruction in 67 patients (31 males and 36 females, mean age 60.4 years) with diverse primary malignancies. These patients’ co-morbidities included systemic diseases, preoperative chemotherapy/radiotherapy, and elder over 65 years which precluded the ideal utility of free flaps. Fifty-one patients remained alive without disease, while nine had recurrences/metastases and seven died during the follow-up (0.5–10.4 years, mean 3.7 years). All flaps survived with only partial necroses in four cases. Complications and donor-site morbidities were minimal with five transient facial paralysis and four mild diplopia and enophthalmos. Unrestricted diet and mouth opening, intelligible speech, and satisfactory temporal aesthetics were obtained in most patients.
Conclusion
The TMF is a reliable, versatile, and alternative option for oncologic palatomaxillary reconstruction with satisfactory functional and aesthetic outcomes and minimal complications, especially when appropriately selected for those medically compromised patients.


Similar content being viewed by others
References
Andrades P, Militsakh O, Hanasono MM et al (2011) Current strategies in reconstruction of maxillectomy defects. Arch Otolaryngol Head Neck Surg 137:806–812
O'Connell DA, Futran ND (2010) Reconstruction of the midface and maxilla. Curr Opin Otolaryngol Head Neck Surg 18:304–310
Muzaffar AR, Adams WP Jr, Hartog JM et al (1999) Maxillary reconstruction: functional and aesthetic considerations. Plast Reconstr Surg 104:2172–2183
Futran ND, Mendez E (2006) Developments in reconstruction of midface and maxilla. Lancet Oncol 7:249–258
Kim JY, Buck DW 2nd, Johnson SA et al (2010) The temporoparietal fascial flap is an alternative to free flaps for orbitomaxillary reconstruction. Plast Reconstr Surg 126:880–888
Moreno MA, Skoracki RJ, Hanna EY et al (2010) Microvascular free flap reconstruction versus palatal obturation for maxillectomy defects. Head Neck 32:860–868
Santamaria E, Cordeiro PG (2006) Reconstruction of maxillectomy and midfacial defects with free tissue transfer. J Surg Oncol 94:522–531
Miles BA, Gilbert RW (2011) Maxillary reconstruction with the scapular angle osteomyogenous free flap. Arch Otolaryngol Head Neck Surg 137:1130–1135
Sun J, Shen Y, Li J et al (2011) Reconstruction of high maxillectomy defects with the fibula osteomyocutaneous flap in combination with titanium mesh or a zygomatic implant. Plast Reconstr Surg 127:150–160
Bianchi B, Ferri A, Ferrari S et al (2010) Iliac crest free flap for maxillary reconstruction. J Oral Maxillofac Surg 68:2706–2713
Kreeft AM, Krap M, Wismeijer D et al (2012) Oral function after maxillectomy and reconstruction with an obturator. Int J Oral Maxillofac Surg 41:1387–1392
Lethaus B, Lie N, de Beer F et al (2010) Surgical and prosthetic reconsiderations in patients with maxillectomy. J Oral Rehabil 37:138–142
Hashikawa K, Tahara S, Ishida H et al (2006) Simple reconstruction with titanium mesh and radial forearm flap after globe-sparing total maxillectomy: a 5-year follow-up study. Plast Reconstr Surg 117:963–967
Hanasono MM, Utley DS, Goode RL (2001) The temporalis muscle flap for reconstruction after head and neck oncologic surgery. Laryngoscope 111:1719–1725
Abu-El Naaj I, Leiser Y, Liberman R et al (2010) The use of the temporalis myofascial flap in oral cancer patients. J Oral Maxillofac Surg 68:578–583
Mani V, Panda AK (2003) Versatility of temporalis myofascial flap in maxillofacial reconstruction—analysis of 30 cases. Int J Oral Maxillofac Surg 32:368–372
Wong TY, Chung CH, Huang JS et al (2004) The inverted temporalis muscle flap for intraoral reconstruction: its rationale and the results of its application. J Oral Maxillofac Surg 62:667–675
Ward BB (2007) Temporalis system in maxillary reconstruction: temporalis muscle and temporoparietal galea flaps. Atlas Oral Maxillofac Surg Clin North Am 15:33–42
Xin SZ, Chen N, Wang LJ et al (1998) Immediate recostruction of maxillary defects with temporalis muscle flap. Acta Univeritatis Medicinalis Nanjing (Chin) 18:143–145
Wan LZ, Xin SZ, Zhu ZJ (2003) Long-term outcomes of oral and maxillofacial reconstruction with temporalis muscle flap. Acta Univeritatis Medicinalis Nanjing (Chin) 23:292–293
Shi XH, Xin SZ, Chen N et al (2004) Speech evaluation in patients with palatomaxillary defects recieving temporalis muscle flap reconstruction. J Stomatol (Chin) 24:355–356
Michaelidis IG, Hatzistefanou IM (2011) Functional and aesthetic reconstruction of extensive oral ablative defects using temporalis muscle flap: a case report and a sort review. J Craniomaxillofac Surg 39:200–205
Brown JS, Shaw RJ (2010) Reconstruction of the maxilla and midface: introducing a new classification. Lancet Oncol 11:1001–1008
Hanasono MM, Silva AK, Yu P, Skoracki RJ (2013) A comprehensive algorithm for oncologic maxillary reconstruction. Plast Reconstr Surg 131:47–60
Cordeiro PG, Chen CM (2012) A 15-year review of midface reconstruction after total and subtotal maxillectomy: part I. Algorithm and outcomes. Plast Reconstr Surg 129:124–136
McCarthy CM, Cordeiro PG (2010) Microvascular reconstruction of oncologic defects of the midface. Plast Reconstr Surg 126:1947–1959
Hill JB, Patel A, Del Corral GA et al (2012) Preoperative anemia predicts thrombosis and free flap failure in microvascular reconstruction. Ann Plast Surg 69:364–367
Benatar MJ, Dassonville O, Chamorey E et al (2013) Impact of preoperative radiotherapy on head and neck free flap reconstruction: a report on 429 cases. J Plast Reconstr Aesthet Surg 66:478–482
Binahmed A, Nason RW, Hussain A et al (2008) Treatment outcomes in squamous cell carcinoma of the maxillary alveolus and palate: a population-based study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105:750–754
Browne JD, Butler S, Rees C (2011) Functional outcomes and suitability of the temporalis myofascial flap for palatal and maxillary reconstruction after oncologic resection. Laryngoscope 121:1149–1159
Ahmed Djae K, Li Z, Li ZB (2011) Temporalis muscle flap for immediate reconstruction of maxillary defects: review of 39 cases. Int J Oral Maxillofac Surg 40:715–721
Abubaker AO, Abouzgia MB (2002) The temporalis muscle flap in reconstruction of intraoral defects: an appraisal of the technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94:24–30
Clauser L, Curioni C, Spanio S (1995) The use of the temporalis muscle flap in facial and craniofacial reconstructive surgery. A review of 182 cases. J Craniomaxillofac Surg 23:203–214
Rapidis AD, Day TA (2006) The use of temporal polyethylene implant after temporalis myofascial flap transposition: clinical and radiographic results from its use in 21 patients. J Oral Maxillofac Surg 64:12–22
Baj A, Spotti S, Marelli S et al (2009) Use of porous polyethylene for correcting defects of temporal region following transposition of temporalis myofascial flap. Acta Otorhinolaryngol Ital 29:265–269
Lesavoy MA, Lee GK, Fan K et al (2012) Split, temporalis muscle flap for repair of recalcitrant cerebrospinal fluid leaks of the anterior cranial fossa. J Craniofac Surg 23:539–542
Acknowledgments
This work was financially supported by National Natural Science Foundation of China (grant no. 81100737), Natural Science Foundation of Jiangsu Province (grant no. BK2011762), Specialized Research Fund for the Doctoral Program of Higher Education (grant no. 20113234120003), and A Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions (grant no. 2011-137).
Conflict of interest
The authors declare no financial interests regarding this work.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yanling Wang and Jie Cheng contributed equally to this article.
Rights and permissions
About this article
Cite this article
Wang, Y., Cheng, J., Yuan, C. et al. Reconstruction of palatomaxillary defects following cancer ablation with temporalis muscle flap in medically compromised patients: a 15-year single institutional experience. Clin Oral Invest 18, 1663–1670 (2014). https://doi.org/10.1007/s00784-013-1135-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-013-1135-8