Abstract
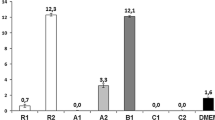
The aim of the present in vitro study was to evaluate the influence of different bone substitute materials (BSM) on the viability of human primary osteoblasts (PO), bone marrow mesenchymal cells (BMMC), and nonadherent myelomonocytic cells (U937). Six different bone substitute materials were tested: Bio-Oss Spongiosa® (BOS), Tutodent Chips® (TC), PepGen P-15® (P-15), Ostim® (OM), BioBase® (BB), and Cerasorb® (CER). Cells were cultivated on comparable volumes of BSM in 96-well plates. Cell culture-treated polystyrol (Nunclon Delta surface; C) served as positive control. After 2 h and 3, 6, 10, and 14 days, viability of cells was evaluated using a standardized ATP viability assay (CellTiter Glo®). Nonsurface-dependent effects of the materials were separately tested using nonadherent U937 suspension cells. For statistical analysis, the Mann–Whitney test was used. Results were considered statistically significant at P < 0.05. Cell viability of PO increased significantly on TC, C, and CER followed by BB. No changes were found for P-15 and decreasing viability for BOS and OM. BMMC showed similar results on C, TC, CER, and P-15. Lower viability for BB and no viability could be detected for BOS and OM (Mann–Whitney test, respectively). Nonadherent cells displayed increasing viability in presence of CER, BB, and BOS. No changes were observed for TC and P-15, whereas for OM, no viability was detected after a maximum cultivation period of 3 days. It was concluded that granular hydroxyapatite (HA; TC, BOS, P-15) and α- and β-tricalciumphosphate (CER, BB) support, whereas nanosized HA (OM) limit or even inhibit surface- and nonsurface-related cell viability in the in vitro model used.




Similar content being viewed by others
References
Acil Y, Springer IN, Broek V, Terheyden H, Jepsen S (2002) Effects of bone morphogenetic protein-7 stimulation on osteoblasts cultured on different biomaterials. J Cell Biochem 86:90–98
Araujo MG, Sonohara M, Hayacibara R, Cardaropoli G, Lindhe J (2002) Lateral ridge augmentation by the use of grafts comprised of autologous bone or a biomaterial. An experiment in the dog. J Clin Periodontol 29:1122–1131
Aybar B, Bilir A, Akcakaya H, Ceyhan T (2004) Effects of tricalcium phosphate bone graft materials on primary cultures of osteoblast cells in vitro. Clin Oral Implants Res 15:119–125
Berger TG, Feuerstein B, Strasser E, Hirsch U, Schreiner D, Schuler G, Schuler-Thurner B (2002) Large-scale generation of mature monocyte-derived dendritic cells for clinical application in cell factories. J Immunol Methods 268:131–140
Betz RR (2002) Limitations of autograft and allograft: new synthetic solutions. Orthopedics 25:s561–570
Blottiere HM, Daculsi G, Anegon I, Pouezat JA, Nelson PN, Passuti N (1995) Utilization of activated U937 monocytic cells as a model to evaluate biocompatibility and biodegradation of synthetic calcium phosphate. Biomaterials 16:497–503
Busenlechner D, Tangl S, Mair B, Fugger G, Gruber R, Redl H, Watzek G (2008) Simultaneous in vivo comparison of bone substitutes in a guided bone regeneration model. Biomaterials 29:3195–3200
Chiriac G, Herten M, Schwarz F, Rothamel D, Becker J (2005) Autogenous bone chips: influence of a new piezoelectric device (Piezosurgery) on chip morphology, cell viability and differentiation. J Clin Periodontol 32:994–999
Cimpan MR, Cressey LI, Skaug N, Halstensen A, Lie SA, Gjertsen BT, Matre R (2000) Patterns of cell death induced by eluates from denture base acrylic resins in U-937 human monoblastoid cells. Eur J Oral Sci 108:59–69
Clavero J, Lundgren S (2003) Ramus or chin grafts for maxillary sinus inlay and local onlay augmentation: comparison of donor site morbidity and complications. Clin Implant Dent Relat Res 5:154–160
Cornell CN (1999) Osteoconductive materials and their role as substitutes for autogenous bone grafts. Orthop Clin North Am 30:591–598
Deligianni D, Korovessis P, Porte-Derrieu MC, Amedee J (2005) Fibronectin preadsorbed on hydroxyapatite together with rough surface structure increases osteoblasts’ adhesion “in vitro”: the theoretical usefulness of fibronectin preadsorption on hydroxyapatite to increase permanent stability and longevity in spine implants. J Spinal Disord Tech 18:257–262
Deligianni DD, Katsala ND, Koutsoukos PG, Missirlis YF (2001) Effect of surface roughness of hydroxyapatite on human bone marrow cell adhesion, proliferation, differentiation and detachment strength. Biomaterials 22:87–96
Huber FX, Belyaev O, Hillmeier J, Kock HJ, Huber C, Meeder PJ, Berger I (2006) First histological observations on the incorporation of a novel nanocrystalline hydroxyapatite paste OSTIM in human cancellous bone. BMC Musculoskelet Disord 7:50
Hurzeler MB, Kirsch A, Ackermann KL, Quinones CR (1996) Reconstruction of the severely resorbed maxilla with dental implants in the augmented maxillary sinus: a 5-year clinical investigation. Int J Oral Maxillofac Implants 11:466–475
Khan SN, Cammisa FP Jr., Sandhu HS, Diwan AD, Girardi FP, Lane JM (2005) The biology of bone grafting. J Am Acad Orthop Surg 13:77–86
Kogler G, Capdeville AB, Hauch M, Bruster HT, Gobel U, Wernet P, Burdach S (1990) High efficiency of a new immunological magnetic cell sorting method for T cell depletion of human bone marrow. Bone Marrow Transplant 6:163–168
Kubler A, Neugebauer J, Oh JH, Scheer M, Zoller JE (2004) Growth and proliferation of human osteoblasts on different bone graft substitutes: an in vitro study. Implant Dent 13:171–179
Logeart-Avramoglou D, Anagnostou F, Bizios R, Petite H (2005) Engineering bone: challenges and obstacles. J Cell Mol Med 9:72–84
Mayr-Wohlfart U, Fiedler J, Gunther KP, Puhl W, Kessler S (2001) Proliferation and differentiation rates of a human osteoblast-like cell line (SaOS-2) in contact with different bone substitute materials. J Biomed Mater Res 57:132–139
Nkenke E, Radespiel-Troger M, Wiltfang J, Schultze-Mosgau S, Winkler G, Neukam FW (2002) Morbidity of harvesting of retromolar bone grafts: a prospective study. Clin Oral Implants Res 13:514–521
Oreffo RO, Kusec V, Romberg S, Triffitt JT (1999) Human bone marrow osteoprogenitors express estrogen receptor-alpha and bone morphogenetic proteins 2 and 4 mRNA during osteoblastic differentiation. J Cell Biochem 75:382–392
Ortega-Munoz M, Morales-Sanfrutos J, Perez-Balderas F, Hernandez-Mateo F, Giron-Gonzalez MD, Sevillano-Tripero N, Salto-Gonzalez R, Santoyo-Gonzalez F (2007) Click multivalent neoglycoconjugates as synthetic activators in cell adhesion and stimulation of monocyte/machrophage cell lines. Org Biomol Chem 5:2291–2301
Piattelli M, Favero GA, Scarano A, Orsini G, Piattelli A (1999) Bone reactions to anorganic bovine bone (Bio-Oss) used in sinus augmentation procedures: a histologic long-term report of 20 cases in humans. Int J Oral Maxillofac Implants 14:835–840
Rothamel D, Schwarz F, Herten M, Engelhardt E, Donath K, Kuehn P, Becker J (2008) Dimensional ridge alterations following socket preservation using a nanocrystalline hydroxyapatite paste. A histomorphometrical study in dogs. J Oral Maxillofac Surg 37: 741–747
Schlegel KA, Fichtner G, Schultze-Mosgau S, Wiltfang J (2003) Histologic findings in sinus augmentation with autogenous bone chips versus a bovine bone substitute. Int J Oral Maxiofac Implants 18:53–58
Seibel MJ (2000) Molecular markers of bone turnover: biochemical, technical and analytical aspects. Osteoporos Int 11:18–29
Stockbauer P, Malaskova V, Soucek J, Chudomel V (1983) Differentiation of human myeloid leukemia cell lines induced by tumor-promoting phorbol ester (TPA). I. Changes of the morphology, cytochemistry and the surface differentiation antigens analyzed with monoclonal antibodies. Neoplasma 30:257–272
Strietzel FP, Reichart PA, Graf HL (2007) Lateral alveolar ridge augmentation using a synthetic nano-crystalline hydroxyapatite bone substitution material (Ostim): preliminary clinical and histological results. Clin Oral Implants Res 18:743–751
Trentz OA, Platz A, Helmy N, Trentz O (1998) Response of osteoblast cultures to titanium, steel and hydroxyapatite implants. Swiss Surg 203–209
Van Belle H (1972) Kinetics and inhibition of alkaline phosphatases from canine tissues. Biochim Biophys Acta 289:158–168
Wiedmann-Al-Ahmad M, Gutwald R, Gellrich NC, Hubner U, Schmelzeisen R (2005) Search for ideal biomaterials to cultivate human osteoblast-like cells for reconstructive surgery. J Mater Sci Mater Med 16:57–66
Yildirim M, Spiekermann H, Handt S, Edelhoff D (2001) Maxillary sinus augmentation with the xenograft Bio-Oss and autogenous intraoral bone for qualitative improvement of the implant site: a histologic and histomorphometric clinical study in humans. Int J Oral Maxillofac Implants 16:23–33
Zijderveld SA, Zerbo IR, van den Bergh JP, Schulten EA, ten Bruggenkate CM (2005) Maxillary sinus floor augmentation using a beta-tricalcium phosphate (Cerasorb) alone compared to autogenous bone grafts. Int J Oral Maxillofac Implants 20:432–440
Acknowledgements
We would like to thank Ms. Brigitte Hartig (Department of Oral Surgery) for her excellent technical expertise and Dr. J. Fischer (Institute for Transplantation Diagnostics and Cell Therapeutics, Heinrich Heine University) for harvesting the bone marrow.
Disclosure
The authors are grateful to Biovision GmbH Ilmenau Germany, Curasan AG Kleinostheim Germany, Dentsply Friadent Mannheim Germany, Geistlich Biomaterials Wolhusen Switzerland, Heraeus Kulzer Hanau Germany, and Tutogen Medical Neunkirchen Germany for kindly providing the BSM for this study. All authors claim to have no financial interest in any company or any of the products mentioned in this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Herten, M., Rothamel, D., Schwarz, F. et al. Surface- and nonsurface-dependent in vitro effects of bone substitutes on cell viability. Clin Oral Invest 13, 149–155 (2009). https://doi.org/10.1007/s00784-008-0214-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-008-0214-8