Abstract
Background
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used in clinical situations to reduce inflammation and pain. Percutaneous administration is one of the routes mainly used in Japan to deal with the pain from acute injuries, to chronic pain such as chronic low back pain and osteoarthritis (OA). There have been no studies that report the effect of percutaneous administration of NSAIDs on chronic pain in animal models. This study aimed to investigate the effect of percutaneously absorbed NSAIDs on a rodent model of OA.
Methods
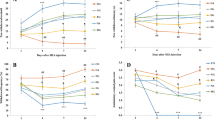
OA was induced with an intra-articular injection of monoiodoacetate into the right knees (left knee was treated with saline, normal control) of female Sprague-Dawley rats. Physical evaluation, diameter, and the range of motion (ROM) of the knee joint, as well as pain-related behavior, were evaluated. Animals were killed and perfused 7 days after the intra-articular injection, and then local tissue from the knee [for cytokine assay: tumor necrosis factor (TNF)-α, interleukin (IL)-6, and nerve growth factor (NGF)] and spinal cord (immunostained for c-Fos protein reflecting neuronal excitation) were evaluated (n = 7 each). Twenty-eight days after the injection, the other rats were then divided into three groups and were identified by a plaster tape containing an NSAID or a vehicle applied to their OA (ipsilateral) knees: a vehicle-treated group, a loxoprofen-treated (lox) group, and a ketoprofen-treated (ket) group. The behavior elicited by von Frey hairs, inflammatory cytokines, and c-Fos protein at 0, 8, and 24 h after tape application were evaluated (n = 7 each). The plaster tapes contained corresponding NSAIDs used in clinical settings: lox 2.8 mg and ket 1.1 mg. Three of the OA animals were histologically evaluated.
Results
As the OA progressed, the ipsilateral knee joint showed OA-like appearance physically and histologically. The knee diameter increased and ROM decreased significantly (P < 0.05), showing histological OA-like cartilage degeneration. Pain threshold decreased significantly according to OA progression (P < 0.05). NSAID application significantly improved the threshold 24 h after application in both the lox and ket groups (P < 0.05) without any significant difference between groups. Cytokine concentrations and c-Fos were significantly suppressed in both lox and ket groups (P < 0.05). Lox suppressed TNF-α and NGF more than ket, whereas ket suppressed IL-6 more.
Conclusion
Suppression of proinflammatory cytokines and c-Fos expression by clinically used NSAIDs suggests that their percutaneous administration may have an analgesic effect for treating chronic pain at a molecular level.




Similar content being viewed by others
References
Sekiguchi M, Shirasaka M, Konno S, Kikuchi S. Analgesic effect of percutaneously absorbed non-steroidal anti-inflammatory drugs: an experimental study in a rat acute inflammation model. BMC Musculoskelet Dis. 2008;9:1–7.
Guingamp C, Gegout-Pottie P, Philippe L, Terlain B, Netter P, Gillet P. Mono-iodoacetate-induced experimental osteoarthritis: a dose–response study of loss of mobility, morphology, and biochemistry. Arthritis Rheum. 1997;40:1670–9.
Guzman RE, Evans MG, Bove S, Morenko B, Kilgore K. Mono-iodoacetate-induced histologic changes in subchondral bone and articular cartilage of rat femorotibial joints: an animal model of osteoarthritis. Toxicol Pathol. 2003;31:619–24.
Bove SE, Calcaterra SL, Brooker RM, Huber CM, Guzman RE, Juneau PL, Schrier DJ, Kilgore KS. Weight bearing as a measure of disease progression and efficacy of anti-inflammatory compounds in a model of monosodium iodoacetate-induced osteoarthritis. Osteoarthritis Cartilage. 2003;11:821–30.
Smith MD, Triantafillou S, Parker A, Youssef PP, Coleman M. Synovial membrane inflammation and cytokine production in patients with early osteoarthritis. J Rheumatol. 1997;24:365–71.
Orita S, Ishikawa T, Miyagi M, Ochiai N, Inoue G, Eguchi Y, Kamoda H, Arai G, Toyone T, Aoki Y, Kubo T, Takahashi K, Ohtori S. Pain-related sensory innervation in monoiodoacetate-induced osteoarthritis in rat knees that gradually develops neuronal injury in addition to inflammatory pain. BMC Musculoskelet Disord. 2011;12:134.
Hunt SP, Pini A, Evan G. Induction of c-fos-like protein in spinal cord neurons following sensory stimulation. Nature. 1987;328:632–4.
Menétrey D, Gannon A, Levine JD, Basbaum AI. Expression of c-fos protein in interneurons and projection neurons of the rat spinal cord in response to noxious somatic, articular, and visceral stimulation. J Comp Neurol. 1989;285:177–95.
Morgan JI, Curran T. Stimulus-transcription coupling in the nervous system: involvement of the inducible proto-oncogenes fos and jun. Annu Rev Neurosci. 1991;14:421–51.
Chimoto E, Hagiwara Y, Ando A, Itoi E. Progression of an arthrogenic motion restriction after immobilization in a rat experimental knee model animals. Ups J Med Sci. 2007;112:347–55.
Janusz MJ, Bendele AM, Brown KK, Taiwo YO, Hsieh L, Heitmeyer SA. Induction of osteoarthritis in the rat by surgical tear of the meniscus: inhibition of joint damage by a matrix metalloproteinase inhibitor. Osteoarthritis Cartilage. 2002;10:785–91.
Schaible HG. Neurophysiology of nociception and pain reactions in inflammatory joint diseases. Rev Rhum Engl Ed. 1997;64:144S–5S.
Kunkel SL, Wiggins RC, Chensue SW, Larrick J. Regulation of macrophage tumor necrosis factor production by prostaglandin E2. Biochem Biophys Res Commun. 1986;137:404–10.
Tipton DA, Gay DC, DeCoster VA. Effect of a cyclooxygenase-2 inhibitor on interleukin-1beta-stimulated activation of the transcription factor nuclear factor-kappa B in human gingival fibroblasts. J Periodontol. 2007;78:542–9.
Kutuk O, Basaga H. Aspirin inhibits TNFalpha- and IL-1-induced NF-kappaB activation and sensitizes HeLa cells to apoptosis. Cytokine. 2004;25:229–37.
Ohtori S, Takahashi K, Moriya H, Myers RR. TNF-alpha and TNF-alpha receptor type 1 upregulation in glia and neurons after peripheral nerve injury: studies in murine DRG and spinal cord. Spine. 2004;29:1082–8.
Pollock J, McFarlane SM, Connell MC, Zehavi U, Vandenabeele P, MacEwan DJ, Scott RH. TNF-alpha receptors simultaneously activate Ca2+ mobilisation and stress kinases in cultured sensory neurones. Neuropharmacol. 2002;42:93–106.
Orita S, Koshi T, Mitsuka T, Miyagi M, Inoue G, Arai G, Ishikawa T, Hanaoka E, Yamashita K, Yamashita M, Eguchi Y, Toyone T, Takahashi K, Ohtori S. Associations between proinflammatory cytokines in the synovial fluid and radiographic grading and pain-related scores in 47 consecutive patients with osteoarthritis of the knee. BMC Musculoskelet Dis. 2011;12:144.
Lotz M, Guerne PA. Interleukin-6 induces the synthesis of tissue inhibitor of metalloproteinases-1/erythroid potentiating activity (TIMP-1/EPA). J Biol Chem. 1991;266:2017–20.
Iannone F, Bari CD, Accio FD, Covelli M, Patella V, Bianco GL, Lapadula G. Increased expression of nerve growth factor (NGF) and high affinity NGF receptor (p140 TrkA) in human osteoarthritic chondrocytes. Rheumatology (Oxf). 2002;41:1413–8.
Pezet S, McMahon SB. Neurotrophins: mediators and modulators of pain. Annu Rev Neurosci. 2006;29:507–38.
Manni L, Lundeberg T, Fiorito S, Bonini S, Vigneti E, Aloe L. Nerve growth factor release by human synovial fibroblasts prior to and following exposure to tumor necrosis factor-alpha, interleukin-1 beta and cholecystokinin-8: the possible role of NGF in the inflammatory response. Clin Exp Rheumatol. 2003;21:617–24.
Carter JL, Lubahn C, Lorton D, Osredkar T, Der TC, Schaller J, Evelsizer S, Flowers S, Ruff N, Reese B, Bellinger DL. Adjuvant-induced arthritis induces c-Fos chronically in neurons in the hippocampus. J Neuroimmunol. 2011;230:85–94.
Takayama B, Kikuchi S, Konno S, Sekiguchi M. An immunohistochemical study of the antinociceptive effect of calcitonin in ovariectomized rats. BMC Musculoskelet Dis. 2008;9:164.
Abbadie C, Besson JM. c-fos expression in rat lumbar spinal cord during the development of adjuvant-induced arthritis. Neuroscience. 1992;48:985–93.
Naranjo JR, Mellström B, Achaval M, Sassone-Corsi P. Molecular pathways of pain: Fos/Jun-mediated activation of a noncanonical AP-1 site in the prodynorphin gene. Neuron. 1991;6:607–17.
Carrive P, Meyer-Carrive I. Changes in formalin-evoked spinal Fos expression and nociceptive behaviour after oral administration of Bufferin A (aspirin) and L-5409709 (ibuprofen + caffeine + paracetamol). Pain. 1997;70:253–66.
Honoré P, Buritova J, Besson JM. Carrageenin-evoked c-Fos expression in rat lumbar spinal cord: the effects of indomethacin. Eur J Pharmacol. 1995;272:249–59.
Buritova J, Besson JM. Effects of flurbiprofen and its enantiomers on the spinal c-Fos protein expression induced by noxious heat stimuli in the anaesthetized rat. Eur J Pharmacol. 2000;406:59–67.
Delcroix JD, Valletta JS, Wu C, Hunt SJ, Kowal AS, Mobley WC. NGF signaling in sensory neurons: evidence that early endosomes carry NGF retrograde signals. Neuron. 2003;39:69–84.
Michael GJ, Averill S, Nitkunan A, Rattray M, Bennett DL, Yan Q, Priestley JV. Nerve growth factor treatment increases brain-derived neurotrophic factor selectively in TrkA-expressing dorsal root ganglion cells and in their central terminations within the spinal cord. J Neurosci. 1997;17:8476–90.
Kerr BJ, Bradbury EJ, Bennett DL, Trivedi PM, Dassan P, French J, Shelton DB, McMahon SB, Thompson SW. Brain-derived neurotrophic factor modulates nociceptive sensory inputs and NMDA-evoked responses in the rat spinal cord. J Neurosci. 1999;19:5138–48.
Orita S, Ohtori S, Nagata M, Horii M, Yamashita M, Yamauchi K, Inoue G, Suzuki M, Eguchi Y, Kamoda H, Arai G, Ishikawa T, Miyagi M, Ochiai N, Kishida S, Takaso M, Aoki Y, Takahashi K. Inhibiting nerve growth factor or its receptors downregulates calcitonin gene-related peptide expression in rat lumbar dorsal root ganglia innervating injured intervertebral discs. J Orthop Res. 2010;28:1614–20.
Buritova J, Honoré P, Besson JM. Ketoprofen produces profound inhibition of spinal c-Fos protein expression resulting from an inflammatory stimulus but not from noxious heat. Pain. 1996;67:379–89.
Panfil C, Makowska A, Ellrich J. Brainstem and cervical spinal cord Fos immunoreactivity evoked by nerve growth factor injection into neck muscles in mice. Cephalalgia. 2006;26:128–35.
Sugimoto M, Kojima T, Asami M, Iizuka Y, Matsuda K. Inhibition of prostaglandin production in the inflammatory tissue by loxoprofen-Na, an anti-inflammatory prodrug. Biochem Pharmacol. 1991;42:2363–8.
Ferreira-gomes J, Adães S, Castro-lopes JM. Assessment of movement-evoked pain in osteoarthritis by the knee-bend and catwalk tests: a clinically relevant study. J Pain. 2008;9:945–54.
Acknowledgments
The authors thank Miho Sekiguchi, M.D., Ph.D. (Department of Orthopaedic Surgery, Fukushima School of Medicine, Fukushima, Japan) for technical advice.
Conflict of interest
None of the authors have any conflicts of interest or disclosures in relation to this work.
Author information
Authors and Affiliations
Corresponding author
Additional information
S. Orita, T. Ishikawa, and M. Miyagi equally contributed to this work.
About this article
Cite this article
Orita, S., Ishikawa, T., Miyagi, M. et al. Percutaneously absorbed NSAIDs attenuate local production of proinflammatory cytokines and suppress the expression of c-Fos in the spinal cord of a rodent model of knee osteoarthritis. J Orthop Sci 17, 77–86 (2012). https://doi.org/10.1007/s00776-011-0175-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-011-0175-7