Abstract
Background
If a transverse incision can be safely used for total knee arthroplasty (TKA), decreases in scar formation, reduced injury of the infrapatellar branch of the saphenous nerve and improved kneeling motion will be observed.
Methods
We evaluated 95 patients (101 knees) on whom primary TKA was performed with follow-up of more than 2 years. A longitudinal incision was used for the first 40 knees and a transverse incision for the remaining 61 knees. Operation time, blood loss, complications and Knee Society Score were evaluated. Wound lengths, widths and the Manchester Scar Scale (MSS) were measured 1 year after the surgery. Further examination evaluated sensory disturbances and whether kneeling was possible.
Results
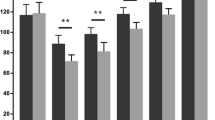
The complication rate in both groups was almost the same. The wound lengths measured at a 90° knee-flexed position were about 15 cm with no significant difference between the groups. The average width measured at a maximum area was significantly smaller in the transverse group than in the longitudinal group. MSS of the transverse group was also significantly lower than that of the longitudinal group. Sensory disturbance was found to be significantly smaller in the transverse group than in the longitudinal group both in subjective and objective evaluation at 1 year after surgery. When a transverse incision was used, the direction of the incision corresponded to the running direction of the saphenous nerve, and thus, we were able to reduce sensory disturbances on the distal lateral side of the knee joint. The transverse group (70.4%) performed significantly better than the longitudinal group (40.6%) at kneeling motion.
Conclusions
We showed that making a transverse incision is a safe method, resulting in a reduction of scar formation and less dysfunction of the infrapatellar branch of the saphenous nerve, and improvement of kneeling motion.




Similar content being viewed by others
References
Johnson DP, Houghton TA, Radford P. Anterior midline or medical parapatellar incision for arthroplasty of the knee. J Bone Joint Surg [Br]. 1986;68-B:812–4.
Sundaram RO, Ramakrishnan M, Harvey RA, Parkinson RW. Comparison of scars and resulting hypoaesthesia between the medial parapatellar and midline skin incisions in total knee arthroplasty. Knee. 2007;14:375–8.
Borley NR, Edwards D, Villar RN. Lateral skin flap numbness after total knee arthroplasty. J Arthroplasty. 1995;10:13–4.
Goldstein WM, Gordon AC, Branson JJ, Simmons C, Berland KA. Stress over the anterior aspect of the knee with kneeling. J Bone Joint Surg [Am]. 2007;89-A(Suppl 3):162–6.
Schai PA, Gibbon AJ, Scott RD. Kneeling ability after total knee Arthroplasty: perception and reality. Clin Orthop Relat Res. 1999;367:195–200.
Scuderi GR. Surgical approaches to the knee. In: Insall JN, editor. Surgery of the knee. 4th ed. New York: Churchill Livingstone; 2005.
Beausang E, Floyd H, Dunn KW, Orton CI, Ferguson WJ. A new quantitative scale for clinical scar assessment. Plast Reconstr Surg. 1998;102:1954–61.
Willhelmi BJ, Blackwell SJ, Phillips LG. Langer’s lines: to use or not to use. Plast Recontr Surg. 1999;104:208–14.
Borges AF. Relaxed skin tension lines (RSTL) versus other skin lines. Plast Recontr Surg. 1984;73:144–50.
Kraissl CJ. The selection of appropriate lines for elective surgical incisions. Plast Recontr Surg. 1951;8:1–29.
Tennent TD, Birch NC, Holmes MJ, Birch R, Goddard NJ. Knee pain and the infrapatellar branch of the saphenous nerve. J R Soc Med. 1998;91:573–5.
Luo H, Yu JK, Ao YF, Yu CL, Peng LB, Lin CY, Zhang JY, Fu X. Relationship between different skin incisions and the injury of the infrapatellar branch of the saphenous nerve during anterior cruciate ligament reconstruction. Chin Med J. 2007;120:1127–30.
Hopton BP, Tommichan MC, Howell FR. Reducing lateral skin flap numbness after total knee arthroplasty. Knee. 2004;11:289–91.
Hassaballa MA, Porteous AJ, Newman JH. Observed kneeling ability after total, unicompartmental and patellofemoral knee arthroplasty: perception versus reality. Knee Surg Sports Traumatol Arthrosc. 2004;12:136–9.
Unnanamana A. Press-fit-condylar total knee replacement: experience in 165 Thai patients. J Med Assoc Thai. 1997;80–9:565–9.
Sharrad WJ. Pressure effects on the knee in kneeling miners. In: Proceedings of Annual meeting. England RCS. 1964;309–24.
Younger ASE, Duncan CP, Masri BA. Surgical exposures in revision total knee arthroplasty. J Am Acad Orthop Surg. 1998;6:55–64.
Vince KG, Chivas D, Droll KP. Wound problems in total knee arthroplasty. J Arthroplasty. 2007;22:39–44.
Acknowledgments
We are deeply grateful to Dr. Nobuyuki Yoshino at Kyoto Kujo Hospital for valuable advices. I am also greatly indebted to all the people who gave me support and cooperation during this study, especially those at Yatsuo General Hospital, Harue Hospital and Fukui General Hospital.
Conflict of interest
None of the authors of this manuscript have received any benefits or funding from anything related directly or indirectly to this article.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ojima, T., Yoshimura, M., Katsuo, Si. et al. Transverse incision advantages for total knee arthroplasty. J Orthop Sci 16, 524–530 (2011). https://doi.org/10.1007/s00776-011-0133-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-011-0133-4